chapter 18 Integration of metabolism in the whole body
 Metabolism needs to be integrated and controlled to prevent ‘futile cycling’ and allow the body to respond to changes.
Metabolism needs to be integrated and controlled to prevent ‘futile cycling’ and allow the body to respond to changes. The hormones insulin and glucagon are responsible for controlling metabolism to maintain an appropriate blood glucose concentration.
The hormones insulin and glucagon are responsible for controlling metabolism to maintain an appropriate blood glucose concentration.The need for coordination
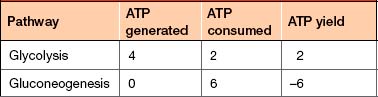
• Prevent ‘futile cycling’—often the energy gained from a catabolic pathway is less than that required by the opposing anabolic pathway (Table 18-1) so the uncontrolled breakdown and re-synthesis of substrates must be prevented.
• Respond to changes in need—the physiological environment of cells and organs will change over time as nutrients are absorbed or energy stores are consumed.
• Organs are metabolically diverse—cells, tissues and organs have different metabolic capabilities and needs.
Balancing blood glucose
The pancreas
The pancreas is a secretory organ that lies posterior to the stomach (Fig 18-1) and contains both an exocrine portion, which secretes digestive enzymes, and an endocrine portion, known as islets of Langerhans, which secrete insulin, glucagon and other hormones. The exocrine portion is made up of groups of cells known as acini. Digestive enzymes are secreted into the pancreatic duct, which empties into the gastrointestinal tract (Table 15-2). These enzymes catalyse the catabolism of carbohydrates, lipids and proteins.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree