Hypertensive Renovascular Disease
A. Brad Farris, III, MD
Key Facts
Terminology
Vascular and glomerular disease 2° to hypertension
Clinical Issues
˜ 30% of American adults have hypertension
95% due to “essential hypertension”
Causes ˜ 25% of ESRD
Effective drug therapy ameliorates renal sequelae
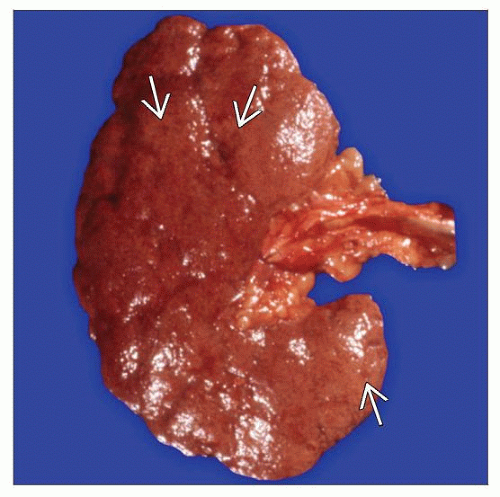
Macroscopic Features
Finely granular cortical surface
Petechiae in malignant hypertension
Microscopic Pathology
Subcapsular sclerotic scars with sclerotic glomeruli, thickened arterioles, and atrophic tubules
Global or segmental glomerulosclerosis
Arterial intimal fibrosis and arteriolar hyalinosis
“Onion skinning,” endothelial swelling, and fibrinoid necrosis of arterioles in accelerated hypertension
IF may show glomerular and arteriolar IgM, C3, fibrin
EM: Wrinkled GBMs, and in malignant hypertension, may show subendothelial expansion & fibrinoid necrosis
Top Differential Diagnoses
Diabetic nephropathy
Renal atheroembolization or severe atherosclerosis from hyperlipidemia
Primary FSGS
Renal artery stenosis leading to renal atrophy
Thrombotic microangiopathy, any cause
Systemic sclerosis
TERMINOLOGY
Abbreviations
Hypertension (HTN)
Arterionephrosclerosis (ANS)
Synonyms
Arterio-/arteriolonephrosclerosis
Hypertensive nephrosclerosis
Benign nephrosclerosis
Malignant nephrosclerosis
Definitions
Renal vascular and glomerular disease secondary to hypertension (blood pressure > 120/80 mmHg)
Accelerated hypertension, mean blood pressure > 140 mmHg, papilledema, retinal hemorrhage
ETIOLOGY/PATHOGENESIS
Essential Hypertension
95% of cases
Evidence for multigenic basis plus environmental factors
Risk factors include obesity, lack of exercise, salt intake, black race
Other factors: Low birth weight, decreased nephron number, dysmetabolic syndrome
Secondary Causes of Hypertension
5% of cases
Renal artery stenosis
Atherosclerosis, dysplasia, vasculitis, dissection
Increased production of renin by ischemic kidney
Neoplasia
Pheochromocytoma
Adrenal cortical tumors
Renin-producing tumors
Chronic renal disease
Cocaine abuse
Hypercoagulable states
Malignant Hypertension
May be primary or secondary
Renin release causes a cycle of vascular injury followed by more renin release
Features of thrombotic microangiopathy
Effect of Hypertension on Arteries and Arterioles
Hypertension precedes renal vascular disease
Shown in early renal biopsy series of Castleman and Smithwick
The more severe the renal vascular disease, the more reduced the glomerular filtration rate and renal blood flow
Vascular disease is the result, rather than cause, of hypertension
Involves direct injury to endothelium
Plasma (and fibrin) insudates into vascular walls
Arterial stiffening and increased pulse pressure to afferent arteriolar level leading to hyalinosis
Severe hypertension causes renal vascular fibrinoid necrosis (Goldblatt)
CLINICAL ISSUES
Epidemiology
Incidence
Approximately 30% of adult Americans have hypertension
Hypertension accounts for around 25% of end-stage renal disease (ESRD) cases
Malignant nephrosclerosis as result of malignant hypertension occurs at rate of 1-2 cases/100,000 per year
Age
Hypertension appears mostly between mid 40s and mid 50s
Renal damage and dysfunction take years to develop and manifest
Gender
Males have predisposition
Ethnicity
Disproportionately affects black race
Presentation
Hypertension
Proteinuria, asymptomatic
Related to severity of hypertension
Renal dysfunction
Accelerated (malignant) hypertension if mean blood pressure > 160 mmHg
Papilledema
Retinal hemorrhage
Congestive heart failure
Stroke
Encephalopathy
Renal insufficiency
Microangiopathic hemolytic anemia (MAHA)
Treatment
Drugs
Antihypertensive agents
Diuretics, mineralocorticoid receptor antagonists
ACE inhibitors, vasopeptidase inhibitors, renin inhibitors
Smooth muscle dilators, endothelin antagonists
β-adrenergic blockers, α-adrenoceptor blockers
Optimal blood pressure control reduces progression to renal insufficiency and may reverse hypertensive nephrosclerosis
Prognosis
ESRD develops in mean of 6 years from onset of azotemia
Factors that predispose to renal failure include
Increasing age
Poor serum glucose control in diabetic patients
Level of systolic blood pressure
Male gender
Black race
Elevated uric acid and triglycerides
High diastolic blood pressure
Malignant hypertension
If left untreated, survival is poor (20% 1-year survival)
Long-term survival is > 90% if blood pressure is controlled
MACROSCOPIC FEATURES
General Features
May be normal in size or slightly reduced in size and weight
Capsular surface is usually finely granular
Cortical scars may be present
Simple cysts may be present
Cortex may be thinned
Malignant hypertension
May be normal or increased in weight to 400 g
Petechial hemorrhages secondary to arteriolar necrosis gives “flea-bitten” appearance
May be mottled yellow and red if infarcts arise
MICROSCOPIC PATHOLOGY
Histologic Features
Subcapsular scars
Composed of sclerotic glomeruli, thickened arterioles, and atrophic tubules
Result in granular surface of kidney
Bulging areas between depressed scars contain spared and hypertrophied nephrons
Medium-sized arteries
Intimal fibrosis
Internal elastic lamina becomes multilayered (fibroelastosis); best seen on elastic stains
Smooth muscle hyperplasia
Decreased vascular lumen
Arterioles
Hyaline arteriolosclerosis
Afferent arteriolar media is replaced by homogeneous eosinophilic material positive on PAS or Masson trichrome stains
Begins under endothelial layer and eventually replaces entire media
Glomeruli
May have swollen endothelial cells and may thus appear “bloodless” and consolidated
Glomerular basement membranes may be duplicated
Glomerular mesangial matrix may be increased
Global glomerulosclerosis
Solidified type: Global solidification without collagenous material in Bowman space
Obsolescent type: Glomerular tuft sclerosed and Bowman space filled with collagenous material
Segmental glomerulosclerosis
Secondary focal segmental glomerulosclerosis (FSGS) may occur, typically with GBM corrugation and periglomerular fibrosis and subtotal foot process effacement
Glomerular hypertrophy (compensatory) in spared areas
Interstitium and tubules
Interstitial fibrosis and mononuclear inflammation
Tubular atrophy
Tubular hypertrophy in spared areas
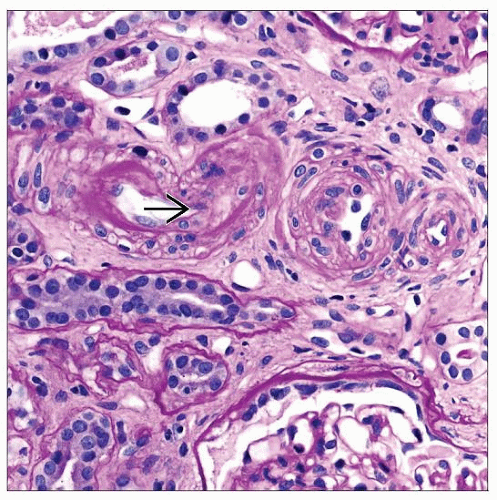
Histologic features of malignant hypertension
Small arteries
Mucoid (myxoid) intimal change and endothelial swelling in arterioles, a.k.a. “onion skinning”
Fibrinoid necrosis
Karyorrhectic debris
Occasional neutrophils within endothelium
Fibrin thrombi
Arterioles
Arteriolar occlusion by endothelial swelling/edema-type change
Fibrinoid necrosis
Fibrin thrombi
Glomeruli
Segmental necrosis of glomeruli
Ischemic retraction of glomeruli with corrugation of GBM
Treated hypertension
As shown by Pickering and Heptinstall
Acute lesions of fibrinoid necrosis and mucoid intimal thickening resolve with adequate treatment
Intima becomes fibrous with increased cellularity and elastic fibers
Predominant Cell/Compartment Type
Arterial intima
ANCILLARY TESTS
Immunofluorescence
IgM and C3 may be present in hyaline layers of arterioles
C3 may be present in absence of immunoglobulins
Fibrinogen is most common reactant seen on IF in malignant hypertension (in areas of fibrinoid necrosis and glomerular capillary loops)
Electron Microscopy
Transmission
Glomerular capillary basement membranes may be thickened or wrinkled
No electron-dense deposits
Thickening and duplication of arteriolar basement membranes
Arteriolar hyalinosis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree