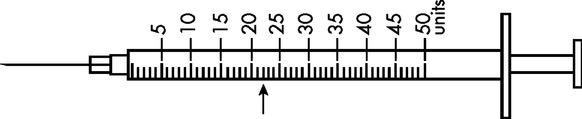
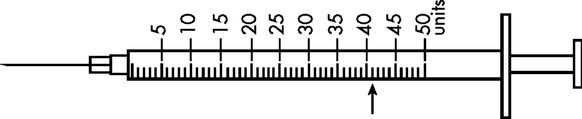
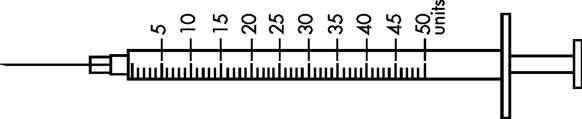
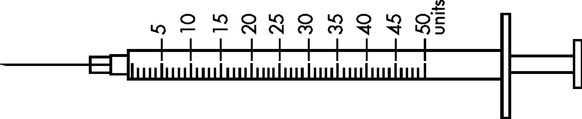
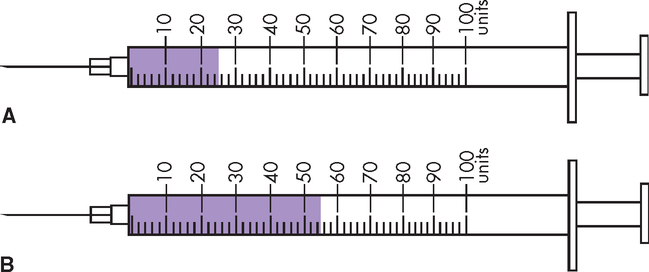
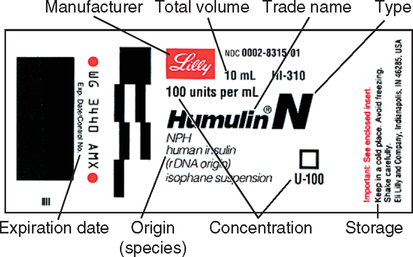
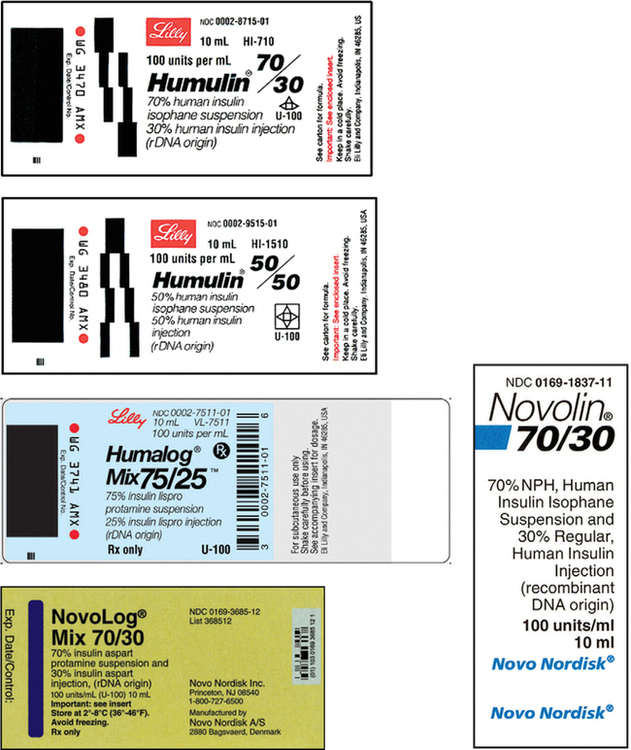
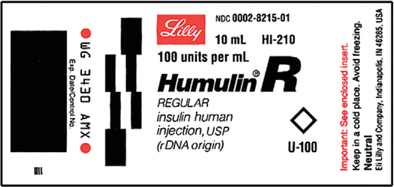
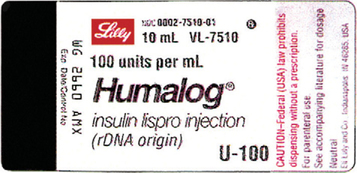
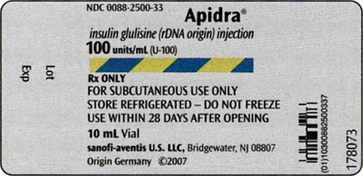
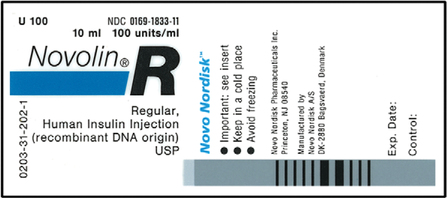
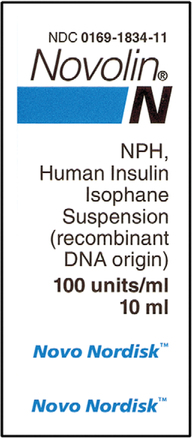
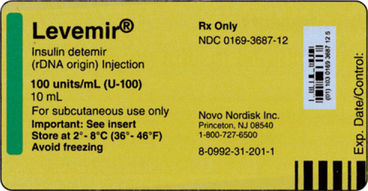
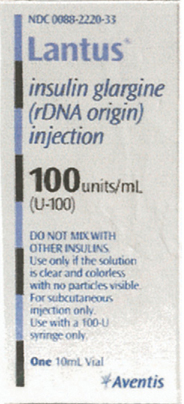
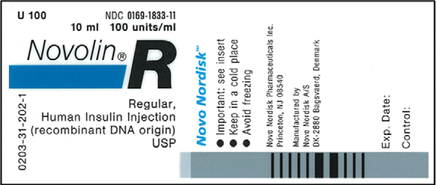
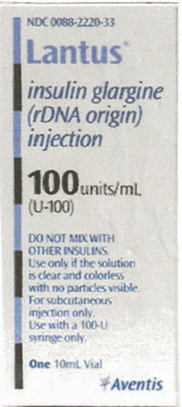
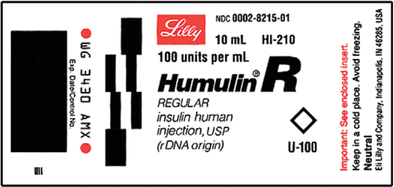
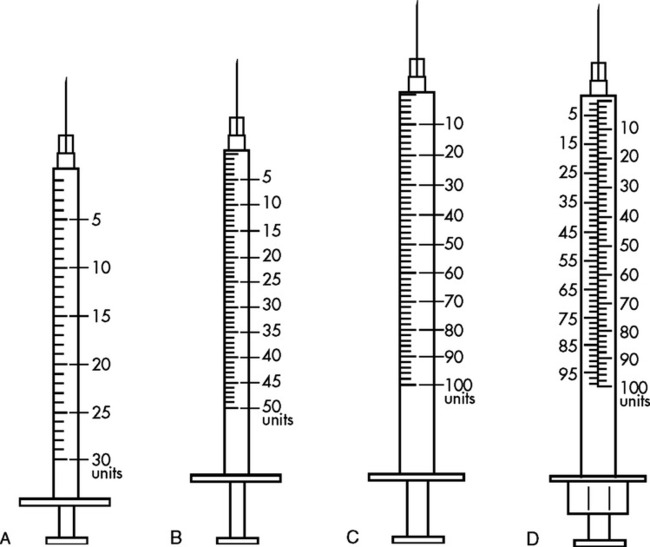
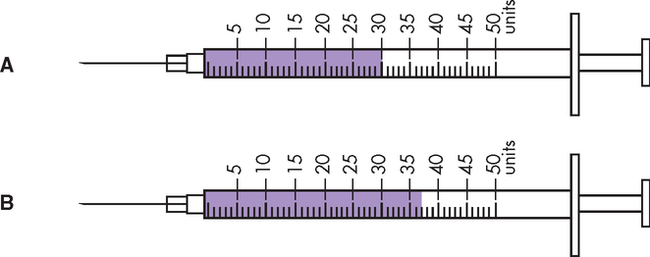
CHAPTER 20 After reviewing this chapter, you should be able to: 1. Identify important information on insulin labels 2. Read calibrations on 30-, 50-, and 100-unit syringes 3. Measure insulin in single dosages • Incorrect rates being programmed into infusion pumps • Incorrect concentrations of insulin used to prepare a dose • Use of tuberculin syringe to prepare a dose, which has resulted in tenfold overdoses • Look-alike names and packaging • Miscommunication of insulin orders • “U” used as an abbreviation for units in orders, resulting in the “U” being misinterpreted as a zero (0) or a number This is just a sample of the causes of errors with insulin and has serious implications for nurses. The only insulin on the market today is recombinant DNA insulin because it causes fewer reactions than insulin from animal sources. It is essential that the nurse knows where to locate this information. When an insulin order is written, the label will specify the origin of the insulin. Also found on the label is the type of insulin. This is indicated by a letter that follows the trade name. (Figure 20-1 shows information that can be found on an insulin label.) The letters that follow the trade name on insulin labels (e.g., Humulin R, Humulin N) identify the type of insulin by action and time (see Figure 20-1). Nurses must be familiar with the onset, peak, and duration of action, which vary depending on the type of insulin. There are three basic action types of insulins: rapid acting (regular, lispro [Humalog], aspart [NovoLog], glulisine [Apidra]); intermediate acting (NPH); and long acting (glargine [Lantus], detemir [Levemir]). The expiration date and concentration are also indicated on the label and are important to check. Notice the uppercase letters on all insulin labels, for example, N for NPH as in Figure 20-1. You will see R for regular insulin. Regular and NPH are the two types of insulin used most often. Look at the Humulin insulin label in Figure 20-1. Notice that the label shows Humulin (trade name), followed by the letter N. N = NPH (intermediate acting). These letters are important identifiers for insulin. Fixed-combination insulins are now available (Figure 20-2). These insulins have become popular for clients who must mix fast-acting and intermediate-acting insulins. The purpose of the fixed-combination insulins is to simulate the varying levels of insulin within the bodies of diabetic persons. The availability of the premixed combination insulins has also decreased the need for clients to mix insulins. Examples of fixed-combination insulins are Humulin 70/30, Novolin 70/30, Humulin 50/50, and Humalog Mix 75/25. Humulin 70/30 is used most often. The 50/50 insulin concentration means there is 50% NPH insulin and 50% regular insulin in each unit. Therefore if the order was 20 units of 50/50 insulin, the client would receive 10 units of NPH (50% or 0.5 × 20 units = 10 units) and 10 units of regular insulin (50% or 0.5 × 20 units = 10 units). It is important to note that Humalog Mix 75/25 contains 75% lispro protamine insulin and 25% lispro “rapid insulin.” Figure 20-2 shows labels of fixed-combination insulins. Insulin is available in 100 units per mL multidose vials and supplied in units that denote strength. The major route of administration for insulin is by subcutaneous injection; it is never administered intramuscularly. Regular insulin, aspart, and glulisine are approved insulins for intravenous administration. Dosage and frequency of insulin administration are highly individualized. It can also be administered with insulin pens that contain a cartridge filled with insulin or with a CSII pump (continuous subcutaneous [subcut] insulin infusion). The CSII pump is used to administer a programmed dose of a rapid-acting 100 units per mL–insulin at a set rate of units per hour. Figure 20-3 shows the various delivery systems used to administer insulin. 1. Lo-Dose syringe—It has a capacity of 50 units (0.5 mL). Each calibration on the syringe measures 1 unit. There is also a 30-unit (0.3 mL) syringe, which is used to accurately measure very small amounts of insulin. It is marked in units up to 30 units. Each calibration is 1 unit. 2. 1-mL (100-unit) capacity syringe—The 100-unit syringe comes with even and odd numbers on it. There are two types of 1-mL syringes in current use. a. The single-scale syringe is calibrated in 2-unit increments. Any dosage measured in an odd number of units is measured between the even calibrations. This would not be the desired syringe for clients with vision problems. b. The double-scale syringe has odd-numbered units on the left and even-numbered units on the right. To avoid confusion, the scale on the left should be used for odd numbers of units (e.g., 13 units) and the scale on the right, for even numbers of units (e.g., 26 units). When even numbers of units are measured, each calibration is then measured as 2 units. To review what the syringes look like, see Figure 20-4 for the four types of insulin syringes discussed.
Insulin
TYPES OF INSULIN
FIXED-COMBINATION INSULINS
INSULIN ADMINISTRATION
Measuring Insulin in a U-100 Syringe
Insulin



 Practice Problems
Practice Problems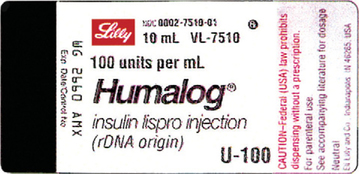

 Practice Problems
Practice Problems