2South West Health Protection Agency
- key concepts and terminology in infectious disease epidemiology;
- principles of and methods for infectious disease surveillance and outbreak management.
Introduction
An infectious disease is an illness resulting from the transmission of a pathogenic biological agent – including some viruses, bacteria, fungi, protozoa, parasites and prions – to a susceptible host. A communicable disease is an infectious disease that can be transmitted directly or indirectly from person to person. The ‘germ theory’ of disease, attributing the presence of disease to specific micro-organisms, was firmly established in the late 19th century by the work of Louis Pasteur and Robert Koch. Earlier studies by John Snow and William Budd, who are often considered among the forefathers of modern epidemiology, had demonstrated the contagiousness of cholera and typhoid through contaminated water, although not the specific agents responsible. This knowledge provided the scientific basis for infectious disease control, which is among the key public health successes of the twentieth century: including, as highlighted in Chapter 15, improvements in hygiene, the advent of effective antibiotic therapy and successful vaccination programmes.
Despite these advances, the burden of infectious disease remains high, particularly in low-income countries and we face new challenges from emerging infections and organisms resistant to antimicrobials. Globally, an estimated 68% of the 8.8 million deaths in children under 5 years are due to infectious diseases, with the most common causes being pneumonia (18%), diarrhoea (15%) and malaria (8%) (Black, 2010). In England, the mortality associated with infectious disease is much lower (although, still an estimated 10% of deaths overall have an underlying infectious cause) but the financial burden remains high at around £6 billion per annum, with respiratory infections, infectious intestinal disease, health-care acquired infections and HIV/AIDS contributing the greatest cost.
There are many reasons why infections continue to take their toll. In the poorest countries inadequate health care and sanitation play a large role, and effective interventions may not be available, deliverable or affordable for those most in need. Globally, new infectious agents continue to emerge; three examples among a long list in recent decades include the recognition of HIV/AIDS in the 1980s, the emergence of variant CJD in humans arising from the BSE epidemic in cattle in the 1990s, and an epidemic of Severe Acute Respiratory Syndrome due to the SARS-coronavirus in the 2000s. Other communicable diseases have been able to re-emerge due to pathogen evolution (drug resistance) or changes in the host population (e.g. tuberculosis facilitated by HIV). This means that despite improvements in understanding, treatment and prevention, the threat from infectious diseases remains.
What are the characteristics of infectious disease epidemiology?
During the course of this book you have learnt about different study designs, epidemiological and statistical methods. These can just as well be applied to infectious diseases as noninfectious diseases. However, there are some special features of infectious diseases that do not apply to noncommunicable diseases. Communicable diseases can generally be transmitted from person to person, so the incidence of new infections depends on the prevalence of infection (or rather infectious individuals) in the population. Critically treatment or prevention of infection in one person can avert infections in other people. Other important characteristics of infectious disease which distinguish it from noninfectious or chronic disease include:
- immunity – following infection or vaccination individuals may become immune (resistant) to future infections. Some pathogens are strongly immunogenic (e.g. measles infection provokes long-lasting immunity that protects against future infection), others are weakly immunogenic (e.g. gonorrhoea) and therefore people may become infected again;
- carrier state – an individual may be infected and able to infect others without displaying any symptoms of disease;
- urgency – there is sometime a need to act quickly to respond to an outbreak.
Other key features of infectious agents
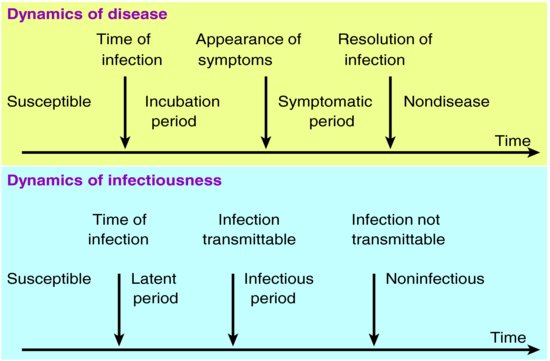
Once a person is exposed to an infectious agent, they may resist infection if they are immune or may become infected. The figure shows dynamics of infection/disease and infectiousness. If they are infected, there is often an incubation period between the time of infection and the time when symptoms develop. This is usually followed by a period of clinical illness with symptoms dependent on the infection although, for some organisms it is possible to have asymptomatic infection (also known as a carrier state). Following infection there is a latent period during which the person infected is not infectious (not able to transmit the disease to others). Following this period, and, depending on the organism, the person may become infectious before, during and / or after the period of clinical symptoms which can pose challenges to the control of disease (Figure 17.1).
Transmission
Infectious diseases can be transmitted by various, and sometimes multiple, means (see below for some examples). Understanding how infections are transmitted is central to developing appropriate and effective control measures (see Table 17.1).
Table 17.1 Modes of transmission and examples.
| Mode of transmission | Example |
| Direct physical contact / transfer of body fluids – touching an infected person, including sexual intercourse | Staphylococcus, gonococcus, HIV, hepatitis B, ebola |
| Inhalation of droplets containing the infectious agent (aerosol) | Tuberculosis, measles, influenza |
| Vertical transmission (mother to foetus) | Hepatitis B, HIV, syphilis, rubella |
| Parenteral – bloodborne through needlestick/injection or transfusion | HIV, hepatitis B, hepatitis C |
| Ingestion of food or water that is contaminated | Salmonella, campylobacter, cholera, vCJD, hepatitis A |
| Vector borne – through animal carrier/zoonosis | Malaria (mosquito), Lyme disease (deer ticks) |
A useful measure of transmissibility (the intrinsic potential for an infectious agent to spread) is the basic reproduction number. Also known as R0, this can be defined as the average number of secondary cases produced by one primary case in a wholly susceptible population. The estimated R0 for influenza is around 2–3, whereas measles has an R0 of around 12–18. Other things being equal, the larger the value of R0, the more difficult the infection is to control. Often, some proportion of the population is not susceptible to the infection because they are immune, so that the number of cases infected by a primary case is less than R0. The actual average number of secondary cases produced by an infectious primary case is known as the effective reproduction number (R).
Occurrence of infectious diseases
If the effective reproduction number, R, is less than one (i.e. each case gives rise to fewer than one secondary case) then the infection cannot persist in the population and will eventually die out. We can reduce R by reducing the number of susceptible people in the population, for example through vaccination. R0 can be used to estimate the proportion of the population that needs to be vaccinated to prevent sustained spread of the infection; this is given by 1 − 1/R0 and is known as the herd immunity threshold. If the vaccination coverage consistently exceeds this threshold then the disease will eventually die out. Herd immunity therefore refers to the proportion of a host population which is immune to an infection, but also relates to the concept that the presence of immune individuals protects those who are not themselves immune.
If R is greater than 1 then the incidence of the disease is increasing in the population giving rise to an epidemic. An epidemic occurs when the incidence of disease, in a given population and during a given period, substantially exceeds the expected incidence. Outbreak is often used interchangeably with epidemic, but is sometimes used more specifically to refer to an epidemic in a geographically or demographically localised population. A pandemic is a worldwide epidemic – as recently occurred in relation to swine flu. An endemic infection is one that occurs regularly in a given population and can be maintained in that population without external influence (i.e. R is around 1). For example, in the UK chickenpox is endemic, malaria is not.
Control of infectious diseases
Interrupting transmission is a key aim of infectious disease control. More specifically, control can be defined as a reduction in the incidence, prevalence, morbidity or mortality of an infectious disease to a locally acceptable level. Elimination refers to a reduction to zero of the incidence of disease or infection in a defined geographical area. Eradication is the permanent reduction to zero of the worldwide incidence of infection (Dowdle, 1998).
To date smallpox is the only infectious disease of humans that has been eradicated (as certified by WHO in 1979), with poliovirus currently being targeted as the second. Vaccines have been highly successful in combating formerly common childhood diseases such as measles and pertussis (whooping cough). Successful immunisation programmes rely upon the availability of safe and effective vaccines, targeted at the age groups at highest risk. High uptake ensures that individuals are protected, but because of herd immunity, it is not necessary to immunise 100% of the population.
The current national routine childhood immunisation schedule in the UK includes vaccines that protect against the following infections:
2 months:
- diphtheria, tetanus, pertussis, polio and Haemophilus influenzae type b (Hib, a bacterial infection that can cause severe pneumonia or meningitis in young children) given as a 5-in-1 single injection known as DTaP/IPV/Hib
- pneumococcal infection
3 months:
- 5-in-1, second dose (DTaP/IPV/Hib)
- meningitis C
4 months:
- 5-in-1, third dose (DTaP/IPV/Hib)
- pneumococcal infection, second dose
- meningitis C, second dose
between 12 and 13 months:
- meningitis C, third dose
- Hib, fourth dose (Hib/MenC given as a single jab)
- MMR (measles, mumps and rubella), given as a single jab
- pneumococcal infection, third dose
3 years and 4 months, or soon after:
- MMR second jab
- diphtheria, tetanus, pertussis and polio (DtaP/IPV), given as a 4-in-1 pre-school booster
around 12–13 years:
- cervical cancer (HPV) vaccine, which protects against cervical cancer (girls only): three jabs given within six months
around 13–18 years:
- diphtheria, tetanus and polio booster (Td/IPV), given as a single jab
In addition, the elderly and those at high risk are offered seasonal influenza vaccine each year.
There are many infections for which vaccines are not currently available so disease control measures must therefore rely on other ways of interrupting transmission. Returning to R0, the factors influencing the basic reproduction number and potential control measures targeting these factors are shown in Table 17.2, illustrated using the example of sexually transmitted infections.
Table 17.2 Factors influencing basic reproduction number for an STI and potential control measures targeting these factors.
| Factors influencing R0 | Potential control measures |
| R0 = probability of effective contact | Condoms, acyclovir (treatment for herpes simplex virus), anti-retroviral therapy |
| x number of contacts | Education, negotiating skills |
| x duration of infectiousness | case ascertainment (screening, partner notification), treatment, compliance, accessibility of services |
Surveillance of infectious diseases
Public health surveillance refers to the ongoing, systematic collection, analysis and interpretation of data essential to the planning, implementation, and evaluation of public health practice, closely integrated with the timely dissemination of these data to those responsible for prevention and control. Put more simply, surveillance provides information for public health action.
Clearly it is not possible or desirable to monitor all infections, but some infectious diseases are deemed important enough to be included in national and international surveillance systems. The criteria that are applied to determine this ‘importance’ include:
- Is it an important public health problem, for example because of high mortality/morbidity or significant epidemic potential?
- Is the disease amenable to public health action?
- Is it feasible to undertake surveillance – is the relevant information available?
We undertake surveillance to monitor trends including the identification of outbreaks, to guide immediate public health action such as outbreak control, to guide the planning, implementation, and evaluation of programmes to prevent and control disease and to evaluate public health policy.
In the UK statutory notifications are a key source of surveillance information. Clinicians have a legal requirement under public health legislation to notify, on suspicion, each case of a notifiable disease. The current list of notifiable infectious diseases in the UK is given In Box 17.1.
Other key sources of surveillance information include laboratory reports, voluntary reports from clinicians, hospital activity data, general practice consultations and vaccination coverage data, as well as epidemiological studies. Enhanced surveillance systems are sometimes established for diseases of particular public health importance. These systems collect a more detailed set of information on each case in order to characterise better the distribution or infection or behavioural risk or in response to a new or emerging problem to improve our understanding of it or to monitor a new vaccination programme. For example, enhanced surveillance has been established for syphilis, hepatitis B, TB, and severe group A streptococcal disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree