Hypertension is the most important risk factor for stroke and congestive heart failure (CHF), and an important contributor to the risk of myocardial infarction.
The cardiovascular risk imposed by high blood pressure is reversed toward normal by effective treatment, with the most improvement in risk of stroke, and less, but significant risk reduction for myocardial infarction.
 The majority of cases of “essential” hypertension occur in association with obesity.
The majority of cases of “essential” hypertension occur in association with obesity.
Up to 70% of essential hypertension may be attributed to obesity. Obesity-related hypertension is salt sensitive and is associated with insulin resistance and hyperinsulinemia, sympathetic stimulation secondary to elevated levels of insulin and leptin, and activation of the renin-angiotensin-aldosterone system (RAAS). The RAAS activation is at least in part due to synthesis of RAAS components in visceral adipose tissue and release of these components into the circulation.
The Pressure–Natriuresis Relationship
Blood pressure and sodium excretion are inextricably related. Indeed, the pathophysiology of hypertension can only be understood in relation to sodium excretion. As the blood pressure increases, all other things being equal, sodium excretion increases: this is known as the “pressure–natriuresis relationship,” described in detail by physiologist Arthur Guyton and his colleagues over five decades ago. Since the kidney has an infinite capacity to compensate for BP elevations by increasing salt and water excretion, it follows that the kidney plays a critical role in the initiation and maintenance of hypertension.
Strong experimental evidence in support of the role of the kidneys in the pathogenesis and maintenance of hypertension includes the fact that norepinephrine (NE), infused intravenously, induces only transient increase in BP; natriuresis ensues with normalization of the BP. Sustained hypertension, on the other hand, results if the same dose of NE is infused into the renal artery, increasing sodium reabsorption and blunting natriuresis.
 The presence of high blood pressure is always associated with an alteration in the capacity of the kidney to excrete salt, imposing a so-called “natriuretic handicap.”
The presence of high blood pressure is always associated with an alteration in the capacity of the kidney to excrete salt, imposing a so-called “natriuretic handicap.”
In the hypertensive state the pressure–natriuresis relationship is shifted to the right: a given amount of sodium excretion is associated with a higher blood pressure (Fig. 5-1).
 The “natriuretic handicap” of the hypertensive state explains why all diuretics, regardless of class, are effective antihypertensive agents: they help the kidneys excrete salt, thereby restoring the pressure–natriuresis relationship toward normal.
The “natriuretic handicap” of the hypertensive state explains why all diuretics, regardless of class, are effective antihypertensive agents: they help the kidneys excrete salt, thereby restoring the pressure–natriuresis relationship toward normal.
There is a natural tendency to confuse the natriuretic handicap with salt and water retention, edema and volume expansion; this is not the case. The elevation in blood pressure is a compensatory mechanism that overcomes the altered sodium excretion in order to prevent volume expansion.
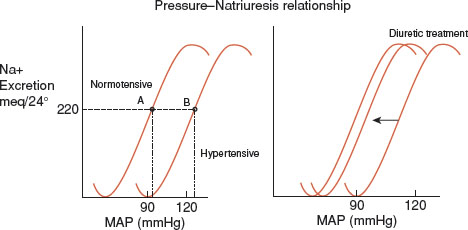
FIGURE 5.1 The pressure–natriuresis relationship: sodium excretion in relation to blood pressure. In balance on a normal sodium intake (say 220 mEq as shown in the figure) the normotensive individual will excrete the day’s intake at a mean arterial pressure (MAP) of 90 mm Hg (point A); the hypertensive individual will be able to maintain sodium balance only at a MAP of over 120 mm Hg (point B). This impediment to sodium excretion has been called the “natriuretic handicap” of hypertension. Diuretic treatment helps the kidney excrete salt, thereby moving the pressure natriuresis curve toward normal and addressing the natriuretic handicap.
 Despite the natriuretic handicap of hypertension edema and volume expansion are not present because the elevated BP compensates for the renal sodium avidity and permits the maintenance of sodium balance and a normal plasma volume.
Despite the natriuretic handicap of hypertension edema and volume expansion are not present because the elevated BP compensates for the renal sodium avidity and permits the maintenance of sodium balance and a normal plasma volume.
The natriuretic handicap of hypertension is best understood in a physiologic context. Precise regulation of blood pressure around a “normal” value is not a high priority. Maintenance of an adequate circulation, critical organ perfusion, and normal plasma volume are high priorities. Unlike serum sodium, or pH, or tonicity, BP varies considerably throughout the day under normal circumstances. BP increases with exercise and falls during sleep, for example. High blood pressure is a long-term, but not a short-term risk, while plasma volume regulation requires precise short-term regulation. A small mismatch in sodium intake and excretion may be fatal, resulting either in shock or pulmonary edema.
High blood pressure, therefore, represents the triumph of volume over pressure in physiologic regulation of the circulation, an example of the “wisdom of the body” to use the phrase coined by Walter Cannon. High blood pressure enables the individual to excrete the day’s sodium intake and maintain sodium balance despite an increased renal avidity for sodium.
 Hypertension is the footprint of mechanisms evolved to survive trauma, hemorrhage, and extracellular volume depletion.
Hypertension is the footprint of mechanisms evolved to survive trauma, hemorrhage, and extracellular volume depletion.
Essential hypertension may be seen in evolutionary terms as a consequence of mechanisms evolved to maintain an adequate circulation in the face of trauma with blood loss, or in other situations associated with extracellular fluid volume depletion. Such mechanisms include the RAAS and the sympathetic nervous system (SNS), both of which play a role in the maintenance of blood pressure under situations of blood loss or volume depletion as well as in the initiation and maintenance of hypertension. When activated these systems result in vasoconstriction and renal sodium reabsorption. Those individuals on the higher end of the spectrum of activity in these systems would have increased survival in the face of circulatory challenge, a clear short-term survival advantage, but would be predisposed to hypertension and its consequences in the long term.
 Most cases of “resistant” hypertension are due to insufficient diuretic inclusion in the regimen.
Most cases of “resistant” hypertension are due to insufficient diuretic inclusion in the regimen.
MALIGNANT HYPERTENSION
In times past much was made of the distinction between “benign” and “malignant” hypertension. The development of highly effective antihypertensive drugs, along with the recognition that “benign” is an inappropriate descriptor for hypertension, has almost, but not completely, rendered these terms of historical interest. It remains of clinical importance to recognize and treat malignant hypertension aggressively.
 Malignant hypertension is a medical emergency that requires prompt evaluation and treatment.
Malignant hypertension is a medical emergency that requires prompt evaluation and treatment.
Unrecognized and untreated treated malignant hypertension is usually lethal within a year.
 The pathologic hallmark of malignant hypertension is fibrinoid arteriolar necrosis. Clinical evidence of the latter may be found in the eye grounds and in the urine.
The pathologic hallmark of malignant hypertension is fibrinoid arteriolar necrosis. Clinical evidence of the latter may be found in the eye grounds and in the urine.
On funduscopic examination, flame-shaped hemorrhages and “cotton-wool” spots (fluffy exudates), which signify retinal infarction, are diagnostic of malignant hypertension. Papilledema, due to ischemia of the nerve head or increased intracranial pressure, often in association with hypertensive encephalopathy, are also indicative of malignant hypertension. Damage to the kidney is assessed by the urine analysis: heavy proteinuria and hematuria are consistent with malignant hypertension.
 Malignant hypertension is much more common in current smokers.
Malignant hypertension is much more common in current smokers.
Prompt lowering of the BP is essential to limit and reverse end organ damage.
 Malignant hypertension requires the consideration and the exclusion of secondary causes, particularly renal artery stenosis (RAS) and pheochromocytoma.
Malignant hypertension requires the consideration and the exclusion of secondary causes, particularly renal artery stenosis (RAS) and pheochromocytoma.
SECONDARY HYPERTENSION
 Secondary causes should be ruled out when the hypertension is severe, when it occurs in the young, or when the onset is abrupt.
Secondary causes should be ruled out when the hypertension is severe, when it occurs in the young, or when the onset is abrupt.
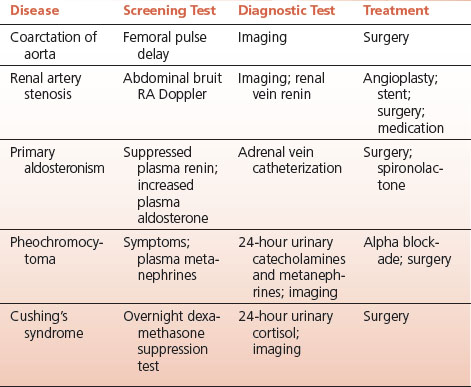
Particular attention should be directed to the correctible secondary causes including coarctation of the aorta, RAS, primary hyperaldosteronism, pheochromocytoma, and rarely, Cushing’s syndrome (Table 5-1).
 Coarctation of the aorta, has a strong male predominance, is diagnosed by a delay in the femoral pulse, is frequently associated with a bicuspid aortic valve, and when noted in a female, Turner’s syndrome is likely.
Coarctation of the aorta, has a strong male predominance, is diagnosed by a delay in the femoral pulse, is frequently associated with a bicuspid aortic valve, and when noted in a female, Turner’s syndrome is likely.
 It is a faux pearl that hyperthyroidism and the carcinoid syndrome are causes of secondary hypertension.
It is a faux pearl that hyperthyroidism and the carcinoid syndrome are causes of secondary hypertension.
Hyperthyroidism is associated with an increase in cardiac output and a wide pulse pressure; the diastolic BP is decreased. The carcinoid syndrome is associated with kinin-mediated hypotension rather than serotonin-mediated hypertension.
Renal Artery Stenosis
 The hypertension of RAS is usually severe and may be accentuated or brought on by oral contraceptives.
The hypertension of RAS is usually severe and may be accentuated or brought on by oral contraceptives.
TABLE 5.1 Correctable Secondary Hypertension
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


