2 Infectious disease
Approach to the patient with a suspected infection
• Management
Returning travellers (Table 2.1)
There are number of common illnesses that occur only in certain areas. The history should cover all recent travel. Most tropical illnesses are uncommon in the countries in which they occur; upper respiratory tract infections, urinary tract infections and viral infections are still common worldwide. However, some illnesses, such as malaria or dengue, are common. WHO advises that fever occurring in a traveller 1 week or more after entering a malaria risk area and up to 3 months after departure is a medical emergency because of the mortality associated with Plasmodium falciparum, though there have been well-reported cases of falciparum infection occurring after 3 months. Viral haemorrhagic fevers are also seen in patients returning from endemic areas, though these are very rare infections. Websites are a useful source of up-to-date information on geographic medicine and epidemics (e.g. www.cdc.gov/travel/destinat.htm).
Table 2.1 Causes of febrile illness in travellers returning from the Tropics and world-wide
| Developing countries | Specific geographical areas (see text) |
|---|---|
| Malaria | Histoplasmosis |
| Schistosomiasis | Brucellosis |
| Dengue | World-wide |
| Tick typhus | Influenza |
| Typhoid | Pneumonia |
| Tuberculosis | Upper respiratory tract infection |
| Dysentery | Urinary tract infection |
| Hepatitis A | Traveller’s diarrhea |
| Amoebiasis | Viral infection |
Fever of unknown origin (FUO)
Systemic multi-system infections
Sepsis
Management
Sepsis and septic shock should be treated urgently, as should the bacterial cause of the infection.
Meningococcal septicaemia
Presentation is with the classic triad of headache, fever and neck stiffness, though this is not always the case (p. 54). Septicaemia causes septic shock with fever, myalgia and hypotension, and may be accompanied by a petechial or haemorrhagic rash. The case fatality rate is approximately 10%.
Management (Box 2.1)
Start antibiotics immediately.
Box 2.1 Meningococcal meningitis and meningococcaemia emergency treatment
Suspicion of meningococcal infection is a medical emergency requiring treatment immediately
Immediate treatment for suspected meningococcal meningitis at first contact before transfer to hospital or investigation
Malaria
Diagnosis
Management of uncomplicated falciparum malaria
The treatment of malaria varies, depending on the resistance patterns to antimalarial chemotherapy and will vary over time. Up-to-date advice should be sought if there are doubts as to the appropriate therapy. There is very little chloroquine-sensitive falciparum malaria. Treatments for uncomplicated falciparum malaria are shown in Table 2.2.
Table 2.2 Drug treatment of uncomplicated malaria in adults
| Type of malaria | Drug treatment |
|---|---|
| Plasmodium vivax, P. ovale, P. malariae | Chloroquine 600 mg 300 mg 6 hours later 300 mg 24 hours later 300 mg 24 hours later |
| P. falciparum (almost all are resistant to chloroquine) | Quinine 600 mg 3 times daily for 7 days Plus Doxycycline 200 mg once daily for 7 days Or Clindamycin 450 mg 3 times daily for 7 days (Fansidar (SP) (pyrimethamine and sulfadoxine) 3 tablets as single dose with or following quinine) Or Malarone 4 tablets daily for 3 days Or Riamet (artemether with lumefantrine) 4 tablets 12-hourly for 3 days |
| Alternative therapy | |
| Artesunate-mefloquine 12/25 mg/kg daily for 3 days Or Dihydroartemisinin/piperaquine 6.3 mg/kg daily for 3 days |
Management of severe falciparum malaria (Box 2.2)
Management of non-falciparum malaria
Non-falciparum malarias can be treated with oral chloroquine 600 mg, then 300 mg after 8 hours, then 300 mg daily for 2 days. There is some reported chloroquine-resistant malaria in Papua New Guinea and treatment can be with riamet or malarone (dosages in Table 2.2). P. vivax and P. ovale have hypnozoites that may persist and cause a recurrence of infection many years later. Patients with vivax or ovale infection should receive primaquine 15 mg daily for 2–3 weeks following successful treatment, to eradicate hepatic hypnozoites and prevent relapse. Anyone who is about to receive primaquine should have their glucose-6-phosphate dehydrogenase (G6PD) status checked, as primaquine use is associated with haemolysis in patients with G6PD deficiency (p. 216). WHO guidelines www.who.int/topics/malaria/en.
Prevention of malaria
Dengue
Investigations
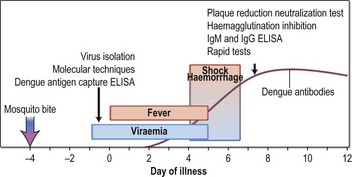
Investigations show a low platelet count, normal white cell count and sometimes mildly abnormal liver biochemistry. See Figure 2.2 for the course and timing of diagnosis.
Plague
Clinical features
Clinical manifestations of plague are bubonic, septicaemic, pneumonic, pharyngeal and meningitis.
Brucellosis
Clinical features
The onset is insidious, with an incubation period about 2–4 weeks. Symptoms are initially non-specific, although specific ones include an ‘undulant’ fever, malodorous sweat and a peculiar taste in the mouth. Brucellosis can affect nearly any organ of the body and includes lymphadenopathy, hepatosplenomegaly, sacro-iliitis, arthritis, osteomyelitis and meningoencephalitis. Chronic brucellosis can last over a year. Symptoms may also recur over long periods.
Investigations
Listeriosis
Clinical features
Q fever
Infection with the obligate intracellular pathogen Coxiella burnetii, which is widespread in many animals, is the cause of Q fever. Transmission to humans is usually via dust, aerosol and unpasteurized milk; spore formation means that the infection can remain in the environment for long periods.
Lyme disease
There are three stages of Lyme infection:
Treatment
Visceral leishmaniasis
Visceral leishmaniasis (kala-azar) is caused by Leishmania donovani, L. infantum or L. chagasi, and is present in India, Asia, Africa, the Mediterranean and South America. In central India, humans are the main host and the disease occurs in epidemics. In most other areas, it is a zoonosis; the main animal reservoirs are dogs and foxes, although in Africa it is carried by rodents. Visceral leishmaniasis is a common opportunistic infection of advanced HIV disease in Mediterranean coastal regions.
Diagnosis
Epstein–Barr virus (EBV)
Clinical features
Skin and soft-tissue infections
Meticillin-resistant Staph. aureus (MRSA)
Treatment
Treatment of MRSA infection depends on the source of the infection and the sensitivity of the MRSA.
Staphylococcal toxic shock syndrome (TSS)
In the early 1980s, most cases of TSS were in menstruating females and associated with retained tampons. Recently, TSS has been less often associated with menstruation.
Post-streptococcal syndromes
Rheumatic fever
• Treatment
Other post-streptococcal syndromes
Necrotising skin and soft-tissue infections
Bite wounds
Varicella zoster virus (VZV) infection
Shingles is a secondary reactivation of latent VZV infection in the distribution of one or sometimes two dermatomes. The vesicles of shingles are identical to those in chickenpox. Shingles mainly affects the elderly but can occur at any age. Post-herpetic neuralgia may occur after herpes infection and causes severe debilitating pain. Shingles involving the ophthalmic division of the trigeminal nerve has a high rate of complications. Disseminated shingles infection can occur in the immunosuppressed patients (particularly in late HIV infection), when the rash is seen over many dermatomes and appears similar to chickenpox. Shingles lesions may transmit infection to non-immune individuals.
Treatment
Respiratory infections
Upper respiratory tract infections
Pharyngitis
Epiglottitis
Sinusitis
Otitis media
Diphtheria
Lower respiratory tract infections
Influenza
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree