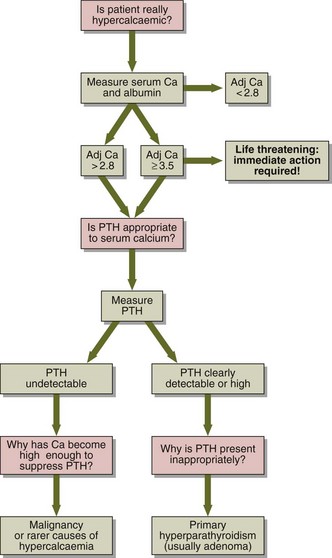
36 A diagnostic decision chart is shown in Figure 36.1. Primary hyperparathyroidism is most often due to a single parathyroid adenoma, which secretes PTH independently of feedback control by plasma calcium. Hypercalcaemia associated with malignancy is the commonest cause of a high calcium in a hospital population. Some tumours secrete a protein called PTHrP (parathyroid hormone-related protein), which has PTH-like properties. Rarer causes of hypercalcaemia include:
Hypercalcaemia
Diagnosis
 Inappropriate dosage of vitamin D or metabolites, e.g. in the treatment of hypoparathyroidism or renal disease or due to self-medication.
Inappropriate dosage of vitamin D or metabolites, e.g. in the treatment of hypoparathyroidism or renal disease or due to self-medication.
 Granulomatous diseases (such as sarcoidosis or tuberculosis) or certain tumours (such as lymphomas) synthesize 1,25-dihydroxycholecalciferol.
Granulomatous diseases (such as sarcoidosis or tuberculosis) or certain tumours (such as lymphomas) synthesize 1,25-dihydroxycholecalciferol.
 Thyrotoxicosis very occasionally leads to increased bone turnover and hypercalcaemia.
Thyrotoxicosis very occasionally leads to increased bone turnover and hypercalcaemia.
 Thiazide therapy: the hypercalcaemia is usually mild.
Thiazide therapy: the hypercalcaemia is usually mild.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Hypercalcaemia