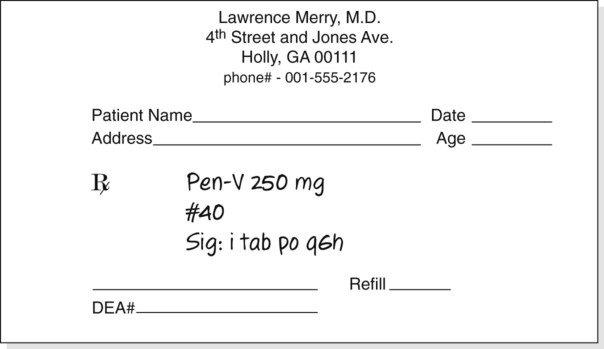
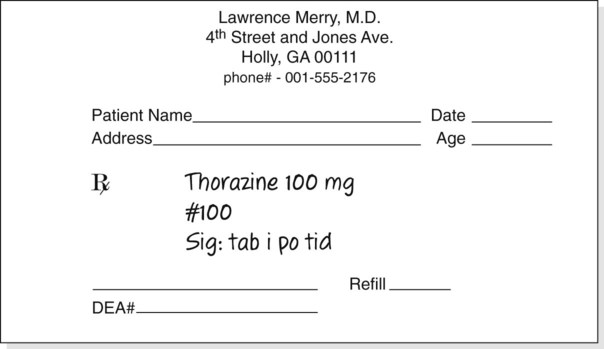
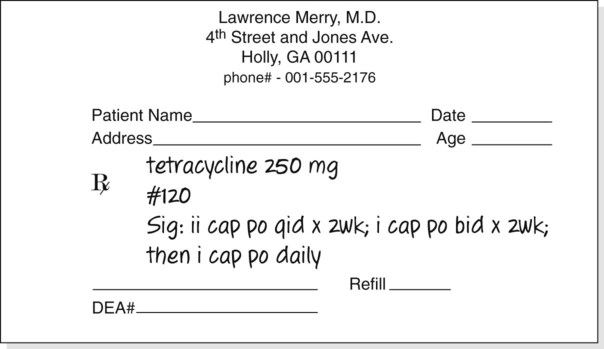
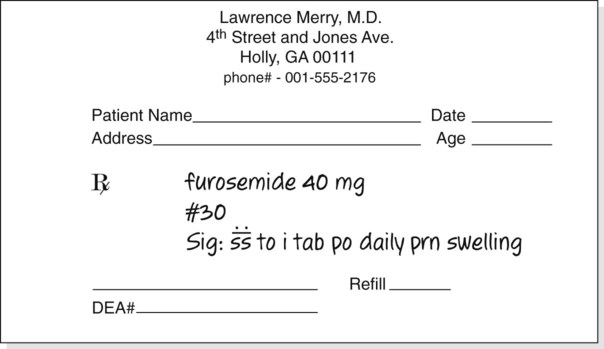
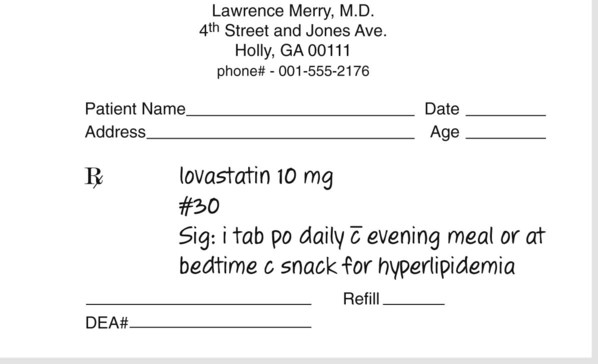
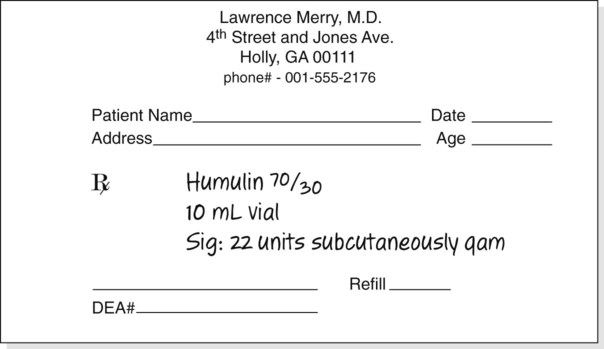
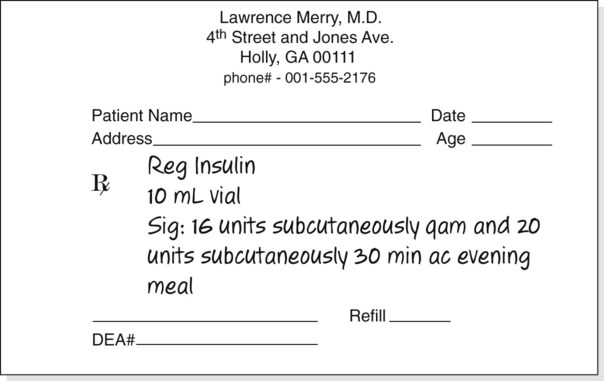
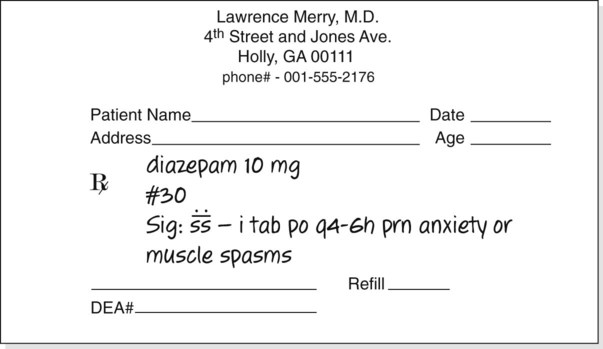
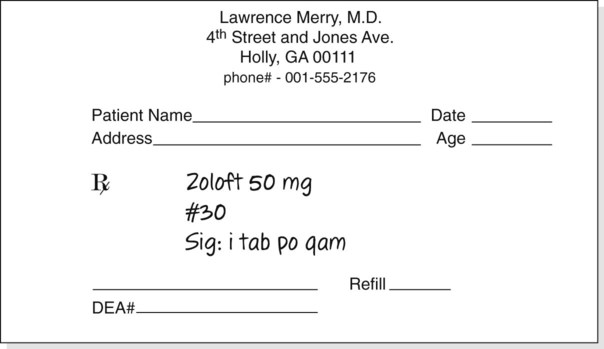
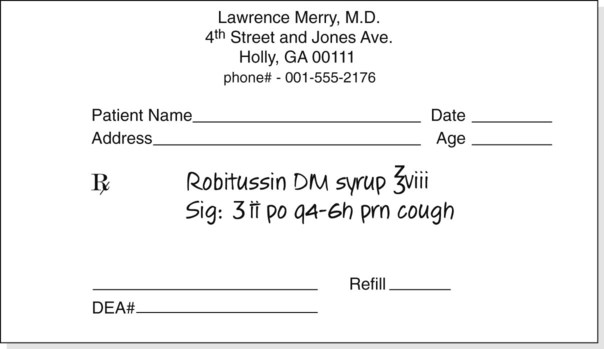
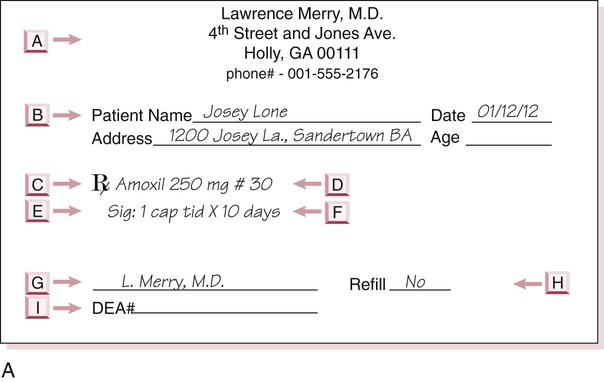
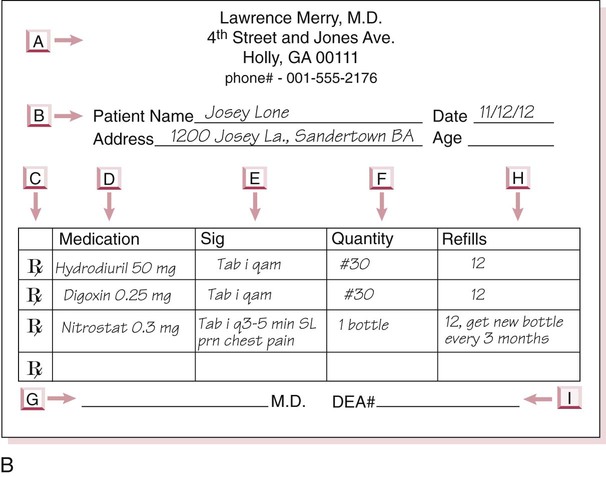
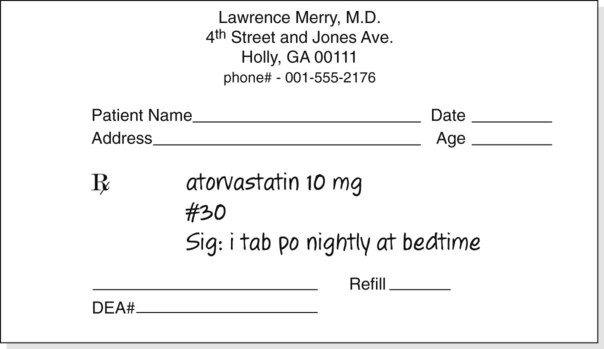
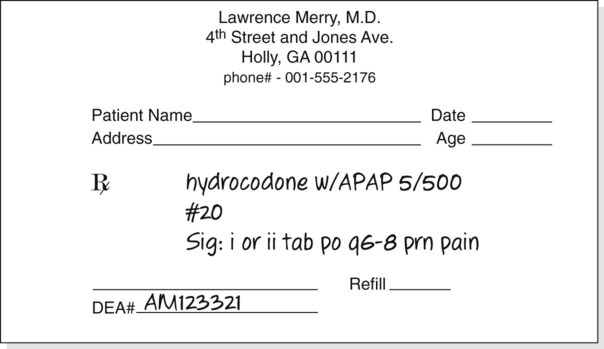
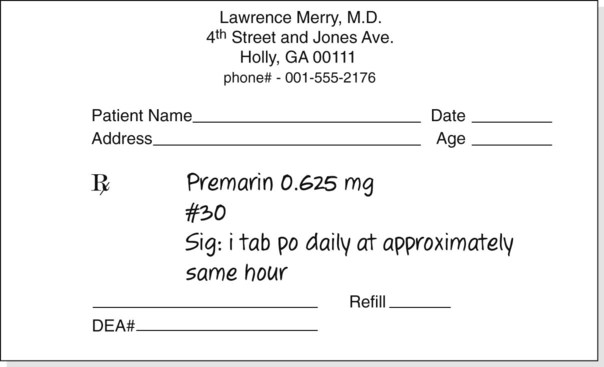
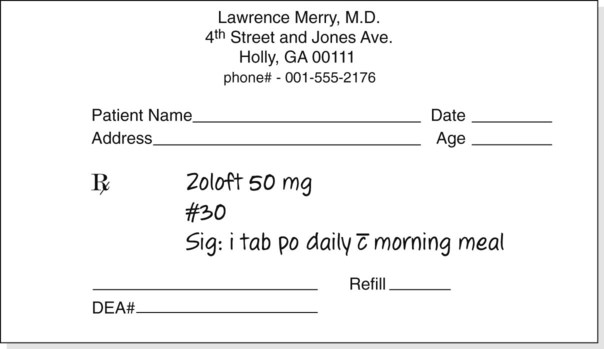
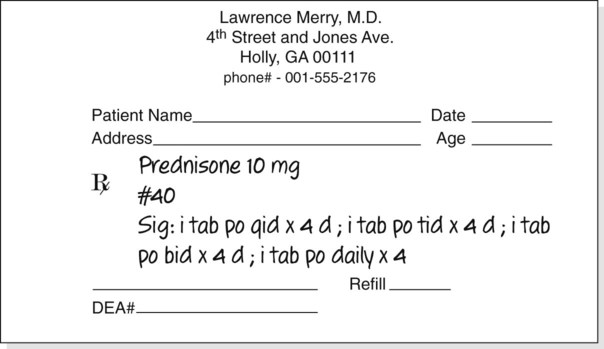
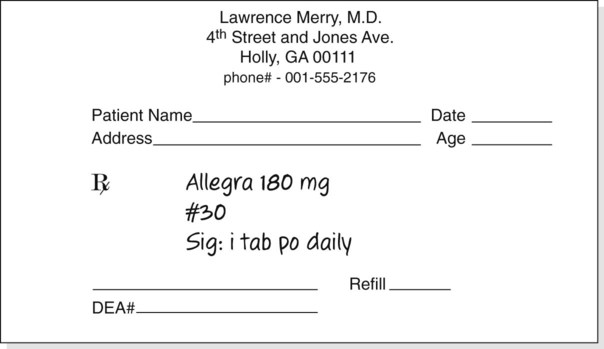
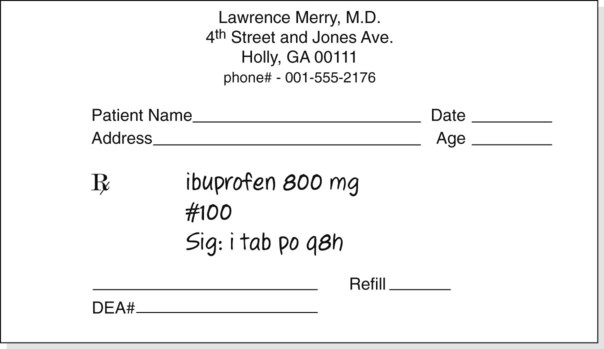
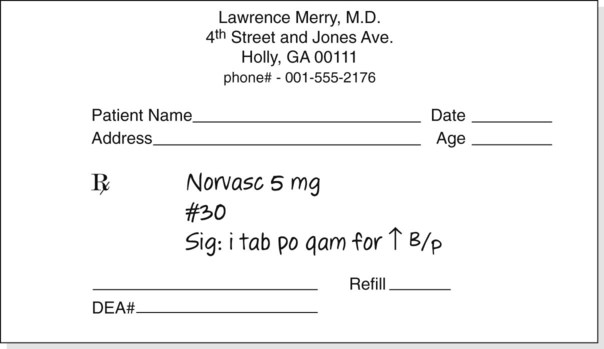
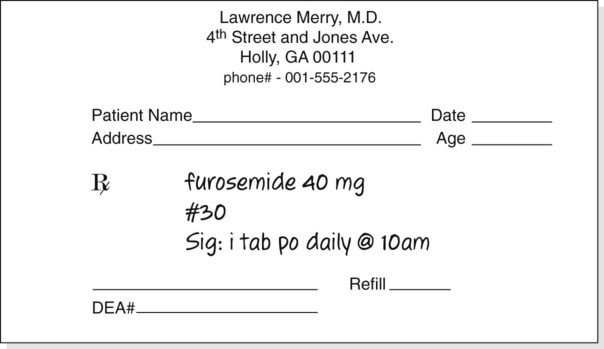
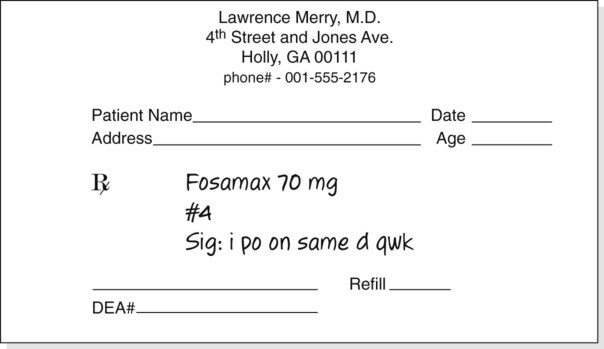
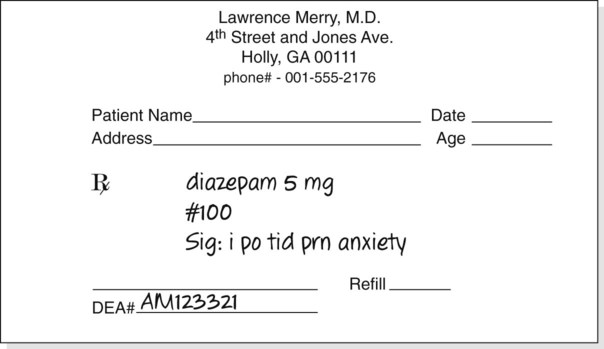
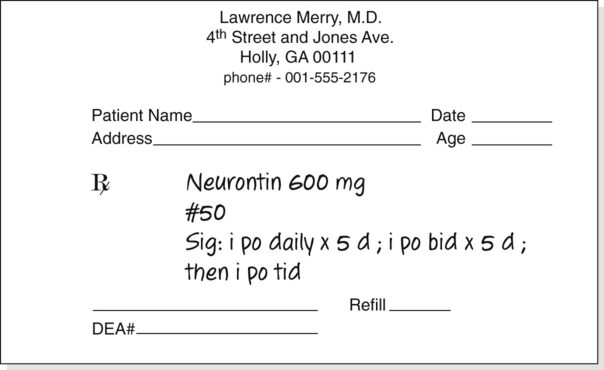
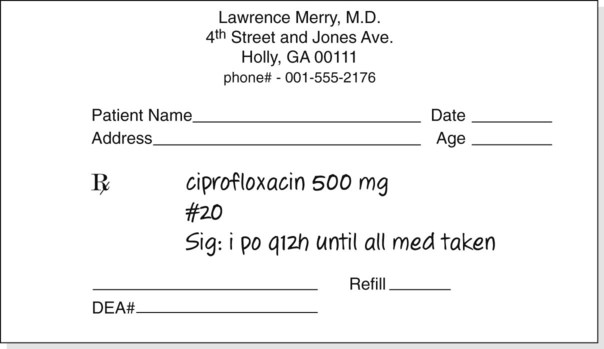
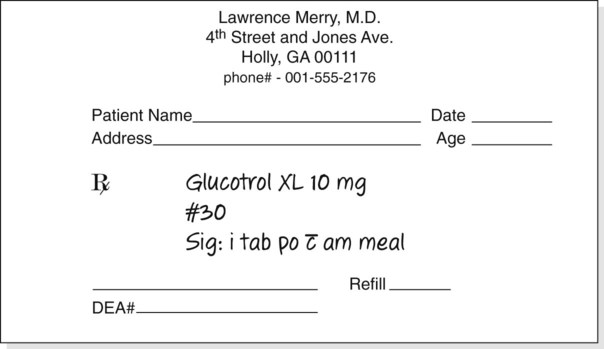
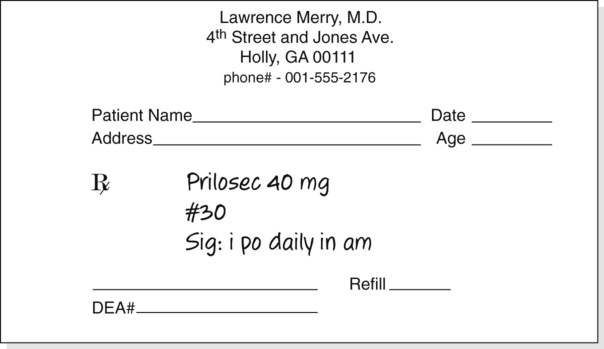
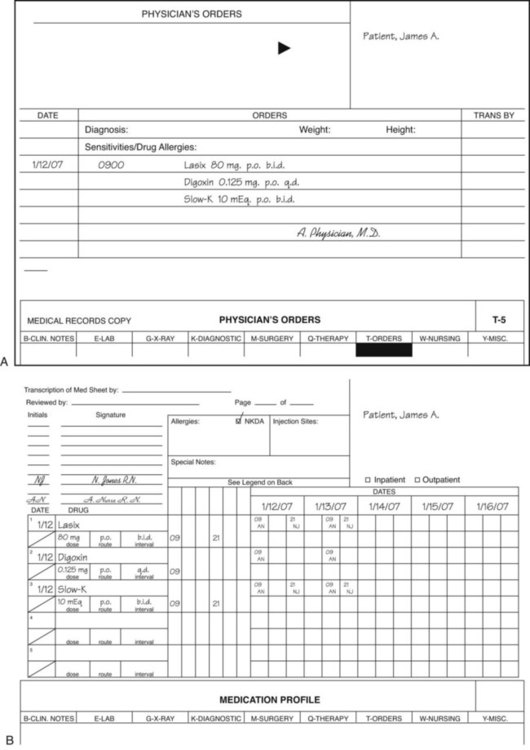
Chapter 6 • Describe components of a prescription • Interpret prescriptions and medication orders • Interpret labels found on medication containers • Use and understand units of measurement found in pharmacology Figure 6-1 provides short descriptions of the parts of a prescription. The five major components are the superscription, inscription, signa (Sig), subscription and signature of the health care professional. Line A of Figure 6-1 is the preprinted name of the physician or group of physicians, the address, and phone number. Line B includes the patient’s name, address, date of the prescription, and the patient’s age if the patient is a child. Dating the prescription is important because prescriptions must be filled within 12 months of writing except with controlled substances or scheduled medications, and the refilling of prescriptions is dependent on the date. Line C is the superscription or the symbol Abbreviations are often used in the writing of prescriptions. Only standard abbreviations should be used. Remember that a prescription is a legal document that could appear in a court case. In those instances, “local” or nonstandard abbreviations might become an area of concern for possible misinterpretation. Abbreviations are actually medical shorthand that is used to write clear and concise orders that will be used among health care professionals. For orders to be correctly written and interpreted, the health care professional and the person dispensing the medication must understand the meaning of each abbreviation used. For commonly accepted abbreviations, see the table on the inside front cover and Chapter 1. A medication order is a method of providing the same information as found on a prescription given to the patient, but is used in an inpatient or physician’s office environment (Figure 6-2). An exception with the medication order is that the order is written for either the number of doses or for the specific length of time for the medicine to be taken. With the medication order, the health care professional is told what drug or drugs should be administered, the strength of the medication, and the frequency to be taken. This order is a means of providing drugs at correct frequency in an inpatient setting. The medication order has six parts: date; patient name, which may appear on the patient record; medication name; dose or medication strength/form; route, time, and frequency of administration; and signature of the prescribing professional. Medication orders may be verbally communicated, but for legal purposes, each order should be transcribed onto a written form by the health care professional who accepts the order and the order must be countersigned by the health care professional who communicated the order and is licensed to prescribe medications in the state of practice.
Interpretation of Medication Labels and Orders
What Does a Prescription Indicate?
 , meaning “recipe” or “take thou,” from Latin. The inscription, which specifies the name of the medication, its strength, and quantity of drug to be dispensed, appears on line D. If the medication must be compounded or prepared, the ingredients would appear in this location. Line E is the “Sig,” or signa, giving directions for taking the medication. The subscription, line F, tells the pharmacist the drug form, as well as how the medication is be taken. The physician’s signature appears on line G, and the number of allowed refills on Line H. Finally, if the prescription is for a controlled medication, the physician must place his or her U. S. Drug Enforcement Administration (DEA) number either under or beside the signature.
, meaning “recipe” or “take thou,” from Latin. The inscription, which specifies the name of the medication, its strength, and quantity of drug to be dispensed, appears on line D. If the medication must be compounded or prepared, the ingredients would appear in this location. Line E is the “Sig,” or signa, giving directions for taking the medication. The subscription, line F, tells the pharmacist the drug form, as well as how the medication is be taken. The physician’s signature appears on line G, and the number of allowed refills on Line H. Finally, if the prescription is for a controlled medication, the physician must place his or her U. S. Drug Enforcement Administration (DEA) number either under or beside the signature.
What Is a Medication Order?
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




 po q4h prn itching
po q4h prn itching