Injury to Abdomen
LTC Charles J. Fox
Abdominal vascular injuries present significant technical challenges and are among the most lethal injuries suffered by trauma patients. The need to achieve rapid proximal control of bleeding vessels located in the deep retroperitoneum without aggravating the injury is challenged by the presence of profound hemorrhagic shock or possibly cardiac arrest upon admission. Massive resuscitation requirements necessary to restore physiologic derangements like acidosis, coagulopathy, and hypothermia illustrate the technical dilemmas of having the necessary experience, precision, and surgical expedience to effectively deal with the morbidity and mortality associated with injuries to the abdomen.
The incidence of penetrating abdominal hemorrhage remains high in urban trauma centers where low-velocity handguns are prevalent and prehospital transport is rapid. Reports of military abdominal vascular injuries have been well documented in major conflicts of the 20th century, but have been infrequent and may be attributed to the wounding pattern and survivability on the battlefield. Common sites of bleeding are the viscera, mesentery, and blood vessels of the retroperitoneum and the focus of this chapter is to concentrate on the operative approach to abdominal vascular injury.
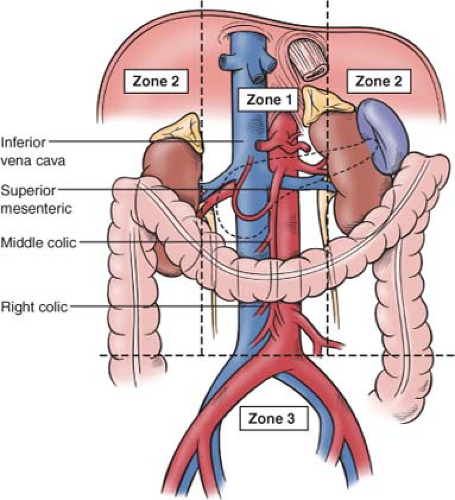
Abdominal vascular injury refers to the injury of major vessels located in the midline retroperitoneum (zone 1), upper lateral retroperitoneum (zone 2), pelvic retroperitoneum (zone 3), or the porto-retrohepatic area of the right upper quadrant. Zone 1 begins at the aortic hiatus and ends at the sacral promontory; it is located in the midline and courses on the top of the spinal column. This zone is further subdivided into the supramesocolic and inframesocolic zones. There are two zones 2 (right and left) and both are located within the pericolic gutters. Zone 3 begins at the sacral promontory and encompasses the pelvis (Fig. 1).
Injuries to the abdominal aorta and inferior vena cava injuries are defined in relation to the renal vessels and the liver, respectively. The renal and superior mesenteric arteries may be injured in any of the classic anatomic zones. Larger veins are usually injured at the confluence of smaller tributaries. For example, the portal vein can be injured within the portal triad or at the confluence of the superior mesenteric and splenic veins. Renal veins may be injured, either at their confluence with the inferior vena cava or at the renal hilum. An injury to the superior mesenteric vein is defined in terms of the relationship to the pancreas categorized by the infrapancreatic or retropancreatic location.
Penetrating injuries commonly result in lateral wall defects with diffuse intraperitoneal bleeding or expanding hematomas of the mesentery or retroperitoneum. Thrombosis and complete transections of major abdominal vessels are much less common. Intimal injury can also be observed secondary to blast effects and is especially common with military munitions. Arteriovenous fistulae of the hepatocaval, mesenteric or renal vessels are very rare findings. Blunt injuries of the abdomen are the result of deceleration forces and may produce thrombosis, intimal injury, or lateral wall defects of the mesenteric vessels. Avulsions of small branches of major vessels such as intestinal branches at mesenteric fixation sites may result in thrombosis or pseudoaneurysm.
The clinical presentation is dependent upon the nature of the vascular injury. Complete transections and lateral wall defects from penetrating injury can produce hemorrhage and hypotension that may respond to resuscitative fluids secondary to tamponade. In cases of persistent intraperitoneal bleeding, progressive hypotension, peritonitis, and abdominal distention is usually observed. The specific physical examination findings will depend upon the degree of free intraperitoneal bleeding and may also be associated with flank pain or lower extremity pulselessness.
Acute traumatic thrombosis may lead to abdominal pain (superior mesenteric artery), hematuria (renal artery), or lower extremity ischemic changes with abnormal ankle–brachial indices (abdominal aorta). This may be particularly evident for transpelvic trajectories that may result in injury to the iliac vessels and can be associated with the loss of a femoral pulse. A focused assessment for the sonographic evaluation of the trauma patient (FAST) is a practical way of making the diagnosis of an associated cardiothoracic injury in patients with both stable and unstable abdominal vascular injury.
Acute traumatic thrombosis may lead to abdominal pain (superior mesenteric artery), hematuria (renal artery), or lower extremity ischemic changes with abnormal ankle–brachial indices (abdominal aorta). This may be particularly evident for transpelvic trajectories that may result in injury to the iliac vessels and can be associated with the loss of a femoral pulse. A focused assessment for the sonographic evaluation of the trauma patient (FAST) is a practical way of making the diagnosis of an associated cardiothoracic injury in patients with both stable and unstable abdominal vascular injury.
Laboratory tests are of minimal value in the early diagnosis of abdominal vascular injuries. An initial complete blood count (CBC) should be obtained to monitor the status of the hemoglobin and hematocrit. An arterial blood gas (ABG) is useful to establish the presence of an acidosis and to determine the effectiveness of oxygenation and ventilation. These studies are frequently repeated to assess the effectiveness of resuscitative efforts and to monitor the correction of acidosis, abnormal base deficits, and traumatic coagulopathy that are often evident upon admission. Massive transfusions should be anticipated for those unstable patients who present with a low systolic blood pressure (<100 mm Hg).
Plain radiographs can be a useful diagnostic adjunct in determining the missile track to predict the site of an abdominal vascular injury. When immediate laparotomy is not indicated, stable patients with blunt abdominal injury should have an abdominal computed tomography (CT) scan. Multidetector row CT angiography can now detail a vascular injury with the accuracy and resolution that may eventually surpass that achieved by conventional preoperative aortography. When catheter-based interventions such as coil or gel-foam embolization are planned to control pelvic hemorrhage, transfemoral arteriography is useful in making the diagnosis of intimal injury, thrombosis, or in locating the site of hemorrhage.
The degree of initial resuscitation will depend on the presenting condition and location of the patient. A decision regarding the need for thoracotomy with thoracic aortic cross clamping should be made for the “in extremis” patient with a penetrating abdominal injury, immediately upon admission to the emergency department. Those with penetrating injuries are taken quickly to the operating room once the patient is identified, the airway is controlled, and thoracostomy tubes are inserted. Laboratory studies should be obtained in the admitting area while achieving intravenous access. It is not advisable to place intravenous lines into the femoral veins as iliac venous or inferior vena caval injuries may be actively hemorrhaging. Large intravenous catheters should be inserted in the upper extremities or in the subclavian or jugular veins. Similar to penetrating injury, the patient with hypotension and blunt abdominal vascular injury should also have an immediate celiotomy once the diagnosis of hemorrhage is established by the surgeon. Additional lines and other maneuvers should not delay the transport of the patient. The anesthesia team can often optimize intravenous access and hemodynamic monitoring during the final positioning, draping, and preparation of the patient for surgery.
Damage control resuscitation is crucial for success and emphasizes immediate blood bank notification, activation of massive transfusion protocols, and early transfusion of blood products in the admitting area. Prewarmed crystalloid fluids, transfusion of blood through high-flow warming devices, and replacement of prewarmed blankets with a heating unit are important maneuvers to prevent or decrease hypothermia. The entire chest, abdomen, and upper thighs are prepped in anticipation of extending an incision across body cavities or harvesting the saphenous vein for an autologous vascular reconstruction. Before a midline abdominal incision is made, the surgeon should ensure that all vascular instruments, sponge sticks, and suture materials are available, and that the anesthesia team is prepared for dramatic hemodynamic changes.
A midline incision is made and all clots and pooled blood are evacuated from the abdominal cavity to rapidly inspect areas of hemorrhage. Active hemorrhage is controlled by packing solid organs and by standard vascular techniques with emphasis on digital compression, and adequate dissection before clamping proximal and distal to bleeding vessels. Sponge sticks and kitners are very useful for controlling hemorrhage from perforations of the iliac or renal veins and the inferior vena cava.
For a retroperitoneal hematoma or hemorrhage associated with an injury to the midline retroperitoneum and base of the mesentery, the operation is approached differently depending on the likelihood of an injury to the suprarenal paravisceral abdominal aorta (supramesocolic), or to the infrarenal abdominal aorta, left renal vein, or inferior vena cava (inframesocolic). In general, all midline hematomas in the zone 1 region regardless of mechanism (blunt or penetrating) are opened. Hematomas in zones 2 and 3 (upper lateral or pelvic retroperitoneum) are all opened in penetrating wounds but in blunt abdominal injury are only opened when hematomas are ruptured, rapidly expanding, or pulsatile.
A left-sided medial mobilization is the preferred operative approach for injury to the suprarenal abdominal aorta. This includes division of the lateral retroperitoneal attachments beginning along the avascular line of Toldt, and progressive reflection of the left colon, kidney, spleen, tail of the pancreas, and fundus of the stomach to the midline (Fig. 2). This allows complete visualization of the entire aorta from the diaphragm to the bifurcation of the iliac vessels (Fig. 3). Care must be taken to ensure that the spleen is not injured. Time-consuming dissection of the celiac plexus can be spared by transecting the left crus of the aortic hiatus of the diaphragm to expose the distal thoracic aorta to rapidly apply a supraceliac aortic clamp.
Active hemorrhage may require hasty manual anterior compression for temporary proximal control superior to the wound. Although manual compression may initially limit the ability to repair the vascular injury, additional exposure is achieved by dividing the lesser omentum, retracting the stomach and esophagus to the left, and manually separating the crura muscle fibers from the supraceliac aorta to obtain proximal control of the injury. Small tears are repaired using a long 3-0 or 4-0 polypropylene suture. Patch aortoplasty using Dacron or polytetrafluoroethylene (ePTFE) is used for larger perforations to avoid an iatrogenic stenosis. An end-to-end anastomosis is used for short segmental defects when a tensionless repair is possible. When a prosthetic conduit is necessary, a 14-mm Dacron or ePTFE graft (slight undersizing encouraged) is sufficient in the nondiseased adult aorta. If concomitant bowel injury exists, then the enteric contents are first controlled with clamps, followed by aortic repair, closure of the retroperitoneum, copious irrigation,
and subsequent reconstruction of the gastrointestinal tract.
and subsequent reconstruction of the gastrointestinal tract.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree