Chapter 2 Inflammation
Inflammation
Inflammation is the dynamic process by which living tissues react to injury. They concern vascular and connective tissues particularly.
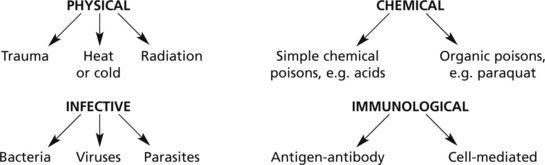
Various agents may kill or damage cells:
… and any other circumstance leading to tissue damage, e.g. vascular or hormonal disturbance.
Acute Inflammation
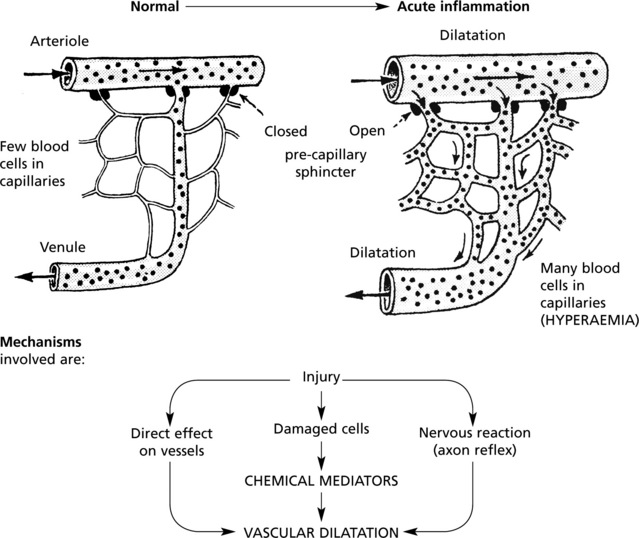
Hyperaemia
The hyperaemia in inflammation is associated with the well known microvascular changes which occur in Lewis’ triple response – a FLUSH, a FLARE and a WEAL. It occurs when a blunt instrument is drawn firmly across the skin and illustrates the vascular changes occurring in acute inflammation.
The stroke is marked momentarily by a white line due to vasoconstriction.
The flush, a dull red line, immediately follows and is due to capillary dilatation.
The flare, a bright red irregular surrounding zone, is due to arteriolar dilatation.
hyperaemia explains the classical signs of redness and heat.
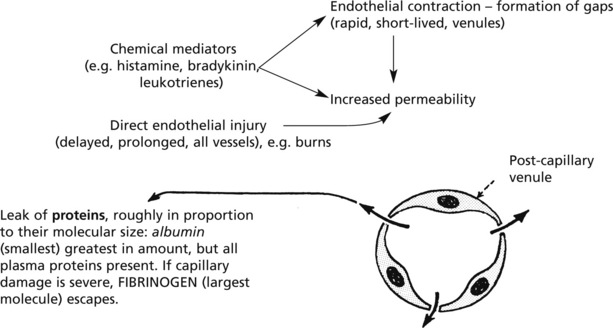
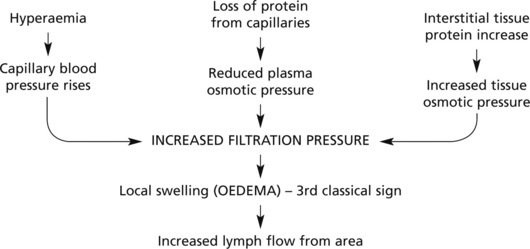
Exudation
Exudation is the increased passage of protein-rich fluid through the vessel wall into the interstitial tissue. It explains the weal in Lewis’ triple response.
| Advantageous results | Contents of fluid |
|---|---|
| Fluid increase | (a) Globulins → protective antibodies |
| ↓ | (b) Fibrin deposition → Helps to limit spread of bacteria |
| Dilution of toxins | (c) Various factors promoting subsequent healing |
Emigration of Leucocytes
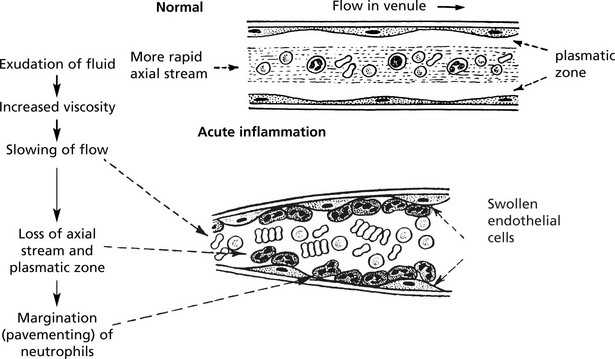
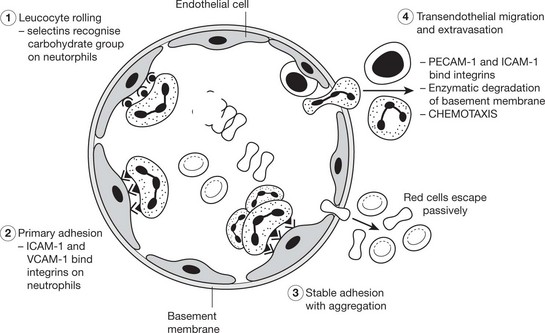
Neutrophils and mononuclears pass between the endothelial cell junctions by amoeboid movement through the venule wall into the tissue spaces. In this process both neutrophils and endothelial cells are activated and both express cell adhesion molecules, initially
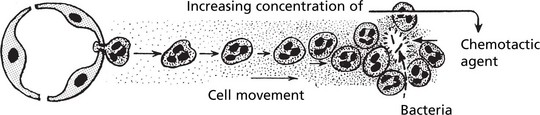
Chemotaxis
The initial margination of neutrophils and mononuclears is potentiated by slowing of blood flow and by increased ‘stickiness’ of the endothelial surface.
Important examples of chemotactic agents are:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree