Iliopubic Tract Repair of Inguinal and Femoral Hernia: the Posterior (Preperitoneal) Approach
Lloyd M. Nyhus
The posterior (preperitoneal, properitoneal, or extraperitoneal) approach to the repair of inguinal and femoral hernia had its origin with Annandale in 1876. Since then, interest in its use has waxed and waned, primarily because of a lack of understanding of the groin anatomy as seen posteriorly. The anatomic dissections of Condon first reported in 1960 presented with clarity the long-forgotten analogue of the transversalis fascia: the iliopubic tract. The intimate relation between the iliopubic tract and the abdominal wall defect was apparent, and the use of a strong band of fascia at the edge of each defect—the iliopubic tract—became the cornerstone of the repair. It soon became clear that the approach was mainly facilitative and that the iliopubic tract repair was the key to either an anterior or a posterior approach. In 1966, C. Thomas Bombeck and I presented both approaches and emphasized the iliopubic tract repair. The anterior approach and iliopubic tract repair are presented by Condon in Chapter 173.
General and detailed concepts of groin anatomy are presented throughout this section. Although greater exposition would be redundant, a few anatomic considerations that relate to the iliopubic tract repair must be reiterated.
Laminar Structure of the Inguinal Region
The abdominal wall is composed of musculoaponeurotic layers protected externally by skin and subcutaneous fat and covered internally by preperitoneal fat and peritoneum. An anatomic hernial repair should restore the continuity and integrity of each disrupted musculoaponeurotic lamina. In uncomplicated groin hernias, only the transversalis fascia lamina is disrupted; other structures are merely displaced. In the repair of groin hernias, the essential task is the repair and restoration of the transversalis fascial layer.
The inguinal region is separated into two laminar structures. The spermatic cord is contained between these layers within a cleft or space: the inguinal canal. The group of structures that lies anterior to the spermatic cord constitutes the anterior inguinal wall, or the superficial musculoaponeurotic lamina, and is composed of the Scarpa fascia and the external oblique aponeurosis and its lowermost fibers, the inguinal (Poupart) ligament. The spermatic cord exits from the medial end of the inguinal canal by passing through the anterior wall at the external inguinal ring. The structures posterior to the spermatic cord constitute the posterior inguinal wall, or the deep musculoaponeurotic lamina, and are composed of transversalis fascia and the transversalis fascial analogues: the iliopubic tract, crura and sling of the internal abdominal ring, the transversus abdominis aponeurosis, the anterior femoral sheath, and the Cooper ligament. The spermatic cord enters the lateral end of the inguinal canal by passing through the posterior inguinal wall at the internal abdominal ring. The floor of the inguinal canal is formed primarily by the bony superior ramus of the pubis and its closely associated structures: the pectineus muscle, the pectineus fascia, and the more distal portion of the anterior femoral sheath.
Transversalis Fascia
A groin hernia results anatomically from a weakening and relaxation of the transversalis fascia. This concept is fundamental to understanding the anatomy of all repairs of groin hernias. If surgical cure of the hernia is expected, the anatomic integrity of the transversalis fascia must be restored, no matter what technique of repair is used. If the defect in the transversalis fascia is not repaired, a high rate of recurrence follows. In the usual anterior approach to hernial repair, the exposure of the transversalis fascia is less than ideal, which may account in part for continuing relatively high recurrence rates with the anterior approach.
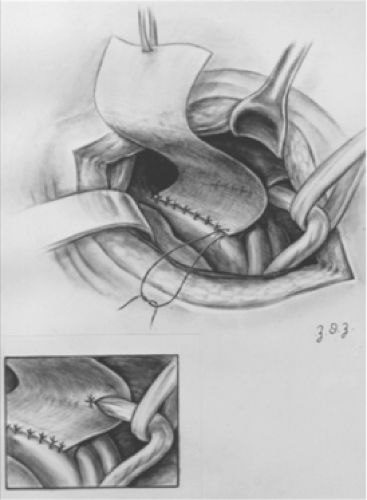
Adherence to the principle of restoration of the anatomic integrity of the transversalis fascia in groin herniorrhaphy does not imply an unalterable commitment to use only transversalis fascia in the repair. It does imply, however, that all the structures used for repair must lie within the transversalis lamina of the inguinal region—in the posterior inguinal wall. This layer still forms the essential guide to repair because it defines the lamina within which repair should be carried out. This statement applies to femoral hernias as well as to direct and indirect hernias. Often used in the hernioplasty are a group of ligamentous and aponeurotic structures closely associated with the transversalis fascia. These are capable of retaining heavy sutures and provide the strength required for the reapproximation and restoration of continuity of the transversalis fascia.
Iliopubic Tract
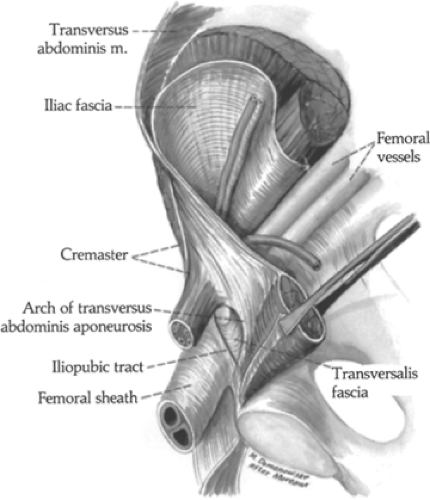
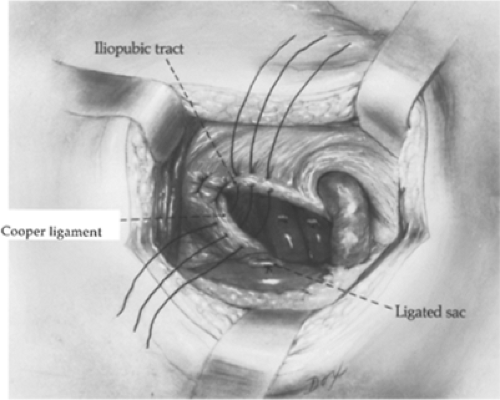
The iliopubic tract (ligamentum iliopubicum thomsonii, bandelette iliopubienne of the French) is a strong fascial band that begins laterally along the crest of the ilium and at the anterosuperior iliac spine. In this area, it gives origin to the iliacus muscle and the lowermost fibers of the transversus abdominis muscle. The iliopubic tract arches over the psoas muscle and femoral vessels, where it forms an integral part of the anterior femoral sheath (Fig. 1). In its midportion, it lies immediately subjacent to the inguinal ligament. It is, however, completely separated from the inguinal ligament, and the relation is one of proximity only. Continuing medially, the iliopubic tract inserts fan-wise into the superior ramus of the pubis and into the Cooper ligament (Fig. 2). The most inferior fibers of the iliopubic tract—those that insert most laterally into the Cooper ligament—are sharply recurved in the normal groin. It is this recurved portion of the iliopubic tract that defines the medial border of the femoral canal, rather than the lacunar (Gimbernat) ligament of classic description.
The fundamental importance of the iliopubic tract in understanding the anatomy of groin hernias is that it forms one of the margins of the hernial defect in each of the common groin hernias. Direct and indirect inguinal hernial defects are limited on their posterior aspects by the fibers of the iliopubic tract; femoral hernial defects are similarly limited on their medial and anterior aspects in the transversalis lamina of the inguinal region.
Transversalis Crura and Sling of the Internal (Abdominal) Inguinal Ring
The internal ring is given an elliptic shape by the presence on its anterior and posterior aspects of a double fold of transversalis fascia that cradles and supports the spermatic cord in this region. This sling, however, appears to be open laterally. As is implied by the name internal inguinal ring, transversalis fascia can be delineated on all sides of the defect. The posterior crus, or arm, of this sling consists of fibers that parallel the iliopubic tract and finally fuse with it. The anterior crus is a more dense band that has an extensive origin in the transversalis fascia above the internal ring. The two crura are, of course, continuous with each other on the medial aspect of the internal ring and spermatic cord; because they are more prominent at this level, a sling effect is given, which gives rise to the term transversalis fascial sling of the internal inguinal ring. Lateral movement of this sling when straining closes the fascial ring around the spermatic cord. This natural protective mechanism (sphincter) should be enhanced during hernioplasty by placement of sutures only into the posterior lamina, avoiding cross-laminar sutures between the anterior crus and the inguinal ligament.
Layers in the Hesselbach Triangle
Two layers of fascia cover the Hesselbach triangle: the transversalis fascia and fibers of the transversus abdominis aponeurosis. The adherence of these tissues to one another is also apparent at and above the heavy curved arch of the transversus abdominis aponeurosis. Thus, these structures are not isolated but are sutured as one layer in the repair.
The relevant structures contained within the posterior inguinal wall are illustrated in Figure 3.
A Classification of Groin Hernia
The classification of groin hernia (Table 1) includes primary inguinal and femoral hernias (types I, II, and III) as well as recurrent groin hernias (type IV). Primary inguinal hernias are classified according to the severity of the damage to the underlying internal abdominal ring or the defect in the Hesselbach triangle. Small to massive (e.g., scrotal or sliding) indirect hernias can be viewed as a continuum of disease. Initially, they are confined to the internal abdominal ring (type I); then they enlarge medially (type II). In the final stages, they alter the posterior inguinal wall (type III). All direct hernias (small and large without involvement of the internal abdominal ring) are in the transversalis fascial layer and therefore are considered type III.
The classification of groin hernias is based on anatomic criteria. The challenge in devising a classification of this nature lies in formulating descriptions that are clear and specific. The recommended operative approaches to the various types of hernias are given in Table 2.
Type I
Type I hernias are indirect inguinal hernias (usually in infants, children, or young adults) in which the internal abdominal ring is of normal size, configuration, and structure. The boundaries are well delineated and the Hesselbach triangle is normal. There is an indirect hernial sac, which extends variably from just distal to the internal abdominal ring to the midinguinal canal.
Type II
Type II hernias are indirect inguinal hernias in patients in whom the internal ring is enlarged medially and distorted without impinging on the floor of the inguinal canal. The Hesselbach triangle (floor of canal) is normal as palpated through the opened peritoneal sac. The hernial sac is not scrotal but may occupy the entire inguinal canal.
Type III
Type III classifies defects in the posterior inguinal wall (floor) into three subtypes: direct, indirect, and femoral. In direct inguinal hernias (type IIIA), the protrusion does not herniate through the internal abdominal (inguinal) ring. The weakened transversalis fascia (posterior inguinal wall medial to the inferior epigastric vessels) bulges outward in front of the hernial mass. Again, all direct hernias, small or large, are type IIIA.
Type IIIB hernias are indirect inguinal hernias with a large, dilated ring that has expanded medially and encroaches on the posterior inguinal wall (floor) to a greater or lesser degree. Type IIIB hernias frequently have a scrotal position. Occasionally, the cecum on the right or the sigmoid colon on the left makes up a portion of the sac wall. These sliding hernias always destroy a portion of the inguinal floor (types IIIA and IIIB).
The internal abdominal ring may be dilated without displacement of the inferior epigastric vessels. Direct and indirect components of the hernial sac may straddle those vessels to form a pantaloon hernia (types IIIA and IIIB). Type IIIC are femoral hernias, a specialized form of posterior wall defect.
Type IV
Type IV hernias are recurrent hernias. They cause intricate management problems and carry a higher morbidity than other hernias.
The posterior approach is ideal for circumventing the scar tissue in operations for recurrent hernias. In addition, the posterior inguinal wall is usually not touched during previous operations, making iliopubic tract repair feasible in every instance. An inlay polypropylene mesh buttress over the posterior repair has become routine in this approach to all recurrent hernias.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree