Insulin Administration
Objectives
• Identify sites for insulin injections.
• Identify the different types of insulin labels.
• Compare the actions of fast-, intermediate, and long-acting insulins.
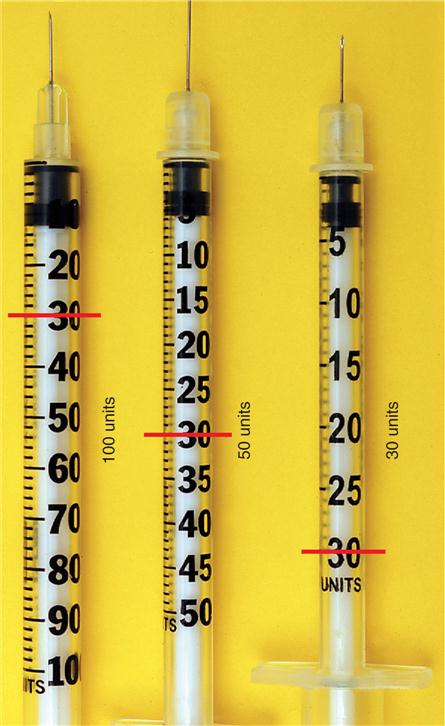
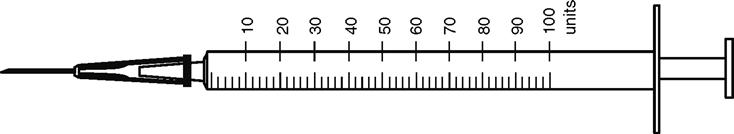
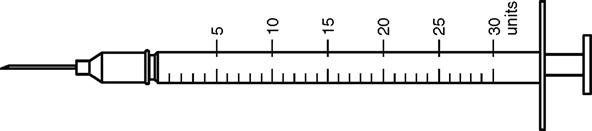
• Read calibrations on 30, 50, and 100-unit insulin syringes.
• Prepare single- and mixed-dose insulin injections.
• Calculate units of insulin based on CHO grams.
• Interpret the sliding scale using the BMBG method.
• Use electronic intravenous devices to administer insulin dosages.
• Calculate IV insulin for units/hr and mL/hr and duration.
Introduction
 According to the USP and the ISMP, insulin is the drug most commonly involved in errors. Insulin has been given as an overdose or confused with other unit measured medications such as heparin. The importance of measuring the correct amount of insulin is stressed. Different types of insulin syringes are shown for the practice of selecting the most appropriate syringe for the ordered dose. Mixing two types of insulin is shown in drawings. The bedside monitor blood glucose (BMBG) flow sheet shows how to use the sliding scale to chart hourly insulin needs. IV infusions are calculated for units per hour based on the BMBG level.
According to the USP and the ISMP, insulin is the drug most commonly involved in errors. Insulin has been given as an overdose or confused with other unit measured medications such as heparin. The importance of measuring the correct amount of insulin is stressed. Different types of insulin syringes are shown for the practice of selecting the most appropriate syringe for the ordered dose. Mixing two types of insulin is shown in drawings. The bedside monitor blood glucose (BMBG) flow sheet shows how to use the sliding scale to chart hourly insulin needs. IV infusions are calculated for units per hour based on the BMBG level.
Insulin
Insulin is an aqueous solution of the principal hormone of the pancreas. Insulin affects metabolism by allowing glucose to leave the blood and enter the body cells, preventing hyperglycemia.
Diabetes Mellitus
Diabetes mellitus is a deficiency of insulin and is classified according to cause. In type 1, which usually affects people before the age of 30, the pancreatic beta cells do not produce insulin. Insulin injections must be taken every day to control blood glucose levels.
The onset of type 2 diabetes usually occurs after 30 years of age; however, obesity has contributed to a rise in the diagnosis of type 2 diabetes in children and young adults. The pancreas produces some insulin but not enough to metabolize the glucose. In some cases, the insulin that is produced is not effective; this is known as insulin resistance. Of people with diabetes, 95% have type 2, and 40% of people with type 2 diabetes take insulin injections in conjunction with oral diabetes medications.
The most common complication of insulin therapy is hypoglycemia. This may be caused by injecting too much insulin (a risk in home care), by missing or delaying meals, or by being involved in more physical activity than usual. To treat hypoglycemia, a patient should always carry sugar in some form. The treatment of choice, if the patient can swallow, is glucose tablets (4 to 5 g carbohydrate [CHO] per tablet). Wait 15 minutes to retest the blood glucose. A glucose gel of 15 g is also available for the treatment of hypoglycemia. The glucose gel is to be used if the person cannot swallow but is still conscious. Put gel in the cheek along the gumline and rub vigorously. If the blood glucose level gets very low, unconsciousness may occur. At that point, the patient will need a glucagon injection. Emergency kits are available for home use (Figure 10-1). For patients weighing over 20 kg, use 1 mL. For patients weighing less than 20 kg, use 0.5 mg of glucagon.
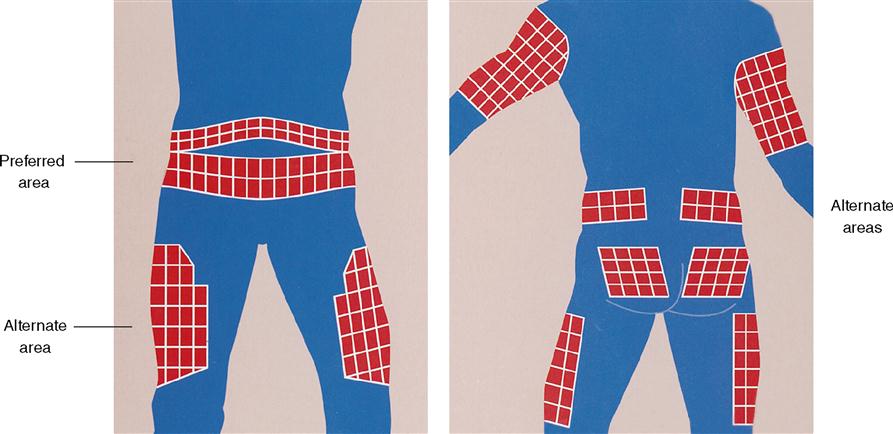
Injection Sites
The abdomen is the preferred site for insulin injections. When insulin injections are required on a daily basis, it is important to rotate within that site (Figure 10-2). The abdomen absorbs insulin more rapidly and is safer as an injection site than the upper arm, back, or thigh. If use of the abdomen is medically contraindicated, alternative sites may be used.
Types of Insulin
The source of insulin is either human or animal. This is known as the species of the insulin. Human insulin is manufactured to be the same as insulin produced by the body. Human insulin is made in one of two ways:
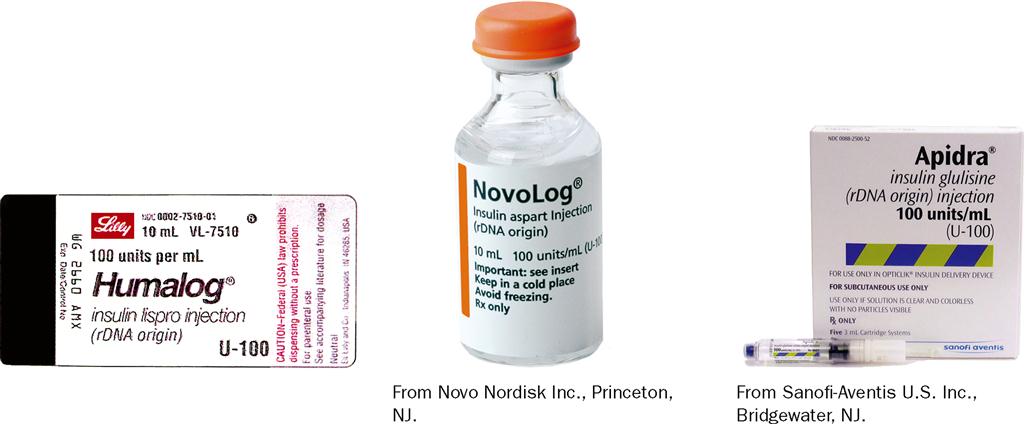
Humalog insulin (lispro) is recombinant DNA insulin with a rapid action of 5 to 15 minutes, allowing patients to dose and eat.
Recombinant DNA insulins cause fewer allergies than those from animal sources.
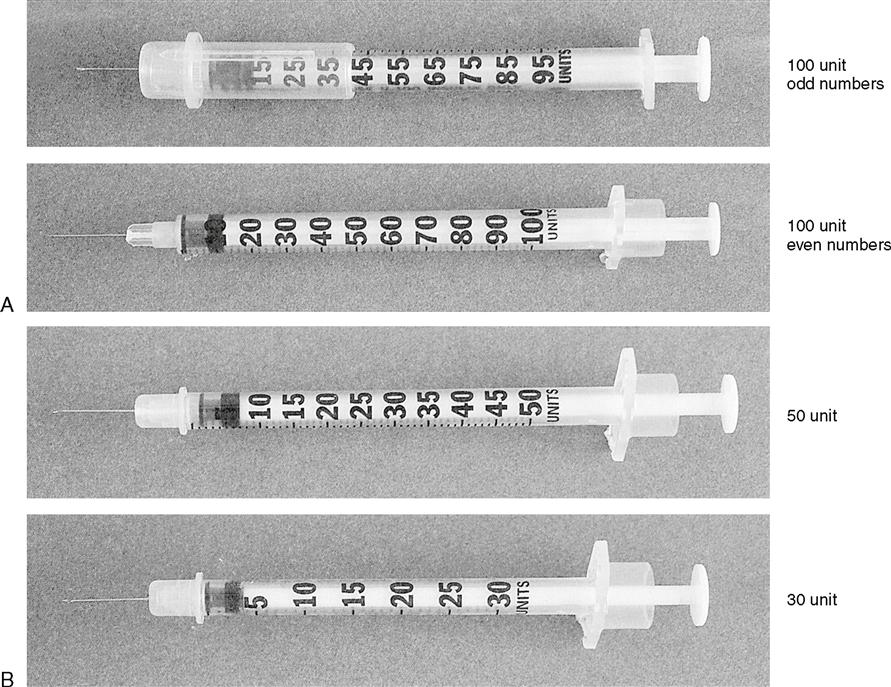
All insulin is supplied in units denoting strength. Insulin is given via special insulin syringes (Figure 10-3) and pens (Figure 10-4). Byetta stimulates glucose-dependent insulin from pancreatic beta cells (GLP-1 and GIP) and decreases glucagon production when glucose levels are elevated (Figure 10-5). Byetta is not insulin.
 CLINICAL ALERT
CLINICAL ALERT
It is essential that nurses know the signs and symptoms of hypoglycemia (too much insulin) and hyperglycemia (too little insulin) when caring for diabetic patients.
| Hypoglycemia Signs and Symptoms | Hyperglycemia Signs and Symptoms |
| rapid onset | several hour onset |
| cold clammy skin | warm skin |
| diaphoretic | flushed dry skin |
| nervous | lethargic |
| blood glucose below 70 mg/dL | blood glucose above 300 mg/dL |
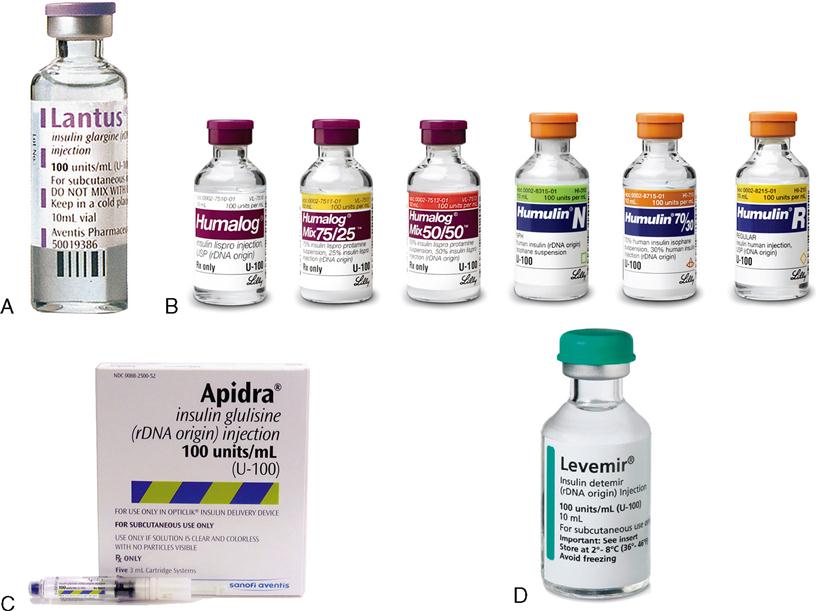
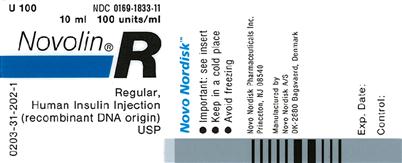
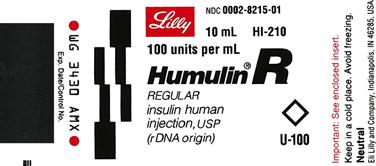
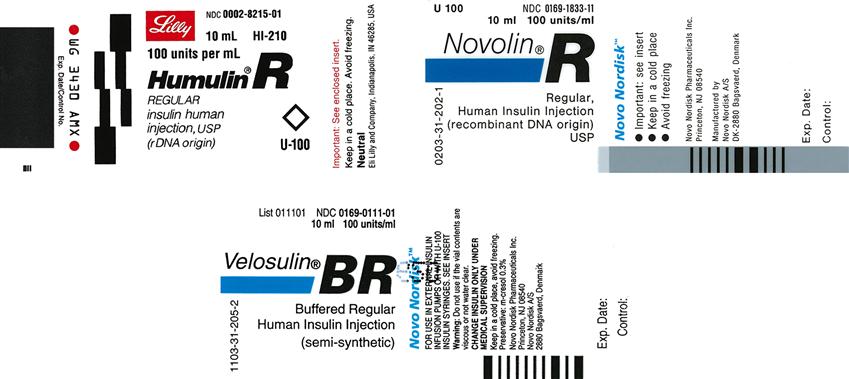
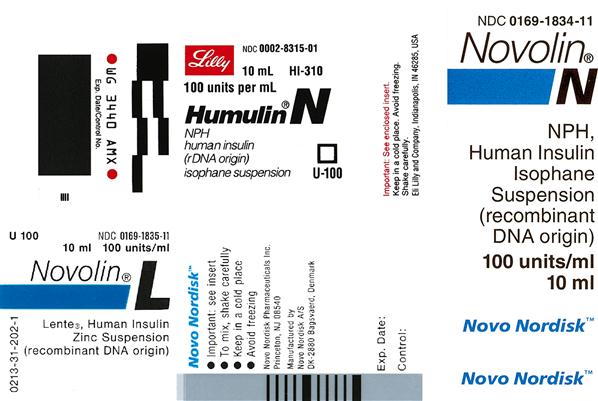
There are different types of cartridges used with insulin pens. Attached needles are usually 24- to 26-gauge with a  – or ½-inch needle. Insulin is supplied in 10 mL vials labeled U-100, which means there are 100 units/mL (Figure 10-6). Insulin is also supplied in 10 mL vials of U-500, which means there are 500 units/mL. This strength is used for those whose blood glucose levels fluctuate to very high levels. This type of insulin is rarely used and rarely kept on the nursing unit. Table 10-1 lists the duration of activity of various types of insulins and other injectables. See examples of various U-100 insulins on pages 229 and 230.
– or ½-inch needle. Insulin is supplied in 10 mL vials labeled U-100, which means there are 100 units/mL (Figure 10-6). Insulin is also supplied in 10 mL vials of U-500, which means there are 500 units/mL. This strength is used for those whose blood glucose levels fluctuate to very high levels. This type of insulin is rarely used and rarely kept on the nursing unit. Table 10-1 lists the duration of activity of various types of insulins and other injectables. See examples of various U-100 insulins on pages 229 and 230.
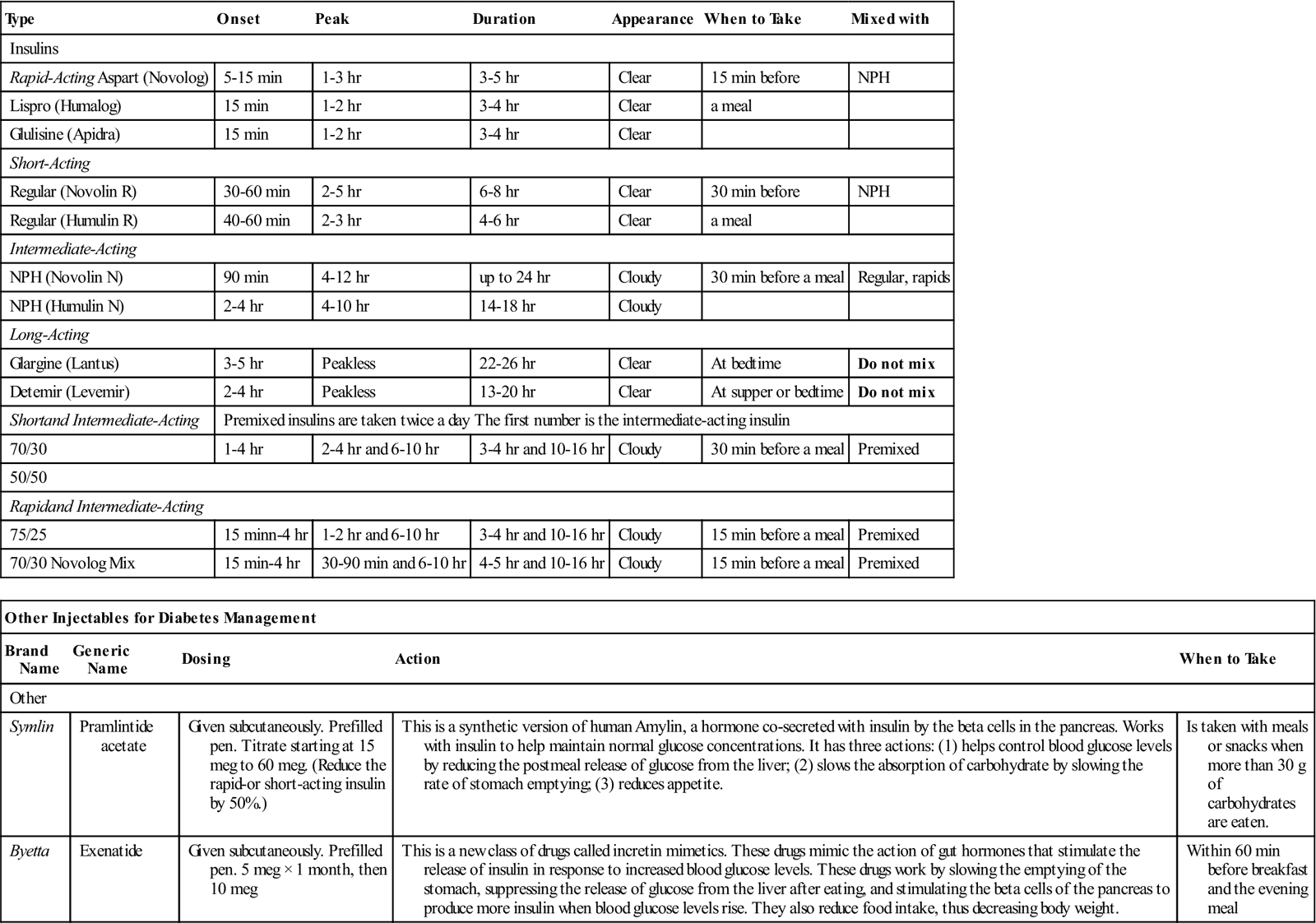
Table 10-1
Insulins and Other Injectables for Diabetes Management
| Type | Onset | Peak | Duration | Appearance | When to Take | Mixed with |
| Insulins | ||||||
| Rapid-Acting Aspart (Novolog) | 5-15 min | 1-3 hr | 3-5 hr | Clear | 15 min before | NPH |
| Lispro (Humalog) | 15 min | 1-2 hr | 3-4 hr | Clear | a meal | |
| Glulisine (Apidra) | 15 min | 1-2 hr | 3-4 hr | Clear | ||
| Short-Acting | ||||||
| Regular (Novolin R) | 30-60 min | 2-5 hr | 6-8 hr | Clear | 30 min before | NPH |
| Regular (Humulin R) | 40-60 min | 2-3 hr | 4-6 hr | Clear | a meal | |
| Intermediate-Acting | ||||||
| NPH (Novolin N) | 90 min | 4-12 hr | up to 24 hr | Cloudy | 30 min before a meal | Regular, rapids |
| NPH (Humulin N) | 2-4 hr | 4-10 hr | 14-18 hr | Cloudy | ||
| Long-Acting | ||||||
| Glargine (Lantus) | 3-5 hr | Peakless | 22-26 hr | Clear | At bedtime | Do not mix |
| Detemir (Levemir) | 2-4 hr | Peakless | 13-20 hr | Clear | At supper or bedtime | Do not mix |
| Shortand Intermediate-Acting | Premixed insulins are taken twice a day The first number is the intermediate-acting insulin | |||||
| 70/30 | 1-4 hr | 2-4 hr and 6-10 hr | 3-4 hr and 10-16 hr | Cloudy | 30 min before a meal | Premixed |
| 50/50 | ||||||
| Rapidand Intermediate-Acting | ||||||
| 75/25 | 15 minn-4 hr | 1-2 hr and 6-10 hr | 3-4 hr and 10-16 hr | Cloudy | 15 min before a meal | Premixed |
| 70/30 Novolog Mix | 15 min-4 hr | 30-90 min and 6-10 hr | 4-5 hr and 10-16 hr | Cloudy | 15 min before a meal | Premixed |
| Other Injectables for Diabetes Management | ||||
| Brand Name | Generic Name | Dosing | Action | When to Take |
| Other | ||||
| Symlin | Pramlintide acetate | Given subcutaneously. Prefilled pen. Titrate starting at 15 meg to 60 meg. (Reduce the rapid-or short-acting insulin by 50%.) | This is a synthetic version of human Amylin, a hormone co-secreted with insulin by the beta cells in the pancreas. Works with insulin to help maintain normal glucose concentrations. It has three actions: (1) helps control blood glucose levels by reducing the postmeal release of glucose from the liver; (2) slows the absorption of carbohydrate by slowing the rate of stomach emptying; (3) reduces appetite. | Is taken with meals or snacks when more than 30 g of carbohydrates are eaten. |
| Byetta | Exenatide | Given subcutaneously. Prefilled pen. 5 meg × 1 month, then 10 meg | This is a new class of drugs called incretin mimetics. These drugs mimic the action of gut hormones that stimulate the release of insulin in response to increased blood glucose levels. These drugs work by slowing the emptying of the stomach, suppressing the release of glucose from the liver after eating, and stimulating the beta cells of the pancreas to produce more insulin when blood glucose levels rise. They also reduce food intake, thus decreasing body weight. | Within 60 min before breakfast and the evening meal |
 CLINICAL ALERT
CLINICAL ALERT
Loss of vision is a complication of diabetes. U-30 and U-50 syringes have large numbers and are easier to read than the U-100 (1 mL) syringes. Tactile insulin measuring devices like the Jordan Medical Count-a-Dose enable nonvisual insulin measurement and mixing.
Types of U-100 Insulins
Short-Acting
Rapid-Acting
 CLINICAL ALERT
CLINICAL ALERT
Regular insulin should always be clear. Discard if unclear.
Mix insulins only with those of the same name because they may have differing amounts of preservatives. For example, Humulin R should be combined only with Humulin L or N. Humulin is a brand name.
Intermediate-Acting
Intermediate- and Rapid-Acting Mixtures
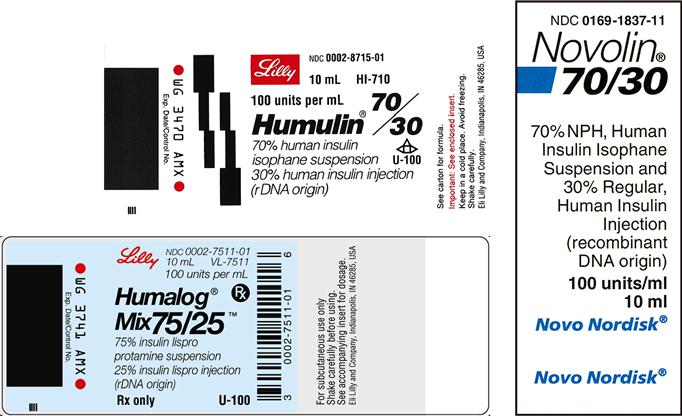
The insulin combination of NPH and Regular is used to give a 24-hour effect.
In 1 mL of Humulin 70/30, there are 70 units of intermediate-acting insulin and 30 units of rapid-acting insulin. In 1 mL of Humulin 50/50, there are 50 units of intermediate-acting insulin and 50 units of rapid-acting insulin.
Note: Mix before administration by rolling gently between the palms. Never shake because this creates bubbles.
 CLINICAL ALERT
CLINICAL ALERT
Insulin is available in various strengths: rapid acting, regular, intermediate-acting, long-acting, and combinations of rapid- and intermediate-acting. READ LABELS CAREFULLY TO AVOID GIVING THE WRONG STRENGTH.
Long-Acting

 CLINICAL ALERT
CLINICAL ALERT
Lantus must NOT be mixed in the same syringe with any other insulin or be diluted. It is NOT intended for IV administration. Caution: Lantus is clear like Regular Humalog. Lantus is given anytime for 24-hour coverage without a peak. Consistency in administration is necessary.
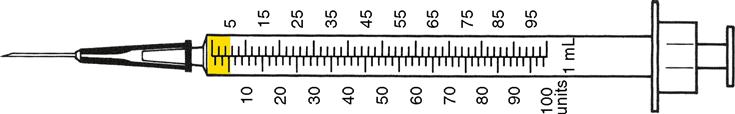
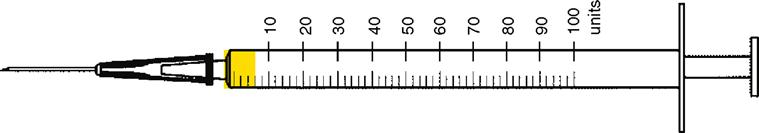
Insulin Syringes
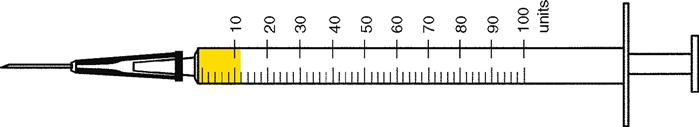
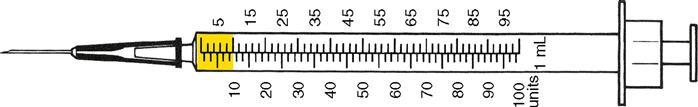
Insulin is usually given in a 1 mL or 0.5 mL insulin syringe calibrated to U-100 insulin. The 0.5 mL insulin syringe is used for smaller doses because the calibrations are larger and easier to read. The most commonly used insulin syringes are 50 and 100-unit syringes, as shown in Figure 10-3.
 CLINICAL ALERT
CLINICAL ALERT
Tuberculin syringes are calibrated in tenths and must never be substituted for insulin syringes, which are calibrated from 1 to 100 units.
Types of U-100 Insulin Syringes
Each calibration in the syringe shown in Figure 10-7 represents 1 unit. This syringe is used for small doses of 50 units or less and is used with U-100 insulin only. Needles are usually 24 to 26 gauge for subcutaneous injections. Clip-on magnifiers for syringes are available to enlarge the calibrations and numbers.
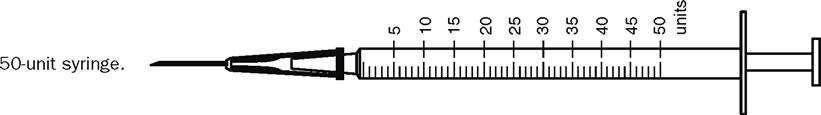
Each calibration in the syringe shown in Figure 10-8 equals 2 units. This syringe is for use with U-100 insulin only.
Each calibration in the syringe shown in Figure 10-9 represents 1 unit. This syringe is used for small doses of 30 units or less as a safety feature for people with diabetes who have vision problems (a Magni-Guide may also be useful for those people [Figure 10-10]) or for children who require small doses of insulin. This syringe is for use with U-100 insulin only.
Insulin Orders
A typical order for insulin must include the following:
A. The name of the insulin: Humulin, Novolin, Lantus.
B. The type of the insulin: regular, lispro, aspart, N, detemir, or glargine.
C. The number of units or amount the patient will receive: 10 units.
D. The time to be given: AM, ½ hr before a meal.
Example
Prepare 30 units of Humulin R insulin subcutaneously ½ hr before a meal. Using a 100 unit syringe, 50 unit syringe, or 30 unit syringe fill the syringe to the 30 units calibration (Figure 10-11). (All insulins come in U-100 so orders no longer specify U-100.)
 CLINICAL ALERT
CLINICAL ALERT
Units must be spelled out (not abbreviated by a U) because abbreviating can be a source of medication errors (e.g., mistaking the U for a zero). Insulin dosages require two licensed nurses to double check for accuracy.
Read the syringes and write your answers in the spaces provided.
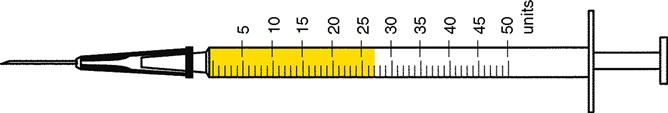
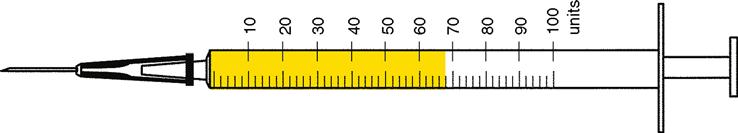
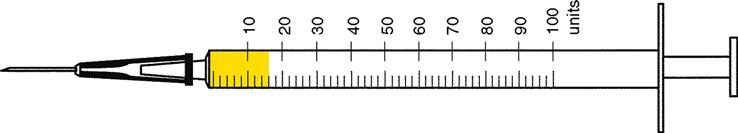
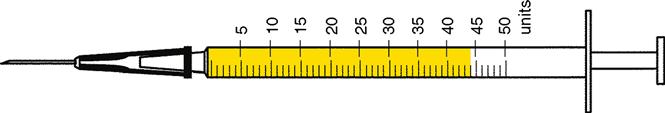
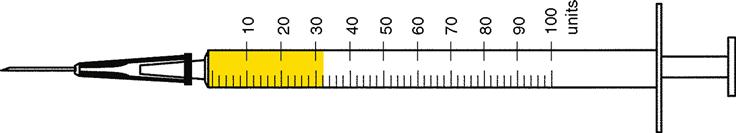
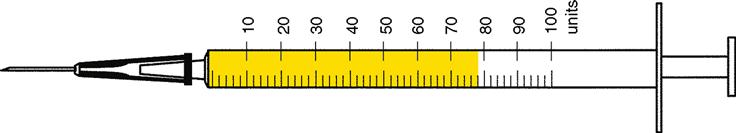
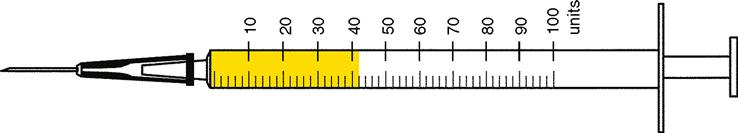
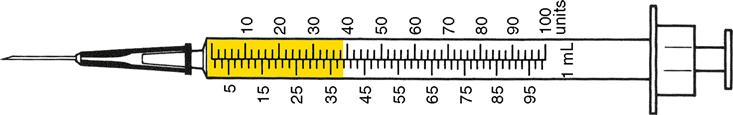
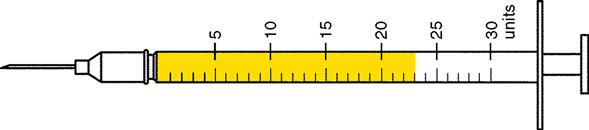
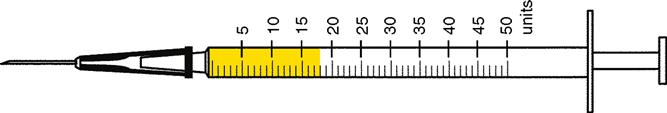
Circle the letter of the syringe with the correct ordered amount.