Immunotactoid Glomerulopathy
Anthony Chang, MD
Key Facts
Terminology
Congo red negative organized glomerular immunoglobulin deposits
Clinical Issues
Caucasian predilection
Nephrotic syndrome, hematuria, and hypocomplementemia
Often associated with monoclonal gammopathy or hematologic malignancy
Microscopic Pathology
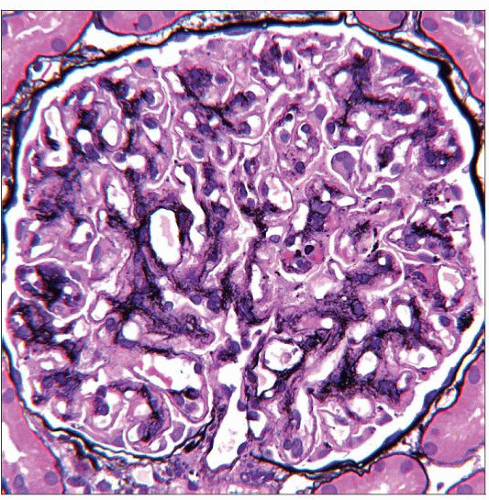
Mesangial expansion with eosinophilic, PAS-positive material
Mesangioproliferative or membranoproliferative pattern
Focal splitting and occasional “spikes” of basement membrane
Immunofluorescence with predominant IgG, with some cases showing IgA or IgM
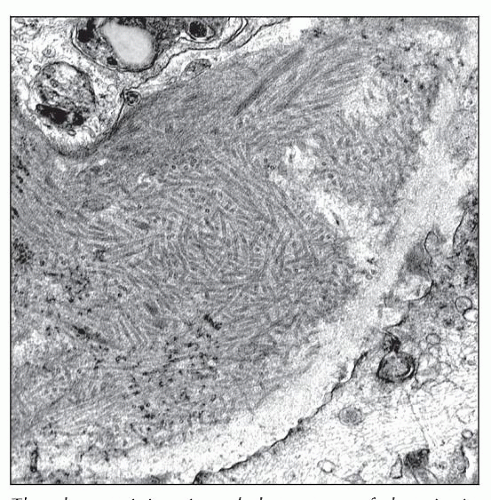
Electron microscopy shows microtubules organized in parallel arrays (> 30 nm) with hollow core
Top Differential Diagnoses
Cryoglobulinemic glomerulonephritis
Fibrillary glomerulopathy
Fibronectin glomerulopathy
Type III collagen glomerulopathy
Diagnostic Checklist
Congo red negative deposits with microtubular appearance and diameter typically > 30 nm
TERMINOLOGY
Abbreviations
Immunotactoid glomerulopathy (ITG)
Synonyms
Congo red negative organized glomerular immunoglobulin deposits
Definitions
Congo red negative microtubular deposits typically > 30 nm in diameter and arranged in parallel arrays
ETIOLOGY/PATHOGENESIS
Unknown Mechanism
Microtubular glomerular deposits usually represent monotypic immunoglobulins
CLINICAL ISSUES
Epidemiology
Incidence
Rare
< 0.1% of adult native kidney biopsies
Age
5th to 6th decade
Older than patients with fibrillary glomerulonephritis
Gender
Slight female predilection
Ethnicity
Caucasian predilection
Site
Typically limited to kidney
Presentation
Nephrotic syndrome
Hematuria
Hypocomplementemia
67% of patients have an associated monoclonal gammopathy or hematologic malignancy
Laboratory Tests
Serum or urine protein electrophoresis
Immunofixation or immunoelectrophoresis
Treatment
Drugs
Chemotherapy for underlying lymphoproliferative disorder or plasma cell dyscrasia, if present
Prognosis
Data limited: Median time to end-stage renal disease is ˜ 2 years
Clinical course depends on underlying lymphoproliferative disorder, if present
Occasional response to chemotherapy
Repeat biopsies show loss of deposits in a minority
Recurrence after kidney transplantation (˜ 50%), more benign course
MICROSCOPIC PATHOLOGY
Histologic Features
Glomerulus
Varied patterns: Mesangioproliferative, membranoproliferative, nodular glomerular disease
Mesangial expansion by eosinophilic, PAS-positive material
GBM: Focal splitting and occasional “spikes”
Rare crescents (vs. fibrillary glomerulonephritis)
Tubular atrophy
Interstitial fibrosis
Extrarenal deposits rarely reported (e.g., peripheral nerve)
ANCILLARY TESTS
Immunofluorescence
Predominantly IgG, with rare cases showing IgA or IgM
IgG1 is most common subclass when monotypic deposits present
Kappa &/or lambda light chain
Most cases are monoclonal, but polyclonal staining can be observed
C3 usually positive, and C1q less frequently positive
Electron Microscopy
Transmission
Microtubular deposits with hollow core or electron-lucent tubular lumen organized in parallel arrays
Typically > 30 nm in diameter (range: 20-90 nm)
Subendothelial location in irregular, chunky pattern along capillary loops and mesangium
Subepithelial and intramembranous deposits may also be seen
DIFFERENTIAL DIAGNOSIS
Cryoglobulinemic Glomerulonephritis
Electron-dense deposits often with substructural organization
Serum positive for cryoglobulins
Fibrillary Glomerulopathy
Randomly arranged fibrils with average thickness of 20 nm without hollow core
Polyclonal IF staining; commonly IgG4
Fibronectin Glomerulopathy
Fibrillar deposits < 30 nm; IgG negative
Positive immunohistochemistry for fibronectin
Type III Collagen Glomerulopathy
Periodic banded collagen fibrils by EM and type III collagen by IHC
Nail-Patella Syndrome
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree