Chapter 38 Plants in African traditional medicine—some perspectives
TRADITIONAL MEDICINE PRACTITIONERS AND THEIR TECHNIQUES
The practitioners of TM in Africa include herbalists, herb sellers, traditional birth attendants, bone setters, diviners, faith healers, traditional surgeons, spiritualists and others. The training of these practitioners is still by an apprenticeship of about 7 years minimum. The content of such training is not standardized. The techniques used in African TM derive from the basic understanding of the aetiology of disease, as conceived by traditional medical practitioners (TMPs), who believe that diseases arise not only from physical ailments and psychological causes (as in Western medicine) but also from astral influences, spiritual causes (due to evil thoughts and machination by enemies), esoteric causes (i.e. originating from the soul or caused by deeds of an individual before reincarnation). Because TMPs in Africa place so much emphasis on supernatural forces, they are consulted not only for sickness but also when misfortunes occur in the family or to an individual, as many such evil omens are ascribed in Africa to supernatural forces. TMPs observe their patients for symptoms and signs but do not perform any pathological examination because they lack training in such techniques. Diagnosis of the disease is made through anamnesis—observation of the patient for signs and symptoms, including visual examination, clinical examination, biological examinations (such as tasting of urine for the presence of sugar in the case of diabetics, or allowing the patient to urinate on the ground and watching for infestation by ants, smelling of sores for putrefaction etc.), divination, which can be by throwing of seeds (Sofowora, 2008) or bones, use of mind-changing plant drugs, use of astronomical signs and analysis of dreams. Although many of these methods can be utilized by TMPs, specializations do occur. The practitioners also refer patients to one another in appropriate cases.
Treatment types in African traditional medicine
Medicaments intended for internal and external application involve the use of vegetable organs (leaves, barks, roots, etc.), latex, resin, etc. Whole or parts of animals (snail, bone, etc.) and mineral substances (alum, kaolin, etc.) are also used. Although the medicine prescribed may contain only a single active item, it is often a multi-component mixture, some of the components of which act as preservatives, flavours or colouring agents. The multi-component preparation also contains ingredients for all the ailments (or symptoms) that need to be removed to restore the patient’s balance. In this way, African TM differs from Western medicine, where a patient can receive a prescription of various tablets, capsules, mixtures along with other dosage forms to eradicate a reported case of illness. The medicaments used in African TM can be administered in the form of a liquid (decoctions, oily mixtures, etc.), solid (powders, ointments), semi-solid (balsams, etc.) or gas (steam inhalation, incense, etc.). The only route of drug administration that is absent in TM in Africa is the intravenous (i.v.) route. The other routes are employed though in rather crude forms.
Ethnopharmacological themes, as illustrated by sub-Saharan art objects and utensils, have been discussed in an illustrated article by De Smet (1998).
Scientific evidence supporting some practices and remedies in African traditional medicine
Plants of Ageratum conyzoides L. collected at night are used to treat children who cry too often for no known cause, especially at night. Night collection of this herb is particularly indicated when the frequent crying is suspected to be due to the influence of witchcraft, or to persistent disturbance from the spirits of the child’s playmates (dead or alive), thus requiring the use of the ‘occult’ power of the herb. The following procedure is followed: A suitable location of A. conyzoides is found during the day. Very late at night, the collector approaches the plant and chews nine or seven seeds (for male or female, respectively) of melegueta pepper (Aframomum melegueta K. Schum.). The chewed grains are spat on the plant while the appropriate incantations are recited. The plant is then plucked and warmed over a fire at home before the juice is expressed. Palm oil (expressed from the mesocarp of Elais guiniensis family, Palmaceae) is added to the pressed juice and the mixture used to rub the whole body of the patient. Ageratum conyzoides is commonly used in TM for dressing wounds and ulcers, for scabies and as an eyewash. It is used as a styptic in East Africa (Kokwaro, 1993). These common uses result from its antimicrobial properties, which have been demonstrated scientifically but the special effect (occult power) it is claimed to possess when collected at night cannot easily be rationalized on a scientific basis, especially when there is no precise diagnosis of the disease. There are, however, other practices in African TM that are justifiable scientifically. Some examples are given below.
In many African homes, teeth are cleaned in the morning by chewing the root or slim stem of certain plants until they acquire brush-like ends. The fibrous end is then used to brush the teeth thoroughly. These chewing sticks impart varying taste sensations: a tingling, peppery taste and numbness is provided by Zanthoxylum zanthoxyloides Waterman (Fagara zanthoxyloides Lam.) root, a strong bitter taste and frothing by Masularia acuminata (G. Don.) Bullock ex Hoyle stem, and an initial bitterness becoming sweet later by Vernonia amygdalina Del. root. The root of Terminalia glaucescens Planch. produces a discoloration of the mouth. The most popular chewing sticks are those with a good flavour and texture, and a recognized effect on the teeth and supporting tissues. Freshly cut specimens are always desirable because they are more easily chewed into a brush. Some of them, however, possess such tough fibres that they penetrate the gums during use, thus causing some discomfort (Sofowora, 2008).
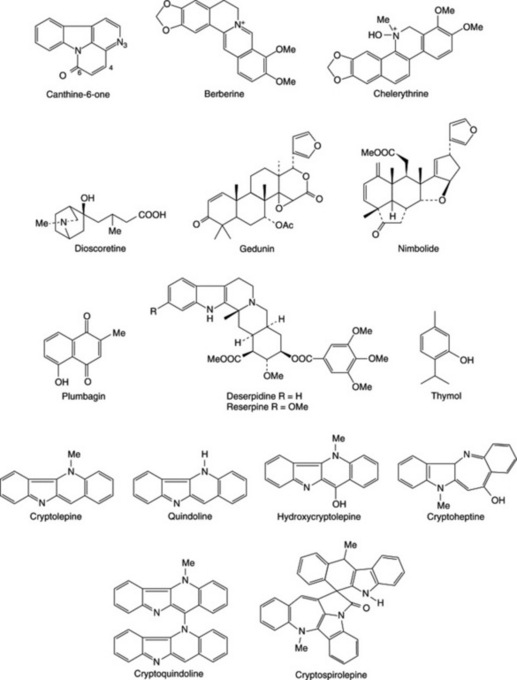
Buffered extracts of the common chewing sticks show antimicrobial activity against oral microbial flora but to varying degrees (Sote and Wilson, 1995; Taiwo et al., 1999; Almas, 2002; Ndukwe et al., 2005). Some African chewing sticks are also reported to contain fluoride ions, silicon, tannic acid, sodium bicarbonate and other natural plaque-inhibiting substances that can reduce bacterial colonization and plaque formation. The antimicrobial activity of the most effective (Z. zanthoxyloides) was shown to be due to berberine, chelerythrine and canthine-6-one (Fig. 38.1), which are most active at pH 7.5 (or during tooth decay) and simple benzoic acid derivatives, which are most active around pH 5 (or after an acid drink like lime juice). These data indicate that the chewing sticks, in addition to providing mechanical stimulation of the gums and removing food particles from the teeth crevices, also destroy oral microbes. Some African chewing sticks have been reported to contain fluoride ions, although their fluoride content was considered insufficient to produce a significant increase in the fluoride content of the dental enamel. Plant parts used as chewing sticks also have been shown to contain not only fluoride but also silicon, tannic acid, sodium bicarbonate and other natural plaque-inhibiting substances that could reduce bacterial colonization and plaque formation (Ogunmodede, 1991; Sote and Wilson, 1995; Taiwo et al., 1999; Almas, 2002; Ndukwe et al., 2005).
The following are the summarized results from a few examples of the investigations carried out to prove the efficacy claimed for medicinal plants used in African TM.
Dioscorea dumetorum (Kunth) Pax tubers are used in African TM, in carefully regulated doses, for the management of diabetes mellitus (Iwu, 1993). Crude extracts of the tuber were shown to possess a hypoglycaemic effect in normal rats and rabbits and were checked for hypoglycaemia produced by alloxan. From the active aqueous fraction, dioscoretine (Fig. 38.1) was characterized as the hypoglycaemic agent by using bioassay-guided fractionation of the extract. Of the solvent fractions tested for toxicity, the aqueous fraction used in TM was the least toxic LD50 = 1400 mg kg−1. Further work has been recommended by the researchers before dioscoretine or the extract of the tuber can be exploited commercially as careful control of the dosage was found necessary even by TMPs.
Polygala nyikensis is used by the highlanders of Malawi and bordering countries to treat various skin problems of fungal origin. The root of the plant was recently shown to exert its antifungal activity owing to the presence of xanthones (Marston et al., 1993).
Azadirachta indica leaves and stem bark are used in treating malaria and have been shown to be effective in vitro and in vivo. Rochanankij et al. (1985) associated the antimalarial activity with nimbolide while Khalid and Duddeck (1989), using a bioassay-directed purification procedure, named another limonoid, gedunin (Fig. 38.1), as the active principle. The possibility that the extract of neem acts by causing a redox perturbation by imposing substantial oxidant stress during malarial infection has been postulated. The antiplasmodial and larvicidal activity of neem has been confirmed by others (Dhar et al., 1998; Isah et al., 2003; Nathan et al., 2005; Udeinya et al., 2006; Okumu et al., 2007; Soh and Benoit-Vical, 2007).
The published scientific proof for the efficacy of other African plants was reviewed by Sofowora (1993) while the efficacy of others can be readily deduced from their active constituents. For example, the use of Rauwolfia vomitoria roots (containing reserpine) in treating some mentally ill patients; Plumbago zeylanica root (containing the naphthoquinone, plumbagin) for treating various fungal skin diseases; Ocimum gratissimum leaves (containing essential oils rich in thymol) for treating diarrhoea are all clearly justifiable (Sofowora, 2008). Other plants whose active constituents have not been characterized have also been demonstrated experimentally in the laboratory to be efficacious. Examples of these include remedies used in treating skin diseases and the use of Combretum mucronatum and Mitragyna stipulosa as anthelminthics (Sofowora, 2008).
Theories on the origin of herbal medicine in Africa
It has been proposed that the knowledge of medicinal plants in Africa was gained by accident, although this theory has been refuted by a number of African TMPs, who claim that information on such plants was communicated to their ancestors in various ways. However, early Africans could have gained some specific knowledge by watching the effects produced by various plants when eaten by domestic animals. Even today, some herbalists try out remedies, in the presence of their patients, on domestic animals, especially when testing for toxicity, and on themselves or their relations. Such tests prove to the patient that the preparation is harmless and sometimes also confirm that the dosage prescribed is also justifiable. Such information on African medicinal and toxic plants has been passed on orally from generation to generation and even today there are many herbal cures in Africa that have not been written down (Sofowora, 2008).
Hunters, especially in African countries, have been reported as the original custodians of some effective traditional herbal recipes. Such knowledge could have been acquired when, for example, a hunter shot an elephant. If the elephant ran away, chewed leaves from a specific plant and did not die, it is believed the hunter noted the plant as a possible antidote for wounds or for relieving pain. Similar observations were made in villages where, for example, a domestic animal chewed the leaf of a specific plant when that animal was ill and recovered later or when another animal accidentally chewed a leaf and died (Sofowora, 2008). Similar observations by scientists have confirmed that chimpanzees use medicinal plants in Africa for self-medication (Huffman and Wrangham, 1993).
RESEARCH INTO AFRICAN MEDICINAL PLANTS
Information on the use of medicinal plants has been obtained from herbalists, herb sellers and indigenous people in Africa over many years (Baba et al., 1992). Under the umbrella of Agence de Coopération Culturelle et Technique (ACCT) in Paris, ethnobotanical surveys with international teams had been carried out by 1988 in the following African countries: Central African Republic, Rwanda, Mali, Niger, Federal Islamic Republic of Comoros, Mauritius, Seychelles, Gabon, Dominica, Tunisia, Madagascar, Togo, Congo and Benin Republic. The African Union’s Scientific Technical and Research Commission (AU/STRC) carried out similar surveys in Western Nigeria, Uganda, Cameroon, Ghana, Swaziland and Mozambique as at 2004 (Adjanohoun et al., 1989, 1993, 1996; Mshana et al., 2000; Adeniji et al., 2001, 2004). All these ethnobotanical surveys have been published. Other ethnobotanical surveys on the region have also been published (Samuelsson et al., 1991).
As early as 1968, it was decided at a conference organized in Dakar by the AU/STRC that the efficacy of herbs used by TMPs should be tested, particularly in the following areas: anticancer, antimalarial, antihelminthic, antimicrobial, antihypertensive, cardiac activity, antisickling and antiviral. The following is a summary of the research to date, as indicated by publications on African medicinal plants collated by NAPRALERT database for natural products. Only 36% of all publications dealt with bioassay-guided isolation of plant constituents along with their pharmacological and toxicological testing. The remainder dealt with purely phytochemical research (including quantitative analysis). Biological screening work resulted in publications on antimicrobial activity (16%), molluscicidal (11%), antimalarial (7%), toxicity testing (7%) and antitumour related (4%), while other minor biological testing amounted to 55% of the total publications relating to bioassay-guided research on African medicinal plants to 1993 (Sofowora, 1993, 2008). In molluscicidal testing, three plants came out as having potential commercial exploitation, namely Phytolacca dodecandra, Swartzia madagascariensis and Tetrapleura tetraptera. The field trials on these and toxicity studies against non-target organisms have been carried out successfully in ponds where the intermediate host snail of schistosomiasis is prevalent (Hostettmann, 1991).
Cryptolepis sanguinolenta, which is used for treating urinary infections in TM, has been shown to be strongly antimicrobial. Cryptolepine was identified as the active alkaloid. The extract of this root has been formulated for therapeutic use by the Centre for Research into Plant Medicine in Ghana. A new alkaloid, named cryptospirolepine (Fig. 38.1), was characterized from this root by Tackie et al. (1993) whereas hydroxycryptolepine, cryptoheptine and cryptoquindoline (three new alkaloids) were reported from a specimen of the same root collected in Guinea Bisau by Houghton et al. (1993). Paulo et al. (1993) have examined the alkaloids characterized by Houghton et al. (1993) from this root for antibiotic activity. All the alkaloids showed activity but to varying degrees against the test organisms used. According to Cimanga et al. (1996, 1997), this plant showed potent antibacterial, anticomplementary and moderate antiviral activities, but no antifungal effect. The results obtained by Paulo et al. (1994a, 1994b) after testing the root extracts and its alkaloids against diarrhoeal and other bacteria suggested that the roots could be a therapeutic alternative for bacterial etiologic diarrhoea in West Africa. See Sofowora (2008) for more research on Cryptolepis sanguinolenta.
Garcinia kola seeds are chewed for protection against liver disease and were shown to contain biflavonoids (Iwu, 1993; Tarashima et al., 2002). The biflavonoids and the crude extracts of the seed have been shown to be effective in protecting against liver damage (Farombi et al., 2004, 2005; Odunola et al., 2005; Adaramoye and Adeyemi, 2006a) and they ameliorate di-n-butylphthalate-induced testicular damage in rats (Farombi et al., 2007). The mechanisms involved in the hepatoprotection were explained by Farombi in 2000. ‘Kolaviron’ has been patented for commercial exploitation and the methods for its isolation and quantification have been enunciated. Other activities reported for ‘Kolaviron’ and the extract of Garcinia kola include: Attenuation of indomethacin- and HCl/ethanol-induced oxidative gastric mucosa damage in rats, and hypoglycaemic and hypolipidaemic effects (Adaramoye and Adeyemi, 2006b), whereas toxicological investigations include on erythrocytes (Esomonu et al., 2005), alteration of oestrous cycle in rats (Akpantah et al., 2005) as well as the brine shrimp lethality and mutagenicity tests (Sowemimo et al., 2007). The amino acid composition of the seeds has been reported by Adeyeye et al. (2007).
Thaumatococcus danielli produces a red fruit, the aril of the seed of which contains the polypeptide thaumatin. Thaumatin is almost 5000 times as sweet as sucrose on molar basis. It is a low-calorie, high-intensity sweetener suitable for sweetening pharmaceuticals for diabetics. The plant grows readily in the moist areas of Africa and the early researches on its development were carried out jointly by researchers in Ife (Nigeria) and Tate and Lyle Ltd in UK. It is used in soft drinks in Japan (Sofowora, 2008). Thaumatin I and Thaumatin II have been cloned and synthesized through recombinant DNA. The cloning experiments showed that the N- and C-terminal regions of both of the thaumatin molecules do not play any important role in eliciting the sweet taste of thaumatin (Masuda et al., 2004; Zemanek and Wassermann, 2005; Ide et al., 2007).
Cassia podocarpa, which is used as a laxative in TM, has been shown to contain anthraquinone derivatives similar to those found in official senna of the British Pharmacopoeia. The leaves and pods were also compared for their biological efficacy with official senna and shown to be just as effective on a weight basis. C. podocarpa was also shown to be less toxic than official senna. This leaf has been formulated into tablets and recommended as a substitute for official senna in Africa through the work of African researchers (Abo and Adeyemi, 2002; Akomolafe et al., 2004). Danafco (Ghana) Ltd. produces standardized tea bags of this leaf on a commercial scale. Similar work on C. italica has led to the development of laxatives based on this plant, now commercially available in Mali and other African countries.
Euphorbia hirta is used traditionally in treating diarrhoea and dysentery in African TM. Although it contains phorbol derivatives this plant has been shown to be effective in vitro and in vivo against Entamoeba, which causes amoebic dysentry. The plant has been formulated into mixtures and a preparation of the whole plant is also available commercially in Mali for use against amoebic dysentery (Keita, 1994; see also Sofowora, 2008).
Zanthoxylum zanthoxyloides (Lam.) Waterm. The ‘antisickling’ property of the root of Z. zanthoxyloides was discovered when it was observed that the aqueous extract preserved the red colour of blood in blood-agar plates during a screen for its antimicrobial activity. The extract was later shown to revert sickled HbAS, HbSS and crenated HbAA red blood cells to normal in vitro. The activity was also demonstrated in the root of other Zanthoxylum species, and Z. gilletti was found to be just as active as Z. zanthoxyloides. This, and previous observations, led to postulation of a membrane-based activity earlier reported for the extracts. Activity-directed fractionation of the aqueous extract located the ether fraction as the active fraction. GC-MS analysis of the ether fraction indicated the presence of phenolic and fatty acids. These acids are 2-hydroxymethylbenzoic acid, p-hydroxybenzoic acid, vanillic acid, m-hydroxybenzoic acid, 2-hydroxy-3-phenylpropionic acid, traces of stearic acid, linoleic and palmitic acids. Further analysis of the fraction confirmed the presence of these acids and identified additional ones: p-coumaric, caffeic and ferulic acids. Xanthoxylol [2-dimethylallyl-4-(3-hydroxypropyl)phenol] was also isolated from the root. p-Hydroxybenzoic acid, 2-hydroxymethylbenzoic acid, vanillic acid, 2,2-dimethyl-2H-1-benzopyran-6-butyric acid (DBA; which is a chemical modification of xanthoxylol) and two uncharacterized non-acidic isomers of butyric acid isolated from the root have all been shown to possess antisickling activity. DBA also causes a slight increase in the pO2 of the HbSS. Although the extract from the root (Z. zanthoxyloides) and DBA have been reported as generally non-toxic to (whole) animals and intracellular enzymes of the red blood cell, such as glucose-6-phosphate and 6-phosphogluconate dehydrogenases, the extract was observed to revert sickled cells to round rather than discoid shapes in some experiments. DBA, however, has been shown to increase the activity of Ca2+-activated Mg2+-dependent ATPase in both normal HbAA and sickle HbSS cell membranes, suggesting an antisickling activity based on Ca2+ mobilization in the HbSS red cell membrane for the root extractives. Other synthetic benzoic acid derivatives known to possess antisickling activities are p-methoxybenzoic acid, 3,4-dihydroxybenzoic acid, 3,4-dimethylbenzoic acid and p-fluorobenzoic acid. Relating the observed antisickling activity to physicochemical parameters of substituted benzoic acids showed that increased lipophilicity enhances sickle-cell reversal activity and that electron-donating substituents play an important role in antisickling activity. Although the attempted preliminary clinical trial on sickle cell anaemia (SCA) patients was plagued with a high default rate, the results obtained appear to indicate significant diminution of painful episodes in treated individuals (Adesanya and Sofowora, 1994). A product developed from the extract of ‘Fagara’ is being marketed under the name DREPANOSTAT® in Togo and Benin Republics. In Burkina Faso and surrounding countries the herbal product FACA® which is a mixture of ‘Fagara’ and Calotropis procera is marketed for SCA (Sofowora 2008). The use of a leaf extract of Terminalia catappa as having antisickling potential has been supported by recent research involving human blood samples (Mgbemene and Ohiri, 1999). Research on other plants used in the management of SCA have been discussed by Adesanya and Sofowora (2008).
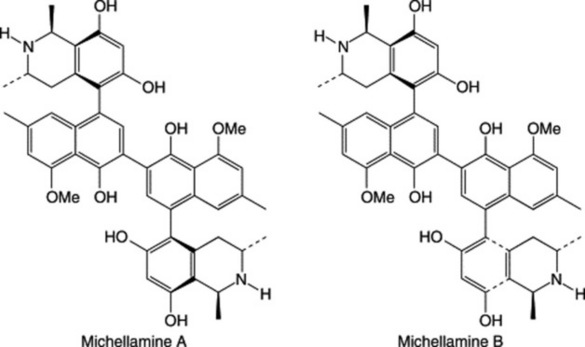
The development of bioassay techniques (Hostettmann, 1991) for antiviral activity in plants and the importance of finding a cure for HIV/AIDS has brought some African medicinal plants into prominence. About 120 plants have been reported to show antiviral activity (many of these grow in Africa, e.g. Diospyros, Spondias, Terminalia spp.), whereas others are reported to have immunomodulating properties, such as Aloe and Zingiber spp. etc. A new plant species, Ancistrocladus korupensis (Ancistrocladaceae), was discovered in Cameroon and found to contain new alkaloids: michellamines A and B, which have a wide spectrum of antiviral activity, including anti-HIV cytopathic activity. Efforts were made to develop michellamine B for use in HIV/AIDS treatment. It was characterized by collaborative effort of some Cameroon scientists and the National Cancer Institute in the USA. The plant is rare. Efforts are in progress to germinate the seeds in its natural habitat at Korup National Park, in glass houses and through tissue culture in collaboration with J. B. Johnson Biotech Laboratories (Manfredi et al., 1991; Jato et al., 1993). Readers should consult the review by Elujoba (2008) on plants used for the management of HIV/AIDS in Africa.
In a review of over 240 higher plants that are used in Africa as arrow poisons, Neuwinger (1996) cites many as having medicinal properties.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree