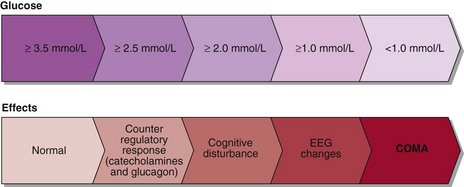
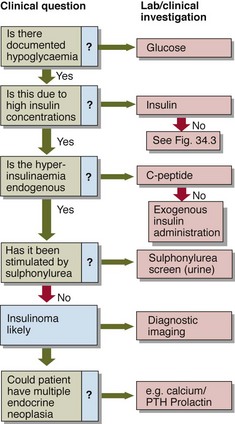
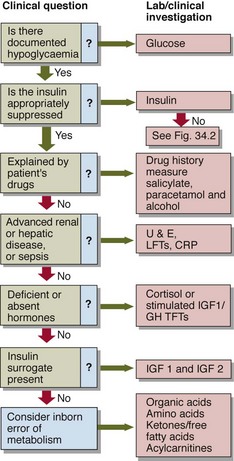
34 Hypoglycaemia normally leads to suppression of insulin secretion, an increase in catecholamine secretion and stimulation of glucagon, cortisol and growth hormone. The catecholamine surge accounts for the signs and symptoms most commonly seen in hypoglycaemia, i.e. sweating, shaking, tachycardia as well as feeling weak, jittery and nauseated. Hypoglycaemia decreases the glucose fuel supply to the brain and symptoms of cognitive impairment must always be sought since they reflect neuroglycopenia. They include confusion, poor concentration, detachment and, in more severe instances, convulsions and coma. The clinical effects of hypoglycaemia are summarized in Figure 34.1. The diagnosis of hypoglycaemia is established when three criteria (‘Whipple’s triad’) are satisfied. As a preliminary step to formal assessment, patients may be supplied with blood spot strips and asked to take fingerprick blood samples during symptomatic episodes. It may be necessary to try to precipitate symptoms, e.g. by prolonged fasting. If a blood sample is being collected for glucose analysis during a symptomatic episode, an additional sample should be collected simultaneously for insulin. This need not be analysed at the time, or indeed at all unless hypoglycaemia is confirmed, but the insulin level critically alters the differential diagnosis of hypoglycaemia (Figs 34.2 and 34.3).
Hypoglycaemia
Clinical effects
Assessment
 There must be symptoms consistent with hypoglycaemia.
There must be symptoms consistent with hypoglycaemia.
 There must be laboratory confirmation of hypoglycaemia.
There must be laboratory confirmation of hypoglycaemia.
Hypoglycaemia