4 Infections and antibiotics
Importance of infection
In the latter half of the 19th century Louis Pasteur hypothesized that bacteria caused infection by being carried through the air (germ theory of disease). Aware of Pasteur’s work, in 1865, Joseph Lister first used carbolic acid (phenol) as a spray in the operating theatre to successfully prevent and treat infection in compound fractures. In the early part of the 20th century, with the advent of sterilized instruments, surgical gowns and the first rubber gloves, antisepsis was replaced by modern aseptic surgical techniques which were championed by Birmingham surgeon Robert Lawson Tait. Penicillin was discovered by Alexander Fleming in 1928 and first used clinically in 1940 by Howard Florey. The prevention and treatment of surgical infection was further transformed by the many different classes of antibiotics that were discovered through the latter part of the 20th century. Nevertheless, control of infection in surgical practice remains an important and challenging issue due to the emergence of antibiotic-resistant organisms and the rise in the numbers of elderly, co-morbid and immunocompromised patients undergoing increasingly complex surgical interventions that frequently involve the use of implants. The risk of infection is related to the type of surgery (Table 4.1). Postoperative infections impact on patient outcomes and increase the length of hospital stay, which in turn increases the cost of surgery. In the UK, there is now a legal duty on hospitals to do all they can to minimize the risk of healthcare associated infections (HCAI) in patients.
Table 4.1 Classification of operative wounds and infection risk with prophylaxis
| % Infection rate with prophylaxis* | |
|---|---|
| Clean (e.g. non-traumatic wound, respiratory / gastrointestinal /genitourinary tracts intact) | 0.8 |
| Clean-contaminated (e.g. non-traumatic wound, respiratory / gastrointestinal /genitourinary tracts entered but insignificant spillage) | 1.3 |
| Contaminated (e.g. fresh traumatic wound from dirty source, gross spillage from gastrointestinal tract or infected urine/bile or major break in aseptic technique) | 10.2 |
* Based on data from: Olson M, O’Connor M, Schwartz ML. Surgical wound infections. A 5-year prospective study of 20,193 wounds at the Minneapolis VA Medical Center. Ann Surg. 1984 Mar;199(3):253–259.
Biology of infection
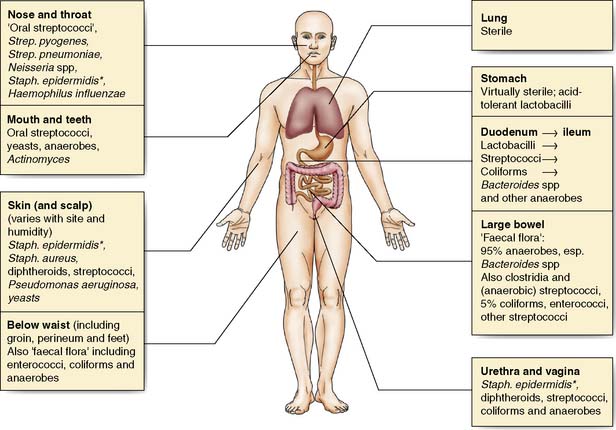
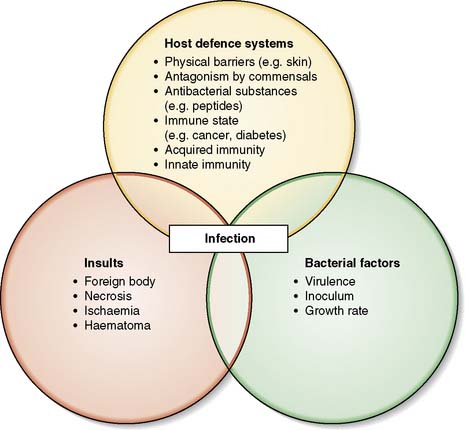
Many body surfaces are colonized by a wide range of micro-organisms, called commensals, with no ill effects (Fig. 4.1). However, once the normal defences are breached in the course of surgery, such as skin (e.g. Staphylococcus aureus) and bowel (e.g. Bacteroides spp. and Escherichia coli) commensals can then cause infection. Infection is defined as the proliferation of micro-organisms in body tissue with adverse physiological consequences. The factors involved in the evolution of infection are shown in Figure 4.2.
Host defence systems
A number of host factors make infection more likely:
• Old age, obesity, malnutrition, cancer and immunosuppressive agents (e.g. steroids) and diabetes
• The presence of dead tissue; for example, burned flesh or haematoma provide a rich source of nutrients for bacteria and hamper the local immune response
• Poor vascularity; in the leg this is often associated with peripheral arterial disease and diabetes
• Foreign material present in tissues either as a result of trauma (e.g. broken glass, clothing, shrapnel) or surgical procedure (e.g. joint replacements, heart valves, vascular prostheses).
Preventing infection in surgical patients
Preoperative MRSA screening
Since 2008 hospitals in England have been required to screen all elective surgical patients for methicillin-resistant Staphylococcus aureus (MRSA). Carriers receive decolonization treatment (nasal mupirocin cream and antiseptic skin wash) and appropriate antibiotic prophylaxis, usually a glycopeptide antibiotic (e.g. teicoplanin) prior to surgery. This policy reduces MRSA transmission in surgical wards (EBM 4.1). Screening for nasal carriage of Staphylococcus aureus followed by decolonization also reduces surgical wound infection (EBM 4.2). These hospitals now screen emergency admissions although the timing of available results will determine whether this has an impact on management and outcomes.
Hardy K, et al. Reduction in the rate of methicillin-resistant Staphylococcus aureus acquisition in surgical wards by rapid screening for colonization: a prospective, cross-over study. Clin Microbiol Infect. 2010; 16:333-9.
4.2 Preventing surgical site infections in nasal carriers of Staphylococcus aureus
Bode LG, et al. Preventing surgical-site infections in nasal carriers of Staphylococcus aureus. N Engl J Med. 2010; 362:9-17.
Hand decontamination
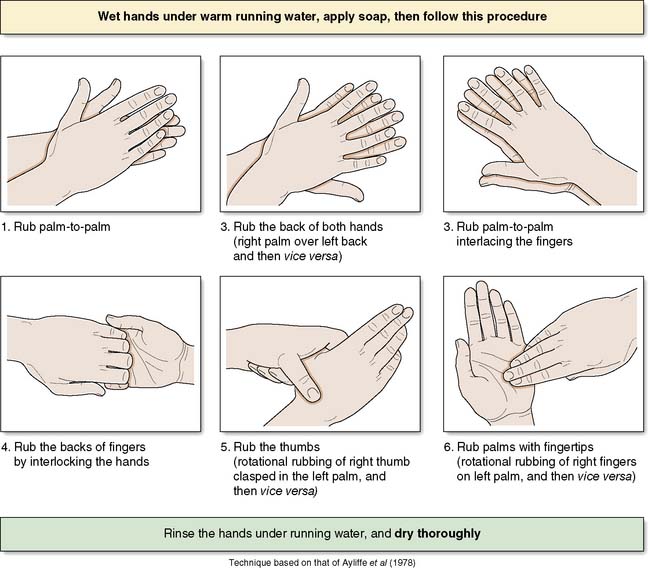
The operating team should wash their hands prior to each operation on the list using an aqueous antiseptic surgical solution, with a single-use brush for the nails. The ‘six-step hand hygiene technique’ is now widely adopted (Fig. 4.3). Hospitals will have policies for which antiseptic agents are used. Where hands are not soiled, alcohol hand gel is a suitable alternative for decontamination on the wards.
Surgical instruments
Terminology
• Decontamination: a process which removes or destroys infectious or unwanted material
• Cleaning: the physical removal of soil and organic matter
• Disinfection: the removal or destruction of some micro-organisms but not bacterial spores
• Sterilization: the complete destruction of all micro-organisms including spores.
Creutzfeldt–Jakob disease (CJD) and other prion diseases
Summary Box 4.1 Prevention of infection
• Preoperative screening of patients for MRSA, and subsequent decolonization of carriers, is now an integral part of surgical care in UK hospitals
• The routine practices of hand washing, surgical scrub, skin preparation of the patient and maintaining a sterile field are collectively known as ‘aseptic technique’
• The practice of aseptic technique is an important component in preventing surgical site infections
• Sterility of surgical instruments is critical to preventing cross-infection. This may be achieved by decontamination of instruments in SSDs or by using sterile, disposable instruments.
Prophylactic use of antibiotics
Antibiotic prophylaxis is defined as their use before, during, or after a diagnostic, therapeutic, or surgical procedure to prevent infectious complications. The evidence base and guidance can be found at www.sign.ac.uk/pdf/sign104.pdf and in the British National Formulary (BNF).