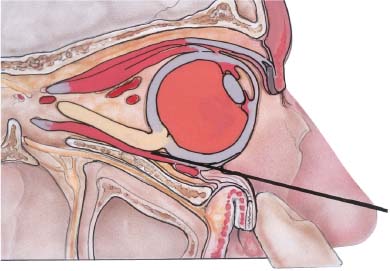
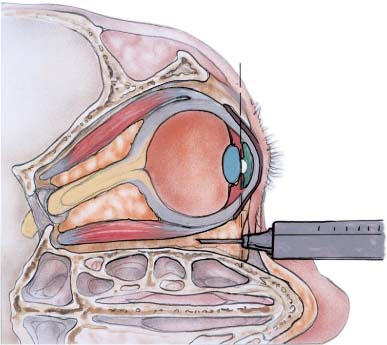
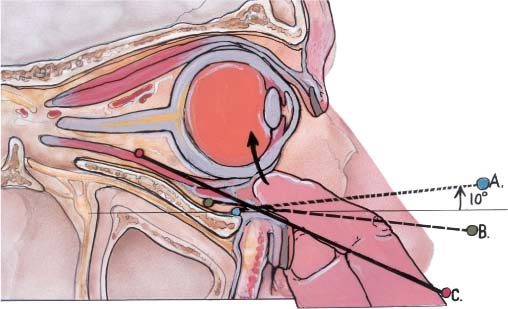
Chapter 1 Complications of regional anesthesia for ophthalmic surgery have become increasingly rare. This decreasing frequency can be attributed to awareness of anatomy and consequently better strategy for administering anesthetics, development of a safe and effective array of anesthetic substances, and the use of appropriate monitoring in the perioperative period. Nonetheless, while many anesthetic complications may be relatively innocuous, some may be sight- or even life-threatening. As such, the administration of anesthesia should be done with proper training and experience and with care and respectful attention to detail. In fact local anesthesia is the greatest single hazard in cataract surgery,1–4 accounting for adverse effects in 3.5% of patients (orbital adverse effects: 2.6%; systemic: 0.9%) according to a study by the Royal College of Ophthalmologists. The average cataract surgeon in the United States has a 3% chance each year of being sued over cataract surgery,5 and the majority of such cases relate to anesthetic complications such as globe perforations, inadvertent intraocular injections, and retinal detachment and intraocular hemorrhage associated with these misadventures.6 The purpose of anesthesia is to convert an otherwise painful, anxiety-producing, and unpleasant experience into a tolerable, comfortable, even pleasant and restful experience. In choosing an anesthetic technique, the least invasive, safest method, should always be employed. The extent, duration, and complexity of the surgery should therefore be evaluated in choosing the route, duration, and depth of anesthesia employed. Exposure to anesthesia in excess of that which is necessary adds unnecessary risk to the procedure, and no tangible benefit to patient or surgical team. Regional anesthesia is usually preferable to general anesthesia, producing safer, equally effective, and cost-efficient results. However, just as it is inappropriate for a surgeon to use the same technique for every surgical intervention, it is equally wrong to use the same anesthetic for each case. While surgeons may subscribe to a particular philosophy of anesthesia for routine cases, it is important to assess each patient’s needs and act appropriately for exceptional cases. Injectible techniques are anesthetic methods that involve the use of a sharp needle and an injectate; they include peribulbar as well as retrobulbar techniques, unless otherwise specified. The procedures collectively are referred to as “regional orbital anesthetic block.”7 It has been suggested that peribulbar block (also referred to as “periconal block”), involving injection outside of the muscle cone, entails less risk of complication than retrobulbar technique. However true this may be, complications have been observed with both techniques.8 Good planning is always part of the strategy to limit risk in anesthetic administration. If patients have preexisting systemic medical conditions, then some authors have felt that history, physical examination, and laboratory testing should be performed.9 There is a great deal of regional and international variation in these requirements and no good standards have yet been established. A prospective multicenter clinical trial is evaluating this issue in 20,000 patients in the United States and Canada. The Study of Medical Testing for Cataract Surgery Randomized randomizes patients into either a no-routine-screening group or a routine-screening group; the latter group receives an electrocardiogram (EKG), electrolytes/glucose, and a complete blood count (CBC). Demographic, clinical, and perioperative and medical event data is being collected through 7 days post-surgery to determine whether such testing results in differences in complications and outcomes between the two groups. A recent study by Rosenfeld et al,10 however, showed that the need for anesthesia intervention during cataract surgery was not correlated with the presence of heart disease, evidenced by an abnormal preoperative EKG, or with the presence of diabetes. EKGs and blood sugar are almost always performed during a preoperative evaluation. However, a history of systemic hypertension, pulmonary disease, renal disease, or cancer was associated with a statistically significant increase in incidence of intervention, suggesting that at least a review of the patient’s medical conditions is prudent in the immediate preoperative assessment. Some investigators have shown that anesthetists did not make use of reported results of preoperative test and examinations, and that perioperative management was not influenced because of these investigations.11 Data from the National Survey of Local Anaesthesia for Ocular Surgery in 1997 reveals further that in patients who did not have any preoperative tests, there was a very low rate of serious adverse events that would have been influenced by such tests.12 Because cataract surgery is commonly performed on geriatric patients, a high incidence of systemic conditions such as diabetes, hypertension, coronary artery disease, obesity, chronic obstructive pulmonary disease, and arthritis may coexist and pose special challenges to the surgical and anesthesia teams. To limit the risks these conditions may generate, every effort should be made to ensure that the patient is optimally prepared for surgery. Nonetheless, cataract surgery can, in most instances, take place even in patients with these conditions. During the immediate preoperative consultation, the patient should be asked to provide a list of current medications. In this way potential drug interactions can be anticipated, and it can be confirmed that the patient has appropriately taken the medications. It is helpful to schedule diabetic patients during the early morning, so that their oral hypoglycemics or insulin dosage can be taken immediately after the surgery. This minimally disrupts their usual routine. Alternatively, they can be scheduled during the early afternoon so that they take their insulin and breakfast earlier in the day with sufficient time to fast prior to surgery. In general it is advisable to continue patients on systemic anticoagulants during routine cataract surgery, particularly in cases of small-incision phacoemulsification. Discontinuation of anticoagulant therapy may bear a greater risk than that of significant intraoperative ocular bleeding, even with retrobulbar injection.13 In these cases, however, it is of particular importance to use small needles and correct anatomic placement, and to avoid excessive manipulation while administering the injectible block. There are no studies to date, however, that have categorized the risk of cessation of anticoagulation as opposed to its continuance for many medical indications. It is recognized that stopping these medications has different implications for risk, depending on the underlying medical condition (e.g., atrial fibrillation vs. stroke vs. heart valve replacement). For example, a patient with mechanical heart valve replacement is at substantially higher risk for embolism or stroke than one with atrial fibrillation as the underlying reason for treatment. These factors should be weighed carefully, in consultation with the patient’s internist, to determine the systemic and ocular risks in each case. In the United States, both CRNAs (certified registered nurse anesthetists) and physician (MD or OD) anesthesiologists have been trained to administer anesthetics, monitor and treat a patient’s systemic condition, and provide suitable sedation. Although there are regional variations in the usage of anesthesia services both through the United States and internationally,14 the role of this vital team member cannot be overlooked. In an era where cost containment has reached a high degree of awareness, it is important to evaluate the necessity of each aspect of the care we provide. Rosenfeld et al10 showed that during cataract surgery, major anesthesia intervention (i.e., more than just verbal reassurance, hand holding, or physical restraint) was required in 28.6% of all patients. While intervention was required more often in patients with certain underlying diseases, almost a third of patients without predisposing factors required intervention of some type. This suggests that with current methods it is impossible to predict preoperatively which patients will require intervention, thereby suggesting further that, to avoid perioperative complications, anesthesia monitoring is essential in all patients undergoing cataract surgery. Considerable debate has persisted regarding the usefulness of intravenous (IV) sedation for cataract surgery, particularly with the use of topical anesthetic agents and minimally invasive surgical technique. Although the specifics of this debate are outside the realm of this discussion, it is important to understand what constitutes appropriate use of this mode of treatment. The anesthesiologist must possess appropriate personality traits and communication skills to enable them to gain patient trust and confidence.15 Additionally, the practitioner should educate the patient about the forthcoming experience. This helps to reduce the patient’s anxiety and decrease perioperative complications.16 Perioperative monitoring should consist, at a minimum, of EKG, pulse oximetry, and periodic blood pressure measurement.17,18 The latter should be kept to a minimum during critical surgical periods so as not to increase patient discomfort, anxiety, or movement during surgery. The goal of IV sedation is to alleviate anxiety, while allowing the patient to remain stationary, calm, comfortable, and cooperative. In regard to the absolute amount of anesthetic agent given and the level of consciousness attained, elderly patients generally require less pharmacologic limitation of anxiety during surgery than do younger patients. It is essential to produce anxiolysis without obtundation. The latter may result in a patient who is periodically and unpredictably combative,19–22 and may cause further depression of preexisting cardiac and respiratory instabilities.23–27 In an effort to prevent this situation, excessive IV sedation should never be used to compensate for an incomplete regional anesthetic block. Rather, the incomplete regional block should be managed by supplementation of the local anesthesia. To do otherwise will subject the patient to an unpleasant, stressful, and potentially dangerous experience.15 Systemic toxicity of anesthetic agents is usually associated with (1) inadvertent ectopic injection of an agent, (2) overdose of a particular agent, (3) allergic reactions, or (4) vasovagal responses. Ectopic injection may be propagated by the intravascular route or through inadvertent direct central nervous system injection through the subdural route via penetration of the optic nerve sheath. These will each be discussed in their respective sections. However, as a general measure, limitation of these problems can be accomplished by (1) gentle preinjection aspiration to ensure an extravascular location of the needle, and (2) slow and patient injection of anesthetics15 (no more than 2 cc/min) while monitoring the patient for any signs of systemic toxicity. Finally, the use of hyaluronidase may be associated with allergic or frankly anaphylactic reactions.28 Therefore, this proteolytic drug should be avoided in atopic individuals. A study by Prosser et al29 suggests that hyaluronidase may not be necessary, at least in peribulbar blocks. In preparation for the administration of the injection, the surgeon must have an awareness of the axial length of the surgical eye. A preexamination of the orbit/globe relationship should be done, and proper instruction to the patient should be given so as to avoid unnecessary movement. A history of prior difficulties with regional block in the companion eye should also be investigated and etiologic factors delineated before proceeding with the second eye. Techniques that may reduce the likelihood of perforation have been described by numerous authors. Current practice consists of a sharp needle technique with insertion either at or slightly below the lateral canthus, or, alternatively, at the medial canthus. The needle is placed preferably though the conjunctiva rather than through the lid. The eye should be held open, remain in primary gaze, and be observed throughout the needle insertion and anesthetic injection. The eye should not move during this maneuver, as this may indicate that the sclera has been engaged. The classic concept of looking “up and in,” as popularized by Atkinson, should be absolutely avoided because it brings the optic nerve closer to the inferotemporal quadrant and places it on stretch, making it more susceptible to injury (Fig. 1–1). There is still debate about the ideal needle for this task. Some authors, such as Waller et al, recommend using a dull needle, stating that a theoretically greater force would be required to penetrate the sclera. This argument, however, fails when one considers that any needle sharp enough to penetrate the skin will probably encounter little difficulty in penetrating the sclera. Further, because eyes at high risk for perforation often have scleral ectasia, there would be sufficient thinning to allow even a dull needle to penetrate. I prefer a straight, sharp, 27-gauge, short (no longer than 31 mm) bevel needle inserted as described above, with the bevel toward the globe, thus reducing the risk of damage to critical structures. FIGURE 1–1 Optic nerve damage. When eye is positioned “up and in,” as has been the classic teaching, the nerve is placed on stretch and positioned more inferiorly and temporally. This increases the risk of nerve damage during injection. A medial orbital injection is also occasionally utilized. In this technique the needle is placed at the caruncle and injection is administered with the needle positioned with the bevel facing away from the globe so as to accommodate the sharply medioposterior sloping of the medial orbital wall (Fig. 1–2). FIGURE 1–2 Medial block. A 27-gauge, 20- to 25-mm sharp needle is placed at the caruncle with the bevel pointed away from the globe. When the needle hub reaches the plane of the iris, the anesthetic is injected near the medial orbital wall. In retrobulbar anesthesia, the needle is inserted inferiorally, one-third the way from the lateral canthus. It is then advanced along the orbital floor. Immediately on perforating the skin or conjunctivae, the globe is actually pushed superiorally with digital pressure. Once the needle is well past the equator, it is slightly withdrawn and redirected superiorally at an approximately 15-degree angle. The needle can be felt to “pop” through the muscle cone, and the anesthetic volume is delivered with a slow and steady injection, with attention to any unusual resistance (Fig. 1–3). With peribulbar anesthesia the needle is inserted similarly, but never redirected into the muscle cone. Instead, the anesthetic is delivered near the orbital rim. Generally it is necessary to wait a longer period of time after a peribulbar block for adequate anesthetic effect. Peribulbar injection is particularly useful superotemporally to provide sensory and motor anesthesia to the superior orbit and lid (Fig. 1–4). The administration of regional orbital anesthetic block is a technique requiring specific training and experience. In some institutions the block is given by the least experienced surgeon or by anesthesia personnel who often have inadequate experience or training. This practice is to be discouraged. A detailed study of the orbit, its nerves, vasculature, and soft tissue septa should be undertaken prior to undertaking injectible anesthesia. Regional orbital anesthesia requires an anatomic appreciation in three dimensions. To ensure success, hands-on, one-to-one training is required. Globe penetration is the most common of the serious complications of injectible anesthesia and has been documented by numerous authors.30–33 Globe perforation and inadvertent intraocular injections also rank as two of the most common causes of litigation after cataract surgery.6 Ocular penetration refers to the entry of a needle into the globe after which the needle is withdrawn. Ocular perforation suggests that the needle entered the eye and then exited through another part of the globe prior to having been withdrawn. Because the clinical pictures are similar, the terms are used interchangeably in this discussion. The actual incidence of ocular penetration is difficult to determine. This is due to a tremendous diversity of reports that have appeared in the literature. Reported incidences range from as few as one penetration in 16,224 consecutive cases,34,35 to as many as 1 in 100 cases. Teichmann and Uthoff36 reported an incidence of 0 in 21,000 using their technique. If the incidences reported in several available references are averaged, the occurrence rate is approximately 0.01%. FIGURE 1–3 Inferotemporal block. The eye is held in primary gaze. The eye is digitally elevated and the injection is performed through the conjunctivae. (A) The needle passes posteriorally at a 10 to 15-degree elevation from the coronal plane until the equator is reached. (B) The needle is then advanced slowly, dropping the hub as it passes over the orbital floor. (C) The needle hub, now behind the equator, is depressed and the tip is advanced through the muscle cone.
INJECTIBLE OPHTHALMIC
ANESTHESIA
GENERAL CONSIDERATIONS
DEFINITION OF INJECTIBLE BLOCK
PREOPERATIVE ASSESSMENT
CONSIDERATIONS REGARDING ANTICOAGULATION
THE ROLE OF THE ANESTHESIA CAREGIVER
SEDATION AND MONITORING
COMPLICATIONS OF PHARMACOLOGIC AGENTS
TECHNIQUE OF RETRO/PERIBULBAR INJECTION
PENETRATION AND PERFORATION OF THE GLOBE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree