27 Insomnia
Definitions and epidemiology
Insomnia refers to difficulty in either falling asleep, remaining asleep or feeling refreshed from sleep. Complaints of poor sleep increase with increasing age and are twice as common in women as in men (Sateia and Nowell, 2004). Thus, by the age of 50, a quarter of the population are dissatisfied with their sleep, the proportion rising to 30–40% (two-thirds of them women) among individuals over 65 years.
Pathophysiology
Sleep systems
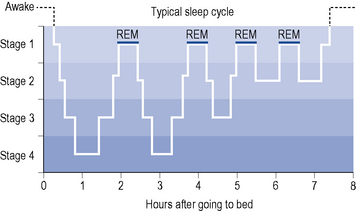
Orthodox sleep normally takes up about 75% of sleeping time. It is somewhat arbitrarily divided into four stages (1–4) which merge into each other, forming a continuum of decreasing cortical and behavioural arousal (see Fig. 27.1). Stages 3 and 4 represent the deepest phase of sleep and are also termed slow-wave sleep (SWS).
Aetiology and clinical manifestations
Insomnia may be caused by any factor which increases activity in arousal systems or decreases activity in sleep systems. Many causes act on both systems (Morin, 2003). Increased sensory stimulation activates arousal systems, resulting in difficulty in falling asleep. Common causes include chronic pain, gastric reflux, uncontrolled asthma and external stimuli such as noise, bright lights and extremes of temperature. Anxiety may also delay sleep onset as a result of increased emotional arousal.
Frequent arousals from sleep are associated with myoclonus, ‘restless legs syndrome’, muscle cramps, bruxism (tooth grinding), head banging and sleep apnoea syndromes. Reversal of the sleep pattern, with a tendency for poor nocturnal sleep but a need for daytime naps, is common in the elderly, in whom it may be associated with cerebrovascular disease or dementia. In general, decreased duration of sleep has been shown to increase the risk of obesity (Kripke et al., 2002) and hypertension (Gangwisch et al., 2006). Sleep disturbances in the elderly are also associated with increased falls, cognitive decline and a higher rate of mortality (Cochen et al., 2009). There is growing concern that daytime sleepiness resulting from insomnia increases the risk of industrial, traffic and other accidents.
Treatment
Non-drug therapies
Explanation of sleep requirements, attention to sleep hygiene (see Box 27.1), reduction in caffeine or alcohol intake and the use of analgesics where indicated may obviate the need for hypnotics (Anon, 2004). Medications that cause insomnia should also be avoided if possible. Psychological techniques such as relaxation therapy and cognitive behavioural therapy (CBT) are also helpful (Kierlin, 2008). However, studies comparing psychological approaches to hypnotics are scarce (Riemann and Perlis, 2009).
Hypnotic drugs
Benzodiazepines
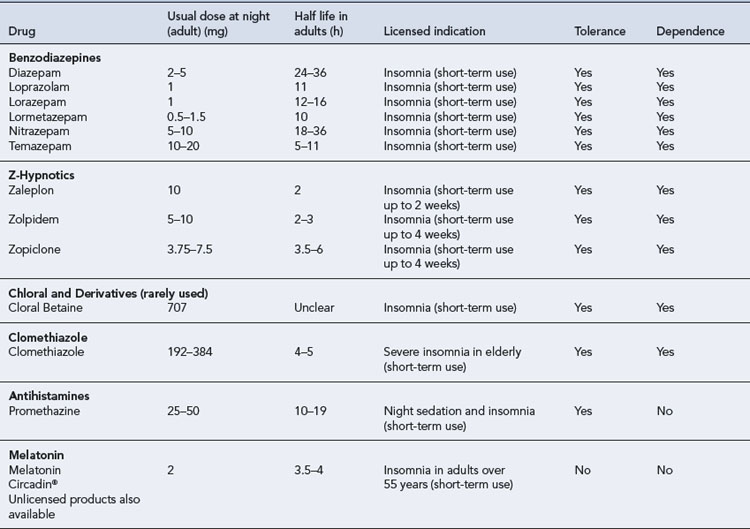
By far the most commonly prescribed hypnotics are the benzodiazepines. A number of different benzodiazepines are available (see Table 27.1). These drugs differ considerably in potency (equivalent dosage) and in rate of elimination but only slightly in clinical effects. All benzodiazepines have sedative/hypnotic, anxiolytic, amnesic, muscular relaxant and anticonvulsant actions with minor differences in the relative potency of these effects.
Pharmacokinetics
Most benzodiazepines marketed as hypnotics are well absorbed and rapidly penetrate the brain, producing hypnotic effects within half an hour after oral administration. Rates of elimination vary, however, with elimination half-lives from 6 to 100 h (see Table 27.1). These drugs undergo hepatic metabolism via oxidation or conjugation and some form pharmacologically active metabolites with even longer elimination half-lives. Oxidation of benzodiazepines is decreased in the elderly, in patients with hepatic impairment and in the presence of some drugs, including alcohol.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree