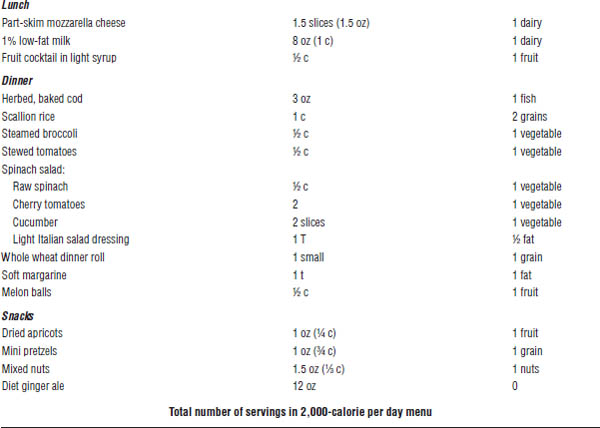
Figure 12-1. Sympathetic Nervous System Activation
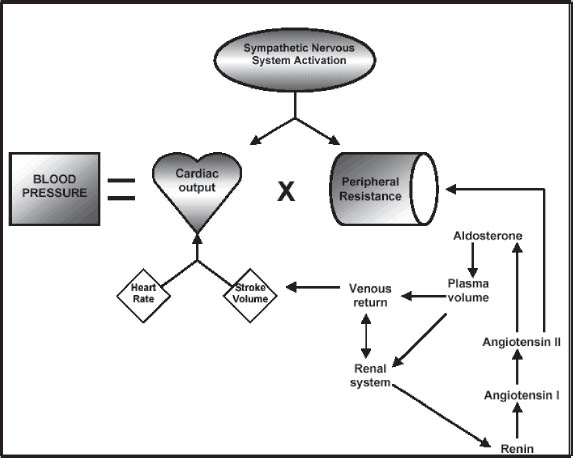
Adapted from Carter BL, Saseen JL, 2002.
■ Angiotensin-converting enzyme (ACE) causes AT-I to become angiotensin II (AT-II).
■ AT-II is a potent vasoconstrictor and stimulates aldosterone release, which increases sodium and fluid retention.
Water and sodium retention
■ Acute: Increased fluid volume causes increased cardiac output, which causes increased blood pressure (BP).
■ Chronic: Excess intracellular sodium causes vascular hypertrophy, which increases vascular resistance and response to vasoconstriction and, in turn, increases BP.
Etiology
Primary (essential) hypertension
■ Unknown cause
■ Found in 85–95% of all hypertension cases
Secondary hypertension
■ Renovascular disease: This condition is suggested by increased blood urea nitrogen (BUN) and creatinine and by abdominal bruits.
■ Primary aldosteronism: This condition is suggested by unprovoked hypokalemia.
■ Cushing’s syndrome: This condition is suggested by unprovoked hypokalemia and truncal obesity with purple striae.
■ Pheochromocytoma: This condition is suggested by increased urinary catecholamine excretion (i.e., vanillylmandelic acid and metanephrine) accompanied by headache, palpitations, and perspiration.
■ Aortic coarctation: This condition is suggested by delayed or absent femoral pulses and decreased BP in the lower extremities.
■ Drug-induced hypertension: The following drugs may induce hypertension:
• Steroids and estrogens (including oral contraceptives)
• Alcohol
• Cocaine
• Cyclosporine and tacrolimus
• Sympathomimetics
• Erythropoietin
• Licorice (in chewing tobacco)
• Monoamine oxidase (MAO) inhibitors
• Tricyclic antidepressants
• Nonsteroidal anti-inflammatory drugs (NSAIDs)
Table 12-1. Recommendations for Follow-up Based on Initial BP Measurements for Adults
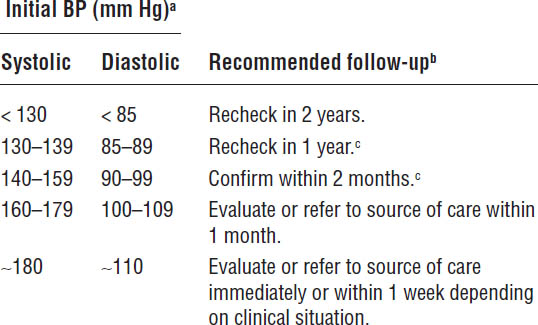
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
a. If systolic and diastolic readings are different, follow recommendations for shorter time to follow-up (e.g., a person with a reading of 160/86 mm Hg should be evaluated or referred to source of care within 1 month).
b. Modify the scheduling of follow-up according to reliable information about past BP measurements, other cardiovascular risk factors, or target organ disease.
c. Provide advice about lifestyle modifications.
Diagnostic Criteria
Diagnosis and treatment begin with proper BP measurement, assessment, and follow-up planning (Table 12-1). The patient should avoid ingesting caffeine and smoking for 30 minutes prior to BP measurement and should be resting for 5 minutes prior to BP measurement. BP is measured as follows:
■ Position arm (brachial artery) at heart level.
■ Uncover arm; do not put cuff over clothes.
■ Determine proper size cuff.
Upper arm circumference | Cuff size required |
|
|
16–22.5 cm | Pediatric cuff |
22.6–30 cm | Regular adult cuff |
30.1–37.5 cm | Large adult cuff |
37.6–43.7 cm | Thigh cuff |
■ Position cuff 1 inch above antecubital crease.
■ Ask patient about previous readings.
■ Place stethoscope over brachial artery (medial to the center).
■ Inflate cuff rapidly to approximately 30 mm Hg above previous readings.
■ Deflate cuff slowly.
■ Remember to deflate cuff completely when done.
■ Wait 1–2 minutes before repeating.
■ Take pressure in both arms.
■ If orthostatic hypotension is suspected, take BP while patient is sitting, standing, and supine.
■ If two readings are taken at least 2 minutes apart, average the readings.
■ If readings differ by > 5 mm Hg, take additional readings.
Treatment Principles and Goals
Figure 12-2 and Table 12-2 outline some important treatment principles. Goals include the following:
■ To reduce end-organ damage
■ To minimize or control other risk factors for cardiovascular (CV) disease
■ To maintain BP, with minimal side effects, at or below the level appropriate for the patient’s risk:
• 140/90 mm Hg for those individuals age < 60 years, with diabetes and with chronic kidney disease
• 150/90 mm Hg for those individuals age ≥ 60 years
Monitoring and Evaluation
Initial evaluation
The initial evaluation of a patient with hypertension has the following goals:
■ To identify known causes of high blood pressure
■ To assess the presence or absence of target organ damage and CV disease, the extent of disease, and the patient’s response to therapies (Box 12-1)
■ To identify other CV risk factors or concomitant disorders that may affect prognosis and guide therapy (Box 12-1)
The patient’s history should be considered in the initial evaluation:
■ Duration and levels of elevated BP
■ History or symptoms of coronary heart disease (CHD), heart failure, cerebrovascular disease, pulmonary vascular disease, diabetes mellitus, renal disease, or dyslipidemia
■ Family history of hypertension, premature CHD, stroke, diabetes, dyslipidemia, or renal disease
■ Symptoms suggesting the cause of hypertension
■ Recent weight changes, physical activity levels, or smoking or other tobacco use
■ Dietary assessment of intake of sodium, alcohol, saturated fat, and caffeine
■ Complete medication history, including prescription, over-the-counter, and herbal or natural products that may increase BP or decrease effectiveness of antihypertensive agents
Figure 12-2. Algorithm for the Treatment of Hypertension
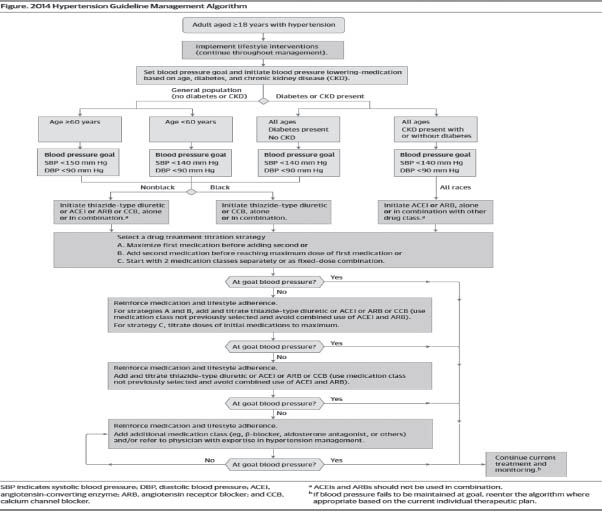
JNC-VIII, 2013.
■ Results and adverse effects of previous antihypertensive therapy
■ Psychosocial and environmental factors that may influence hypertension control
An examination should also be done:
■ Two or more blood pressure measurements separated by at least 2 minutes
■ Measurement of height, weight, and waist circumference
■ Funduscopic exam for hypertensive retinopathy
■ Exam of neck for carotid bruits, distended veins, or enlarged thyroid gland
■ Exam of heart for abnormalities in rate and rhythm, increased size, precordial heave, clicks, murmurs, and third and fourth heart sounds
■ Exam of lungs for rales and evidence of bronchospasm
■ Exam of abdomen for bruits, enlarged kidneys, masses, and abnormal aortic pulsation
■ Exam of extremities for decreased or absent peripheral arterial pulsations, bruits, and edema
■ Neurologic assessment
Routine laboratory tests are necessary:
■ Urinalysis
■ Complete blood cell count (CBC)
Table 12-2. Identifiable Causes, Diagnostic Tests, and Clinical Findings for Secondary Hypertension
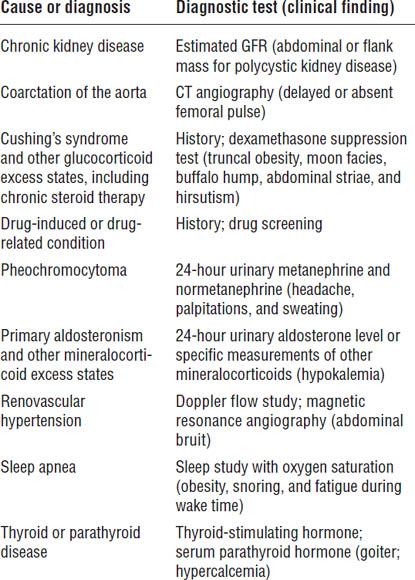
CT, computed tomography; GFR, glomerular filtration rate.
■ Blood chemistries (sodium, potassium, creatinine, BUN, and glucose)
■ Fasting lipid profile: total cholesterol, triglycerides, HDL (high-density lipoprotein), and LDL (low-density lipoprotein)
■ Electrocardiogram (ECG)
The following laboratory tests are optional:
■ Creatinine clearance
■ Microalbuminuria
■ 24-hour urinary protein
■ Blood calcium
■ Uric acid
■ Glycosylated hemoglobin
■ Thyroid-stimulating hormone
■ Limited echocardiography
■ Ankle-brachial index
■ Plasma renin activity and urinary sodium determination
Box 12-1. Cardiovascular Risk Factors
Major Risk Factors
■ Hypertensiona
■ Cigarette smoking
■ Obesitya (body mass index ≥ 30 kg/m2)
■ Physical inactivity
■ Dyslipidemiaa
■ Diabetes mellitusa
■ Microalbuminuria or estimated GFR < 60 mL/min
■ Age (> 55 for men, > 65 for women)
■ Family history of premature cardiovascular disease (men under age 55, women under age 65)
Target Organ Damage
Heart
■ Left ventricular hypertrophy
■ Angina or prior myocardial infarction
■ Prior coronary revascularization
■ Heart failure
Brain
■ Stroke or transient ischemic attack
Kidney
■ Chronic kidney disease
■ End stage renal disease
Vascular System
■ Peripheral arterial disease
Eyes
■ Retinopathy
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute. GFR, glomerular filtration rate.
a. Components of the metabolic syndrome.
Follow-up evaluation
Follow-up evaluation includes any of the previous exams completed during the initial evaluation that are required to monitor both response to and possible adverse effects from prescribed antihypertensive therapies, in addition to the assessment of any new symptoms of target organ damage and the assessment of patient adherence to therapy (Box 12-2).
12-4. Nondrug Therapy
Lifestyle modifications are recommended to improve both BP and overall cardiovascular health (Table 12-3).
Box 12-2. General Guidelines to Improve Patient Adherence to Antihypertensive Therapy
■ Be aware of signs of patient nonadherence to antihypertensive therapy.
■ Establish the goal of therapy: to reduce blood pressure to nonhypertensive levels with minimal or no adverse effects.
■ Educate patients about the disease, and involve them and their families in its treatment. Have them measure blood pressure at home.
■ Maintain contact with patients; consider telecommunication.
■ Keep care inexpensive and simple.
■ Encourage lifestyle modifications.
■ Integrate pill taking into routine activities of daily living.
■ Prescribe medications according to pharmacologic principles, favoring long-acting formulations.
■ Be willing to stop unsuccessful therapy and try a different approach.
■ Anticipate adverse effects. Adjust therapy to prevent, minimize, or ameliorate side effects.
■ Continue to add effective and tolerated drugs, stepwise, in sufficient doses to achieve the goal of therapy.
■ Encourage a positive attitude about achieving therapeutic goals.
■ Consider using nurse case management.
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
Research has shown that diets rich in fruits, vegetables, and low-fat dairy foods, and with reduced saturated and total fats, significantly lower blood pressure (Tables 12-4 and 12-5).
12-5. Drug Therapy
All patient factors (severity of BP elevation, presence of target organ damage, and presence of CV disease or other risk factors) must be considered when initiating therapy.
Initial Therapy
■ For candidates for therapy, see Figure 12-2.
■ Use of lifestyle modifications (Table 12-3) should continue to be stressed to patients after the decision to initiate drug therapy has been made to further decrease the risk of complications from cardiovascular disease.
■ JNC-VIII recommends the use of thiazide diuretics, as initial therapy in non–African American patients alone or in combination with other agents.
■ JNC-VIII recommends CCBs and thiazide diuretics in African American patients alone or in combination.
■ JNC-VIII recommends ACEIs or ARBs alone or in combination with other drug types in CHD regardless of race or diabetes status.
Table 12-3. Lifestyle Modifications to Manage Hypertension
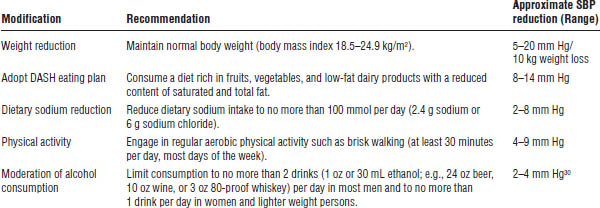
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
DASH, Dietary Approaches to Stop Hypertension. For overall cardiovascular risk reduction, stop smoking. The effects of implementing these modifications are dose and time dependent and could be greater for some individuals.
Table 12-4. Dietary Suggestions for Hypertensive Patients
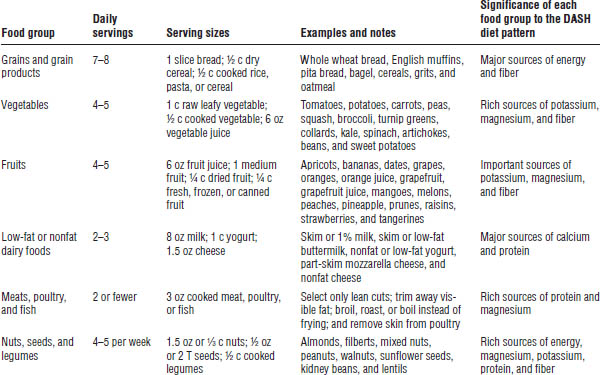
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
DASH, Dietary Approaches to Stop Hypertension.
Table 12-5. The DASH Diet Sample Menu Based on 2,000 Calories per Day
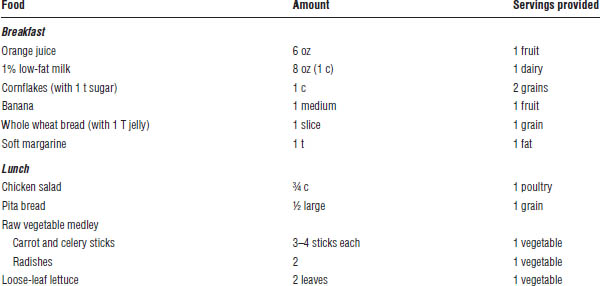
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
DASH, Dietary Approaches to Stop Hypertension.
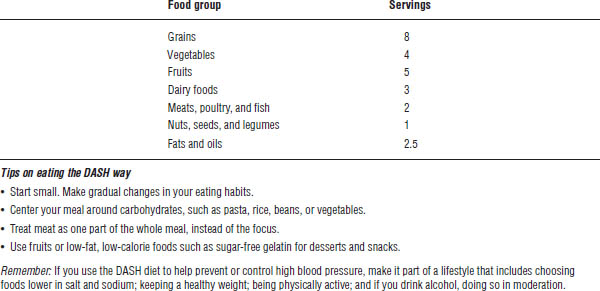
Table 12-6. Strategies to Dose Antihypertensive Drugs
■ JNC-VIII recommends three strategies to dose antihypertensive drugs (Table 12-6). For each strategy, begin with one drug, titrate to maximum dose, and then add a second drug from a second class.
■ For patients who are 20/10 mm Hg greater than their goal BP, 2-drug combination therapy should be strongly considered.
■ All causes for an inadequate response should be addressed before additional agents are added to a patient’s antihypertensive regimen (Box 12-3).
■ Vasodilators, α1-receptor antagonists, α2-receptor agonists, and postganglionic adrenergic neuron blockers should be avoided as initial agents for hypertension.
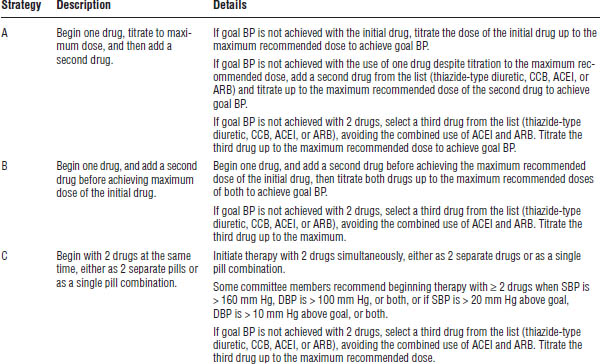
Diuretics
Thiazide and thiazide-like diuretics
See Table 12-7 for a list of thiazide and thiazide-like diuretics, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
■ Direct arteriole dilation occurs.
■ Reduction of total fluid volume occurs through the inhibition of sodium reabsorption in the distal tubules, which causes increased excretion of sodium, water, potassium, and hydrogen.
■ The effectiveness of other antihypertensive agents is increased by preventing reexpansion of plasma volume.
■ A significant decrease in efficacy occurs in renal failure: serum creatinine > 2 mg/dL or glomerular filtration rate (GFR) < 30 mL/min.
■ Diuretics are also available in combination with other drugs (Table 12-8).
Patient instructions and counseling
■ Medication may be taken with food or milk.
■ Take early in the day to avoid nocturia.
■ Medication may increase sensitivity to sunlight. Consider using sunscreen with SPF (sun protection factor) > 15.
■ Medication may increase blood glucose in diabetics.
Box 12-3. Causes of Inadequate Responsiveness to Therapy
Pseudoresistance
■ “White-coat hypertension” or office elevations
■ Pseudohypertension in older patients
■ Use of regular adult cuff on a very obese arm
Nonadherence to therapy
Volume overload
■ Excess salt intake
■ Progressive renal damage (nephrosclerosis)
■ Fluid retention from reduction of blood pressure
■ Inadequate diuretic therapy
Drug-related causes
■ Doses too low
■ Wrong type of diuretic
■ Inappropriate combinations
■ Rapid inactivation (e.g., hydralazine)
■ Drug actions and interactions
■ Sympathomimetics
■ Nasal decongestants
■ Appetite suppressants
■ Cocaine and other illicit drugs
■ Caffeine
■ Oral contraceptives
■ Adrenal steroids
■ Licorice (as may be found in chewing tobacco)
■ Cyclosporine or tacrolimus
■ Erythropoietin
■ Antidepressants
■ Nonsteroidal anti-inflammatory drugs
Associated conditions
■ Smoking
■ Increasing obesity
■ Sleep apnea
■ Insulin resistance or hyperinsulinemia
■ Ethanol intake of more than 1 oz (30 mL) per day
■ Anxiety-induced hyperventilation or panic attacks
■ Chronic pain
■ Intense vasoconstriction (arteritis)
■ Organic brain syndrome (e.g., memory deficit)
Identifiable causes of hypertension
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
■ Report problems with muscle cramps, which may indicate decreased potassium level.
Drug–drug and drug–disease interactions
■ Steroids cause salt retention and antagonize thiazide action.
■ NSAIDs blunt thiazide response.
■ Class IA or III antiarrhythmics (that prolong the QT interval) may cause torsades de pointes with diuretic-induced hypokalemia.
■ Probenecid and lithium block thiazide effects by interfering with thiazide excretion into the urine.
■ Thiazides decrease lithium renal clearance and increase the risk of lithium toxicity.
Parameters to monitor
■ BP
■ Weight
■ Serum electrolytes and uric acid
■ BUN and creatinine
■ Cholesterol levels
Loop diuretics
See Table 12-7 for a list of loop diuretics, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
■ Reduction of total fluid volume occurs through the inhibition of sodium and chloride reabsorption in the ascending loop of Henle, which causes increased excretion of water, sodium, chloride, magnesium, and calcium.
■ Loop diuretics are more effective than thiazides in patients with renal failure: serum creatinine > 2 mg/dL or GFR < 30 mL/min.
Patient instructions and counseling
■ Medication may be taken with food or milk.
■ Take early in the day to avoid nocturia.
■ Medication may increase sensitivity to sunlight. Consider using sunscreen with SPF > 15.
■ Medication may increase blood glucose in diabetics.
■ Report problems with muscle cramps, which may indicate decreased potassium level.
■ Rise slowly from a lying or sitting position.
Drug–drug and drug–disease interactions
■ Aminoglycosides can precipitate ototoxicity when combined with loop diuretics.
■ NSAIDs blunt diuretic response.
Table 12-7. Thiazide Diuretics, Thiazide-Like Diuretics, Loop Diuretics, Potassium-Sparing Agents, and Aldosterone-Receptor Blockers
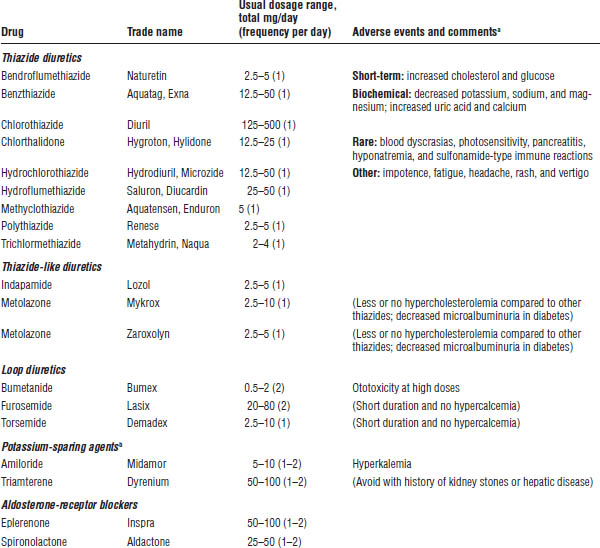
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
a. Adverse events, or side effects, listed are for the class of drugs, except where noted for individual drugs (in parentheses).
b. See Table 12-8 for combination products.
■ Class IA or III antiarrhythmics (that prolong the QT interval) may cause torsades de pointes with diuretic-induced hypokalemia.
■ Probenecid blocks loop diuretic effects by interfering with excretion into the urine.
Parameters to monitor
■ Weight
■ Serum electrolytes
■ BUN and creatinine
■ Uric acid
■ Hearing (in high doses)
Potassium-sparing diuretics
See Table 12-7 for a list of potassium-sparing diuretics, their usual dosage range, and adverse effects associated with these medications.
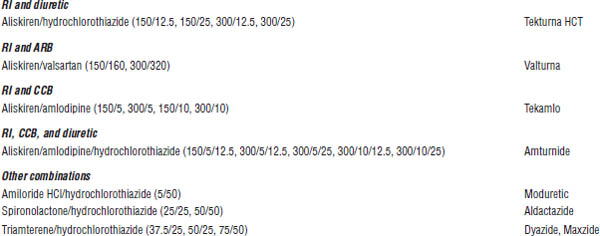
Table 12-8. Combination Drugs for Hypertension
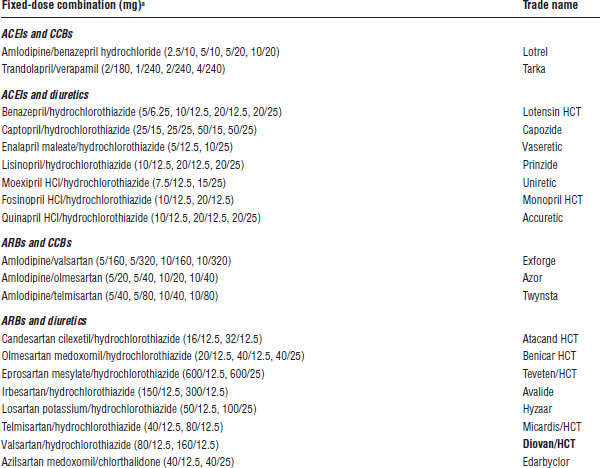
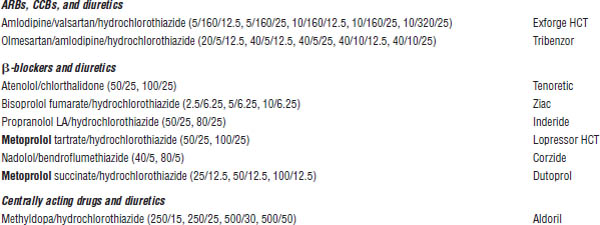
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
BB, β-blocker; RI, renin inhibitor.
a. Some drug combinations are available in multiple fixed doses. Each drug dose is reported in milligrams.
Mechanism of action
■ Potassium-sparring diuretics interfere with potassium and sodium exchange in the distal tubule, decrease calcium excretion, and increase magnesium loss.
Patient instructions and counseling
■ Take early in the day to avoid nocturia.
■ Take after meals.
■ Avoid excessive ingestion of foods high in potassium and use of salt substitutes.
■ Medication may increase blood glucose in diabetics.
■ Report problems with muscle cramps, which may indicate decreased potassium levels.
■ Sexual dysfunction is possible.
Drug–drug and drug–disease interactions
■ ACEIs may increase the risk of hyperkalemia.
■ Indomethacin can cause a decrease in renal function when combined with triamterene.
■ Cimetidine increases bioavailability and decreases clearance of triamterene.
Parameters to monitor
■ Weight
■ Serum electrolytes (especially potassium)
■ BUN and creatinine
Adrenergic Inhibitors
Postganglionic adrenergic neuron blockers
This medication class is best avoided unless necessary to treat refractory hypertension that is unresponsive to all other agents, because the medications are poorly tolerated. See Table 12-9 for a list of postganglionic adrenergic neuron blockers, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
Postganglionic adrenergic neuron blockers cause presynaptic inhibition of the release of the neurotransmitter from peripheral neurons by agonistic activity on the α2 receptor and depletion of the neurotransmitter through competitive uptake into the neurosecretory vesicles.
Patient instructions and counseling
■ Report symptoms of dizziness or hypotension.
■ Do not take over-the-counter (OTC) cold products without first asking the doctor or pharmacist.
■ Rise slowly from a lying or sitting position.
■ Report new fluid retention.
■ Sexual dysfunction is possible.
Table 12-9. Postganglionic Adrenergic Neuron Blockers
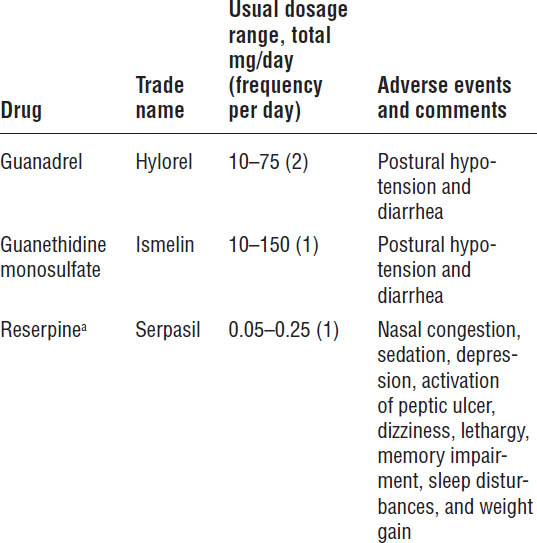
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
a. Reserpine also acts centrally.
Drug–drug and drug–disease interactions
■ OTC sympathomimetics may potentiate an acute hypertensive effect.
■ Tricyclic antidepressants and chlorpromazine antagonize the therapeutic effects of guanethidine.
■ Pheochromocytoma is a contraindication to this class of medications.
■ This medication class should be avoided in patients with CHF, angina, and cerebrovascular disease.
Parameters to monitor
■ History of depression (reserpine)
■ Sleep disturbances, drowsiness, and lethargy (reserpine)
■ Symptoms of peptic ulcer (reserpine)
Centrally active α2-agonists
See Table 12-10 for a list of centrally active α2-agonists, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
These medications cause decreased sympathetic outflow to the cardiovascular system by agonistic activity on central α2 receptors.
Table 12-10. Centrally Active α2-Agonists
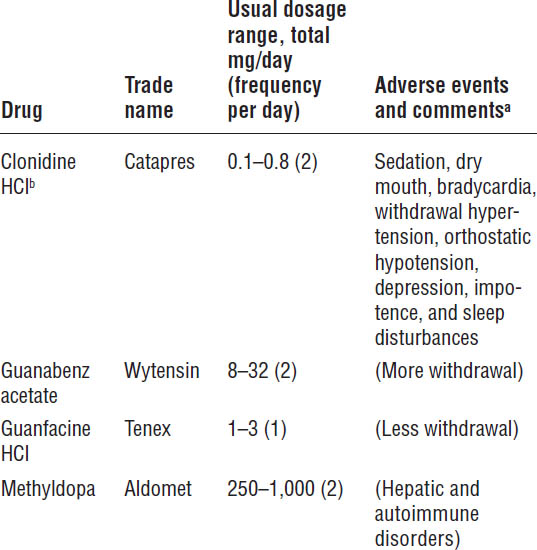
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
a. Adverse events, or side effects, listed are for the class of drugs, except where noted for individual drugs (in parentheses).
b. Clonidine HCl is also available as a once-weekly transdermal patch.
Patient instructions and counseling
■ Report symptoms of dizziness or hypotension.
■ Exercise sedation precautions.
■ Fever and flu-like symptoms may represent hepatic dysfunction (methyldopa).
■ Report new fluid retention.
■ Sexual dysfunction is possible.
Drug–drug and drug–disease interactions
■ Use cautiously with other sedating medications.
■ Use cautiously in patients with angina, recent myocardial infarction (MI), cerebrovascular accident (CVA), and hepatic or renal disease (guanabenz and guanfacine).
Parameters to monitor
■ CBC—positive Coombs test in 25% of those tested; less than 1% develop hemolytic anemia (methyldopa)
■ Sleep disturbances, drowsiness, or dry mouth
■ Symptoms of depression
■ Impotence
■ Pulse
■ Rebound hypertension
Table 12-11. Peripherally Acting α1-Adrenergic Blockers
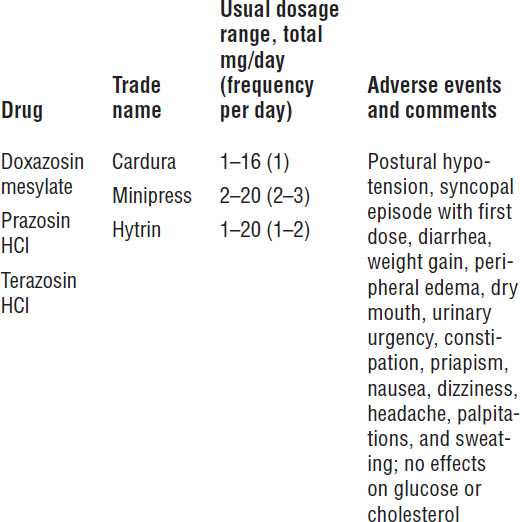
Reprinted with permission from JNC-VII.
Peripherally acting α1-adrenergic blockers
See Table 12-11 for a list of peripherally acting α1-adrenergic blockers, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
■ Peripheral α1 postsynaptic receptors are blocked, which causes vasodilation of both arteries and veins (indirect vasodilators).
■ These agents cause less reflex tachycardia than do direct vasodilators (hydralazine and minoxidil).
Patient instructions and counseling
■ Take first dose of no more than 1 mg of any agent, and take at bedtime.
■ Rise slowly from a lying or sitting position.
■ Medication may cause dizziness.
■ Priapism is possible.
Drug–drug and drug–disease interactions
■ NSAIDs decrease antihypertensive effects of α1-blockers.
■ Increased antihypertensive effects occur with diuretics and β-blockers.
Parameters to monitor
■ BP and pulse
■ Peripheral edema
β-blockers
See Table 12-12 for a list of β-blockers, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
These medications competitively block response to β-adrenergic stimulation:
■ Block secretion of renin
■ Decrease cardiac contractility, thereby decreasing cardiac output
■ Decrease central sympathetic output
■ Decrease heart rate, thereby decreasing cardiac output
Patient instructions and counseling
■ Report symptoms of dizziness or hypotension.
■ Exercise sedation precautions (with lipid-soluble compounds).
■ Abrupt withdrawal of the drug should be avoided.
■ Sexual dysfunction is possible.
Drug–drug and drug–disease interactions
■ Use with caution in patients with diabetes.
■ Use with caution in patients with Raynaud’s phenomenon or peripheral vascular disease.
■ β-blockers may decrease the effectiveness of sulfonylureas.
■ Nondihydropyridines may increase the effect and toxicity of β-blockers.
Parameters to monitor
■ ECG
■ Rebound hypertension
■ Cholesterol levels
■ Pulse (apical and radial)
■ Glucose levels
Direct Vasodilators
This medication class (second-line agents) is best avoided unless necessary to treat refractory hypertension that is unresponsive to all other agents.
These agents should not be used alone secondary to increases in plasma renin activity, cardiac output, and heart rate and should therefore be used only when β-blockers and diuretics are part of the antihypertensive regimen.
Table 12-12. β-Blockers and Combination α- and β-Blockers
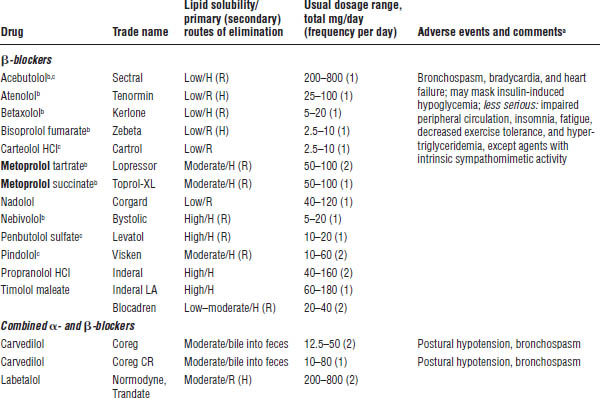
Adapted from JNC-VII.
H, hepatic; R, renal.
a. Adverse events, or side effects, listed are for the class of drugs.
b. Cardioselective.
c. Intrinsic sympathomimetic activity.
See Table 12-13 for a list of direct vasodilators, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
These agents cause direct relaxation of peripheral arterial smooth muscle and thereby significantly decrease peripheral resistance.
Patient instructions and counseling
■ Report symptoms of dizziness or hypotension.
■ Hirsutism is possible (minoxidil).
■ Report any new symptoms of fatigue, malaise, low-grade fever, and joint aches.
■ Report rapid weight gain (> 5 pounds), unusual swelling, and pulse increases of > 20 beats per minute above normal.
■ Rise slowly from a lying or sitting position.
Table 12-13. Direct Vasodilators
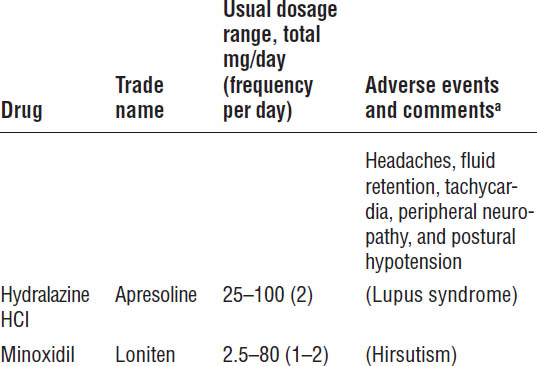
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
a. Adverse events, or side effects, listed are for the class of drugs, except where noted for individual drugs (in parentheses).
Drug–drug and drug–disease interactions
■ Use with caution in patients with pulmonary hypertension.
■ Use with caution in patients with significant renal failure or CHF.
■ Use with caution in patients with coronary artery disease or a recent MI.
Parameters to monitor
■ Weight (fluid status)
■ BP and pulse
■ CBC with antinuclear antibody test (hydralazine)
Calcium Antagonists
Low-renin hypertensive, African American, and elderly patients respond well to this class of medications. See Table 12-14 for a list of calcium antagonists, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
■ Calcium antagonists inhibit the influx of calcium ions through slow channels in vascular smooth muscle and cause relaxation of both coronary and peripheral arteries.
■ These agents cause sinoatrial (SA) and atrioventricular (AV) nodal depression and a decrease in myocardial contractility (nondihydropyridines).
Patient instructions and counseling
■ Report symptoms of dizziness or hypotension.
■ Constipation is possible (verapamil).
■ Report any new symptoms of shortness of breath, fatigue, or increased swelling of the extremities.
■ Rise slowly from a lying or sitting position.
Drug–drug and drug–disease interactions
■ Use with caution in patients on β-blockers (nondihydropyridines), which may increase CHF and bradycardia. This combination can also cause conduction abnormalities to the AV node.
■ Use with extreme caution in patients with conduction disturbances in the SA or AV node.
■ Grapefruit juice may increase the levels of some dihydropyridines.
Parameters to monitor
■ ECG
■ Peripheral edema
Table 12-14. Calcium Antagonists
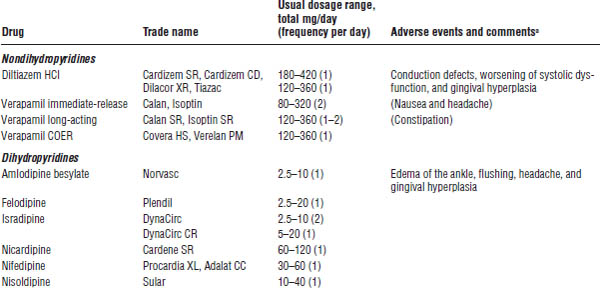
Adapted from JNC-7 Express, National Heart, Lung, and Blood Institute.
a. Adverse events, or side effects, listed are for the class of drugs, except where noted for individual drugs (in parentheses).
■ Bowel habits
■ Symptoms of conduction disturbances
Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers
Ethnic differences exist in the response to these classes of medications. These agents are relatively ineffective as monotherapy in African American patients. However, the addition of diuretic therapy has been shown to sensitize African American patients to these agents to obtain similar responses as in non–African American patients.
See Table 12-15 for a list of ACEIs and ARBs, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
ACEIs
■ ACEIs inhibit the conversion of angiotensin I to angiotensin II (a potent vasoconstrictor; see Figure 12-1).
■ These agents indirectly inhibit fluid volume increases by inhibiting angiotensin II–stimulated release of aldosterone.
ARBs
■ ARBs inhibit the binding of angiotensin II to the angiotensin II receptor, thereby inhibiting the vasoconstrictive properties of angiotensin II as well as its ability to stimulate the release of aldosterone.
■ These agents are currently considered as alternative therapy in patients not able to tolerate ACEIs because of cough.
Table 12-15. Angiotensin-Converting Enzyme Inhibitors and Angiotensin II Receptor Blockers
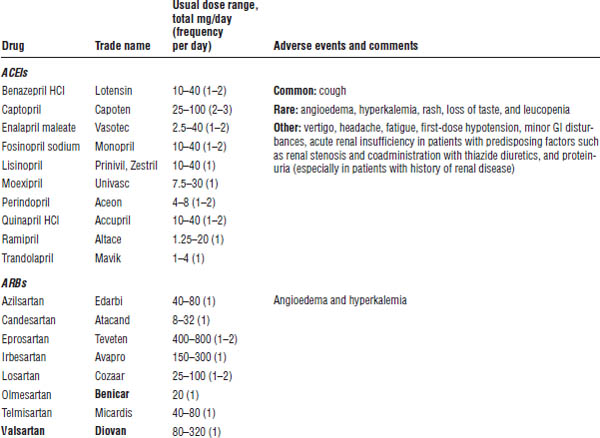
Adapted from JNC-VII.
Boldface indicates one of top 100 drugs for 2012 by units sold at retail outlets, www.drugs.com/stats/top100/2012/units.
GI, gastrointestinal.
Patient instructions and counseling
■ Report symptoms of dizziness or hypotension.
■ Symptoms of swelling of the lips, mouth, or face should be considered an emergency. Report immediately to a doctor’s office or an emergency department.
■ Report new rashes (especially with captopril).
■ Do not use salt substitutes containing potassium, and do not take OTC potassium supplements.
■ Rise slowly from a lying or sitting position.
Drug–drug and drug–disease interactions
■ NSAIDs will decrease the effectiveness of ACEIs and ARBs.
■ Potassium-sparing diuretics, potassium supplements, and salt substitutes will increase the risk of hyperkalemia when used in combination with ACEIs and ARBs.
■ ACEIs and ARBs should be avoided in patients with bilateral renal artery stenosis or stenosis in a single kidney.
■ ACEIs and ARBs should be avoided in pregnant patients.
Parameters to monitor
■ Serum electrolytes (especially creatinine and potassium)
■ Symptoms of angioedema
■ BP
■ Symptoms of hypotension
■ CBC (especially with captopril and enalapril) for neutropenia, which is more common in patients with preexisting renal impairment
■ Cough
■ Urinary proteins
Direct Renin Inhibitors
See Table 12-16 for a list of direct renin inhibitors, their usual dosage range, and adverse effects associated with these medications.
Mechanism of action
Direct renin inhibitors competitively inhibit human renin, which decreases plasma renin activity and inhibits the conversion of angiotensinogen to angiotensin I.
Table 12-16. Direct Renin Inhibitors
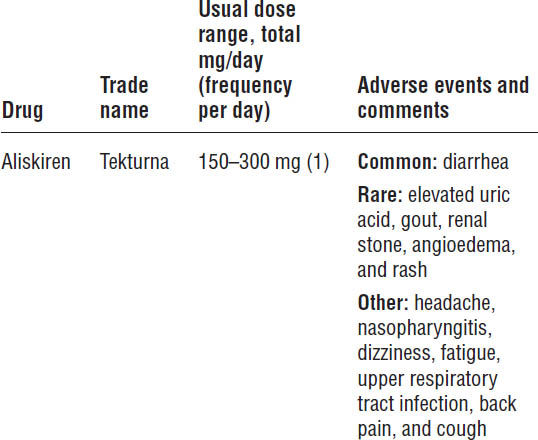
Tekturna [package insert]. East Hanover, NJ: Novartis Pharmaceuticals; revised March 2012.
Patient instructions and counseling
■ Medicine can be taken with or without food.
■ Establish a routine pattern for taking aliskiren with regard to meals. High-fat meals decrease absorption significantly.
■ Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light.
■ Report symptoms of dizziness or hypotension.
■ Diarrhea is possible.
■ Symptoms of swelling of the lips, mouth, or face should be considered an emergency. Report immediately to a doctor’s office or an emergency department.
Drug–drug and drug–disease interactions
■ Concomitant use of aliskiren with cyclosporine is not recommended.
■ Potassium-sparing diuretics, potassium supplements, and salt substitutes will increase the risk of hyperkalemia when used in combination with aliskiren.
■ Blood concentrations of furosemide are significantly reduced when given with aliskiren.
■ Ketoconazole significantly increases aliskiren plasma levels.
■ Aliskiren should be avoided in pregnant patients.
■ According to recent trial data, the combination of ACEI or ARB with aliskiren should be avoided.
Parameters to monitor
■ Symptoms of angioedema
■ BP
■ Symptoms of hypotension
■ Serum electrolytes (especially creatinine and potassium)
12-6. Hypertensive Urgencies and Emergencies
The classification of hypertensive urgencies and emergencies is determined by the presence or absence of acute target organ damage, not by BP, and determines the appropriate treatment approach.
The relative rise and rate of increase in BP is more important than the actual BP.
Hypertensive Emergencies
Acute elevations of BP (> 180 mm Hg systolic or > 120 mm Hg diastolic) with the presence of acute or ongoing target organ damage constitute a hypertensive emergency (Box 12-4). This situation requires immediate lowering of BP to prevent or minimize target organ damage.
Table 12-17 shows details of parenteral drugs used for treatment of hypertensive emergencies. Such emergencies should be treated as follows:
■ As an initial goal, reduce mean arterial pressure (MAP) by no more than 25% within minutes to hours. Reach BP of 160/100 mm Hg within 2–6 hours.
■ Measure BP every 5–10 minutes until goal MAP is reached and life-threatening target organ damage resolves.
■ Maintain goal BP for 1–2 days, and further reduce BP toward normal over several weeks.
■ Excessive falls in BP may precipitate renal, cerebral, or coronary ischemia.
Box 12-4. Clinical Findings of Target Organ Damage
Target Organ Damage
Hypertensive encephalopathy
Intracranial hemorrhage
Unstable angina
Acute myocardial infarction
Acute left ventricular failure with pulmonary edema
Dissecting aortic aneurysm
Eclampsia
Clinical Findings
Funduscopic: papilledema, hemorrhage, exudates
Neurologic: somnolence, confusion, seizures, coma, visual deficits or blindness
Cardiac: S4 gallop, ischemic changes on ECG, chest x-ray consistent with pulmonary edema, chest pain
Renal: oliguria, progressive azotemia, hematuria, proteinuria
Other: dyspnea
Reprinted with permission from JNC-VII.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree