Incapacitating Agents: BZ, Calmative Agents, and Riot Control Agents
Yedidia Bentur
John Gomez
3-QUINUCLIDINYL BENZILATE OR BZ
NAME AND DESCRIPTION OF AGENT
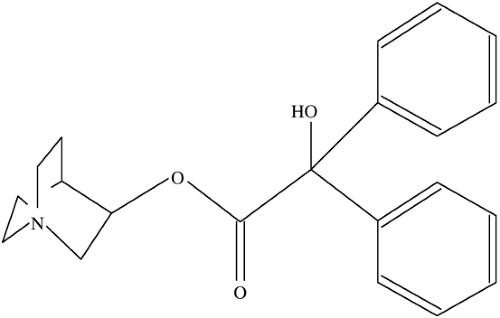
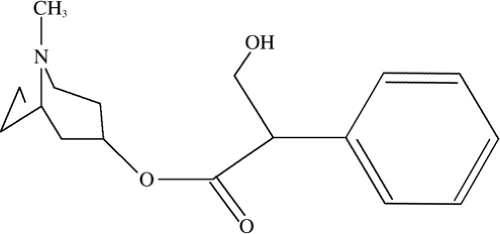
3-Quinuclidinyl benzilate, code named by the Army and widely known as BZ (or QNB), is a potent centrally acting glycolic acid ester anti-cholinergic. It has effects very similar to atropine, but it is much more potent in the central nervous system (CNS) and has a very long duration of action. It is primarily dispersed by aerosol or smoke-producing munitions, and the route of exposure is primarily respiratory. The British reportedly have a similar agent, known only as Agent 15. BZ was first tested commercially as a gastrointestinal antispasmodic, but when the extreme CNS effects were noted, civilian therapeutic research was abandoned. The U.S. Army conducted experiments from the 1960s to the 1980s with various anticholinergics and found BZ to be the most effective (1,2,3) The ICt50 (airborne concentration of BZ necessary to incapacitate 50% of exposed and unprotected individuals through inhalation during a set time period) is approximately 100 mg.min/m3 (Figs. 5-1, and 5-2).
THEORETICAL AND SCIENTIFIC BACKGROUND
The use of incapacitating agents is not limited to the 20th century. Instances of biologic and chemical warfare have been recorded in ancient times. Various alkaloid anticholinergics were used as early as 200 B.C. The infamous Roman enemy and Carthaginian General Hannibal used mandrake root to intoxicate or “incapacitate” rebel African tribes (3,4,5). A well-reported use of a belladonna (atropine-like) alkaloid was by the Bishop of Muenster who in 1672 used projectiles and grenades containing belladonna during his attack on the city of Groningen. Shortly after this occurrence in 1675, the French and Germans signed the first known treaty outlawing the use of chemical weapons (1,3,6).
The first recorded use of an incapacitating anti-cholinergic substance in the 20th century occurred in 1908 when a French unit in present-day Vietnam were poisoned with Datura placed in their evening meal. Several of the soldiers exhibited classic signs of anti-cholinergic delirium but recovered uneventfully (3,6). The former national Yugoslavian army was known to have weaponized and stockpiled BZ. There has been speculation that BZ was used during the conflict in Bosnia. In July of 1995, a contingent of a group of 15,000 people attempting to walk to Srebrenica reportedly
suffered from hallucinations after an attack from Serbian forces using an unknown gas (7). There are also allegations that Serbian forces used BZ against Kosovo Liberation Army forces near the Albanian border. Iraq is suspected to have developed an agent similar or identical to BZ.
suffered from hallucinations after an attack from Serbian forces using an unknown gas (7). There are also allegations that Serbian forces used BZ against Kosovo Liberation Army forces near the Albanian border. Iraq is suspected to have developed an agent similar or identical to BZ.
An incapacitating agent may be defined as a chemical that is temporary in its duration, is nonlethal, and has no permanent sequelae. From a military standpoint, an ideal incapacitating agent would be odorless, colorless, easily dispersed, and last a few hours to days, but longer than a few minutes as seen with the riot control agents. This substance should inhibit the cognitive functions of an enemy, keeping them from performing their task, and be easily dispersible, but still have a large margin of safety. It should be potent, and have an effective antidote known only to the user. Numerous agents were studied by the U.S. Army for this purpose, including atropine, scopolamine, lysergic acid diethylamide (LSD), phenothiazines, and delta-9 tetrahydrocannibinol (THC) (2). BZ offers several advantages over atropine and scopolamine as an incapacitating agent. BZ is said to have a very high safety profile and has 25 times more CNS anticholinergic potency than atropine (8). The incapacitating dose is defined to be roughly 0.5 mg in a typical adult compared to doses 20 to 25 times that for atropine. In addition, BZ also has less peripheral antimuscarinic effect than atropine, which makes it safer, and it is easier to weaponize/disperse. The onset of action is approximately one hour, and it peaks at about 8 hours, often persisting for 3 to 4 days (1,3,8).
Acetylcholine plays a vital role in cognitive function. This is why new centrally acting acetylcholinesterase inhibitors have been developed to improve memory and general cognitive function in patients with Alzheimer’s dementia. Blockade of muscarinic receptors by BZ results in profound CNS dysfunction.
SIGNS AND SYMPTOMS
BZ crosses the blood brain barrier effectively and produces symptoms within 2 hours. Because of its ready penetration across the blood brain barrier, the predominant effects are CNS symptoms. Patients will have anticholinergic delirium and frequently will not be able to report many symptoms. If they are coherent enough to give a history, they may report hallucinations, peripheral effects including dry mouth, visual symptoms such as blurriness and inability to focus, as well as a feeling of warmth (1,3).
The symptoms of anticholinergic delirium range from a mild delirium to full-blown coma. At the mild end of the spectrum when a victim has received only a minimally effective dose, symptoms might include poor judgment, somnolence, impaired speech, and difficulty with complex task assignment. The more severely poisoned victim may manifest severe hallucinations from sensory stimuli, and agitation and even seizures. Consistent with the definition of delirium, there may be waxing and waning of the symptoms with occasional lucid intervals (1,3).
Anticholinergic delirium includes a few unique characteristics that may help identify poisoning with BZ. Patients may exhibit bizarre grasping movements where they may pick at the air, their skin, or clothing. The term “woolgathering” was once used to describe this peculiar feature. Shared hallucinations are described between two patients with anticholinergic delirium who are placed in the same room. Vivid hallucinations may occur that can be visual, auditory, or sometimes tactile. These undergo slow extinction as the CNS symptoms abate (1,3).
Like other anticholinergics, BZ can cause peripheral signs and symptoms; however, they may not be as pronounced as one would expect with the typical belladonna alkaloids such as atropine or Jimson weed (Datura strammonium), for example. Patients may manifest features of the classic anticholinergic toxic syndrome: “dry as a bone, red as a beet, hotter than Hades, and blind as a bat.” Sinus tachycardia, mydriasis, flushed, dry warm skin, and diminished bowel sounds, hyperthermia, and urinary retention may be present. Seizures may occur in severe poisoning. It is important to note that pupillary dilatation may be mild or even absent at doses capable of causing delirium. BZ also causes fewer peripheral symptoms than other anticholinergic drugs. Absence of these symptoms, especially early in the course of the exposure, is not uncommon (3).
MEDICAL MANAGEMENT
Much like any other biologic or chemical warfare attack agent, treatment is contingent upon proper diagnosis and maintaining a high index of suspicion. An isolated exposure to BZ would not be expected, making the diagnosis more difficult. The combination of peripheral antimuscarinic effects described previously with the characteristic delirium suggests the diagnosis. Laboratory examinations are not clinically useful. They assist in ruling out other potential causes (such as metabolic derangements) and in diagnosing possible complications such as rhabdomyolysis and renal failure. Serum levels can be obtained from specific reference laboratories, although they are not helpful in the acute settings.
Patients with exposure to BZ should be decontaminated as soon as possible. All clothing should be removed and placed in sealed plastic bags. Skin should be thoroughly rinsed with copious amounts of water to prevent possible ongoing absorption. Staff members should be trained to prevent contamination of this potent agent.
Supportive care is paramount and intuitive. Delirious patients can certainly be a danger to themselves and others if not properly monitored. Victims should be temporarily restrained if necessary, and parenteral benzodiazepines should be used to control agitation. Although such sedatives are not specific antidotes, they can be useful measures to implement in an agitated patient and to decrease heat production.
Hyperthermia is an important concern due to the inability to sweat and increased psychomotor agitation. The patient’s rectal temperature should be monitored closely to prevent the potential dangerous complications. Hyperthermic patients should be cooled rapidly by misting the patient with water and then applying fans for evaporation, or by implementing other effective techniques. Cold ice packs are not thought to be effective for this form of hyperthermia.
Anticholinergic agents cause drying of the secretions, and along with tachycardia mistakenly lead the treating physician to believe there is significant volume depletion when the patient is actually euvolemic. Hydration status and urine output should be closely monitored, particularly in
warm weather (1,8). As with many stimulants and drugs of abuse, patients are at risk for rhabdomyolysis.
warm weather (1,8). As with many stimulants and drugs of abuse, patients are at risk for rhabdomyolysis.
Acetylcholinesterase inhibitors are a classic but much maligned antidote for antimuscarinic poisonings. Neostigmine, pyridiostigmine, and physostigmine are all known as medicinal carbamates. They act by inhibiting the breakdown of acetylcholine at the synapse, increasing its level, and overcoming the blockade by competitive displacement. Unlike the other two agents listed, physostigmine has a tertiary amine group enabling it to cross the blood brain barrier. Due to its CNS penetration, it is the cholinesterase inhibitor of choice for delirium caused by BZ. There is controversy concerning the use of physostigmine due to reported adverse effects such as seizures and asystole (9,10,11,12). Wide use of physostigmine in the 1970s and 1980s for undifferentiated toxic delirium or coma was felt to be the cause of these reports of complications. Ketchum reports on military studies that show the safety and efficacy of physostigmine in the treatment of BZ-induced delirium (3). Other studies have showed the safety of physostigmine when used in patients with anticholinergic toxidrome who have not ingested drugs with fast sodium channel blocking activity such as tricyclic antidepressants (9,10,11,12). Some clinicians are still reluctant to recommend physostigmine use in this setting. However with BZ, it appears that physostigmine is safe and appropriate.
A typical adult dose of physostigmine would be 1 to 2 mg, IM or IV. The recommended pediatric dose of physostigmine is 20 μg/kg, up to 0.5 mg over 5 minutes. The dose may be repeated. Slow IV push over 5 to 10 minutes reportedly lowers the incidence of seizures and cardiac effects. All patients should have an electrocardiogram (ECG) prior to administration to check the QRS and PR width, and ECG monitoring is recommended. A QRS duration >100 milliseconds and a PR interval >200 milliseconds are contraindications to administration. Possible co-ingestions of tricyclic antidepressants or phenothiazines are relative contraindications, although this is highly unlikely in a suspected BZ exposure (8,9,13).
Physostigmine reversal of symptoms in BZ poisoning may not be immediate for reasons that are not completely understood (3). Once symptom reversal has been obtained, a similar dose should be repeated every 6 hours to prevent relapse. Much higher doses may be required for reversal of severe delirium. In one subject exposed to BZ, a total of 200 mg of physostigmine was given without the occurrence of adverse events (3). Oral dosing is also effective and is an option once the patient has been stabilized. Patients should be admitted for observation for 24 to 36 hours.
TRIAGE CONSIDERATIONS
When evaluating patients with suspected or known BZ poisoning, rapid triage of those with severe agitated delirium for safety issues is important. Those with hyperthermia, severe delirium, or seizures should intuitively take first priority in a mass exposure situation.
PERSONAL PROTECTION
Routine universal precautions should be used, including mask and eye goggles, a long sleeve gown and gloves to prevent contamination.
BZ Summary
BZ is a potent centrally acting anticholinergic
Anticholinergic delirium is the hallmark of BZ exposure; peripheral antimuscarinic effects may be delayed or less prominent.
Diagnosis is historical, epidemiological, and clinical.
Decontaminate all suspected patients, wear appropriate protective clothing.
Restrain patients to protect them from harm when necessary, using loose netting. Use benzodiazepines liberally.
Treat hyperthermia aggressively; monitor for rhabdomyolysis.
The treatment of choice for patients with significant intoxication is physostigmine 30 to 45 μg/kg IV/IM.
SEDATIVE OR CALMATIVE AGENTS
NAME AND DESCRIPTION OF AGENTS
Opioids and volatile anesthetics are potential sedative or calmative agents. Opioids have been used for analgesia for over 100 years. Intuitively, opiates can serve as calmative and/or incapacitating agents. Morphine’s tendency to cause severe respiratory depression, as well as other side effects and logistical concerns limit its use in this capacity. In this section, we will discuss fentanyl and n-4-substituted fentanyl derivatives used as incapacitating agents.
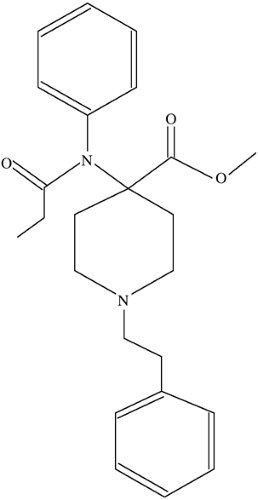
Carfentanil is an n-4 substituted fentanyl derivative that has high potency and a high therapeutic index (Figs. 5-3 and 5-4). Its safety has been well studied in large animal models, when used to immobilize wildlife. Other similar drugs in its class include sufentanil, alfentanil, and remifentanil. A detailed discussion follows later in the chapter.
Halothane is an example of an anesthetic gas that can also be considered as a potential calmative agent. However, its odor and safety profile may be of concern in this capacity.
THEORETICAL AND SCIENTIFIC BACKGROUND
The first and only reported modern use of a sedating incapacitating agent occurred in Russia. In late October of 2002, Chechen rebels took 800 civilian hostages attending a stage show. The rebels were armed with explosives and threatened to blow up themselves and their captives. A few days later, Russian special forces used a calmative gas to subdue the rebels and take control of the crisis. Victims were taken to local Moscow hospitals. In the tragic aftermath of the situation, 646 people were treated in local hospitals, and 118 of the victims died (16).
The victims were found to have signs and symptoms of opiate toxicity (15,16). After significant pressure from the families of the victims, the Russian government released a statement claiming that the gas used was a derivative of fentanyl.
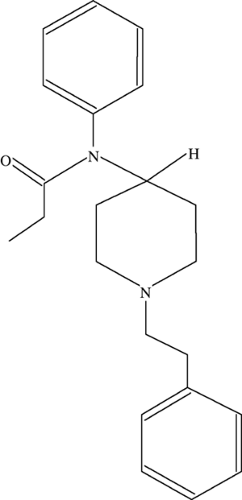 Figure 5-4. Fentanyl
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|