Chapter 3
How Does Multimorbidity Affect Patients?
Elizabeth A. Bayliss
Kaiser Permanente Institute for Health Research, Department of Family Medicine, University of Colorado School of Medicine, USA
Overview
- Greater morbidity burden can be associated with lower quality of life, lower physical function and poor emotional well-being
- Highly symptomatic conditions that affect quality of life for patients are highly prevalent; however, clinical care and biomedical research tend to prioritize treatment of conditions that increase mortality and resource use
- Assessing and understanding patient’s perceptions and priorities are important for planning care for populations and for individuals
- Multimorbidity management should focus on maximizing self-care potential, supporting patients (and their caregivers) and insuring good care coordination and continuity of care.
Background
Multimorbidity affects all aspects of patients’ lives. People with multimorbidity have more requirements for health care—including visits to health professionals, hospitalizations and use of emergency services. Having multiple conditions increases patients’ risk of disability, causes more physical limitations and affects individuals’ ability to care for themselves. Quality of life (QOL), emotional well-being and social interactions may also be affected. People with multimorbidity are less likely to be employed to contribute economically on a personal level and on a societal level. However, not all persons with multimorbidity experience adverse effects: certain combinations of conditions have greater effects than others; and patients have a range of personal, social and societal resources to draw upon for self-care.
Perceptions of multimorbidity
Morbidity burden is in the eye of the beholder. While patients are likely to define multimorbidity in terms of conditions and symptoms that affect function, clinicians are likely to refer to coexisting
Box 3.1
What are the main patient-perceived outcomes associated with greater morbidity burden?
What kind of multimorbidity measures are more appropriate to accurately assess symptom burden?
What kind of multimorbidity measures are more appropriate to accurately predict mortality, cost or care and hospitalization?
diseases. Patients may describe functional limitations such as back pain plus shortness of breath, while clinicians may be concerned about the long-term effects of hypertension and hyperlipidaemia on renal function. Making care decisions requires understanding and incorporating varying perspectives.
On a population level, specific measures of morbidity establish associations between morbidity burden and patient outcomes. It is necessary to use appropriate measures to accurately assess the effects of morbidity burden on patients. Measures that incorporate patient input are more likely to give an accurate assessment of symptom burden; while measures that are based on diagnosis codes and other objective data are more likely to give an accurate assessment of mortality risk, cost of care, risk of hospitalization and other more objective outcomes (Figure 3.1). It is clear that multimorbidity, in general, is associated with increased mortality, higher rates of hospitalization, decrease in functional status, increased financial burdens of medical care and lower quality of life (Box 3.1).
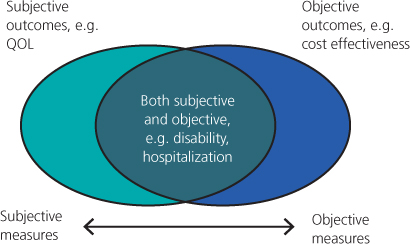
Figure 3.1 Different measures are associated with different outcomes.
Mortality and hospitalization
Although the simplest proxy for degree of morbidity is age (with older age associated with more multimorbidity), having more coexisting chronic conditions is associated with higher rates of mortality that is independent of age. Within populations of people with multimorbidity, mortality is higher among subgroups characterized by certain chronic conditions such as congestive heart failure, cancer, chronic lung disease, and advanced hepatic and renal diseases. Although more multimorbidity is clearly associated with lower socio-economic status that is associated with mortality, it is unclear whether the association between morbidity and mortality is greater in groups characterized by low socio-economic status.
Risk of hospitalization follows similar patterns. People with multimorbidity are more likely to be hospitalized for a range of conditions than those with no chronic conditions—independent of age group and in populations of all ages. Mental as well as physical comorbidities affect hospitalization, although diseases of circulatory, respiratory and metabolic systems and oncology are particularly influential. Hospitalizations can also result from complications of treating multiple conditions such as adverse drug reactions and medical errors.
Functional status and quality of life
Overall, greater multimorbidity is associated with lower reported physical well-being and lower functional status. In contrast to multimorbidity associated with mortality and hospitalization, coexisting conditions that limit physical functioning tend to be those that are highly prevalent and most symptomatic to patients, such as back pain, obesity, arthritis, visual impairments and chronic cardiopulmonary disease. Mental illness as a comorbidity also has a consistently negative effect and likely interacts with other conditions to affect functional status. A subset of symptomatic conditions (musculoskeletal, hearing, vision, diabetes or depression) are specifically associated with work limitations—which may affect patients’ economic well-being as well as their physical quality of life. Low functional status because of multimorbidity may also affect friends and family members who act as either formal or informal caregivers for patients. Care for individuals with functional limitations is usually uncompensated and are difficult to quantify, but is of a far greater magnitude on a population level than formal caregiving (Figure 3.2).
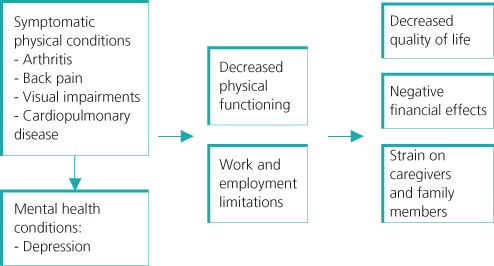
Figure 3.2 Example causes and effects of decreased functional status because of multimorbidity.
As chronic conditions increase in severity and number, they have a greater effect on QOL in general. In addition to physical functioning, QOL is also a function of age, emotional well-being, population and cultural norms, and social support, among other factors. Greater multimorbidity of physical conditions is associated with a lower emotional well-being and a greater risk of depression, and this is especially true for populations with painful physical symptoms. And in populations with multiple chronic medical conditions, depression contributes to mental functioning, disability and quality of life.
The effect of multimorbidity on various domains of QOL is nonlinear and age dependent: an initial condition may have a substantial effect on self-rated health in some age groups; and in all age groups having approximately four or more conditions appears to particularly affect physical functioning and emotional well-being. The effect of multimorbidity on QOL is further moderated by variable adaptation to the effects of total disease burden. Individuals with low self-efficacy, poor problem-solving skills and less social support and with higher degrees of helplessness appear to experience more negative effects of multimorbidity on QOL.
Thus, supporting patient characteristics that improve self-care and physical and emotional functioning may improve QOL for individuals with multimorbidity. Interventions to promote self-efficacy, improve problem-solving approaches to illness, treat depressive disorders, provide adequate pain management for musculoskeletal conditions and maximize social support should be explored for all eligible patients.
Patient experiences
Townsend et al. (2003) found that patients’ ‘…experience of multiple morbidity [is] characterized by fluctuating symptoms, fear, uncertainty and lack of control’. They report barriers to the care process that reflect the magnitude of their disease burden—and perceived barriers increase with the level of morbidity.
Patient-reported barriers to self-management include financial constraints, having symptoms and treatments that interfere with each other, physical limitations, ‘hassles’ with interacting with the healthcare system, decreased medication adherence and a need to prioritize care (Box 3.2).
Multimorbidity requires attention to the collaborative care needs of patients and clinicians. Interactions with the healthcare system are particularly problematic. People with multimorbidity may see numerous different doctors and nurses over the course of a year, and doctors treating multimorbid populations may address several different problems at each visit. This may result in miscommunications and conflicting messages to patients. Patients may also receive conflicting information from different healthcare providers and experience unnecessary or duplicative tests. Unsurprisingly, this can result in lower patient-reported ratings of communication—even for concordant conditions with similar management strategies. One result of miscommunication is that patients with greater multimorbidity may feel that they are obtaining lower quality care (Shadmi et al., 2006).
This frustration is mirrored by clinicians, who struggle with prioritizing the healthcare demands of patients with multimorbidity
Box 3.2 Patient vignette
I take quite a few pills, quite a bit of medication, but I have that all laid out at home. I put a week’s supply out once a week so I know when to take my pills. Some of them I take in the morning, some of them in the afternoon or early afternoon and then a few at night when I am ready to go to bed…my basic problems are diabetes and heart…and high blood pressure of course. What else? Arthritis. I elevate my legs to take care of the arthritis in the knees because they tell me that it is the changing weather…I try to watch my diet…the single thing that bothers me the most is my diminished capacity to do things that I particularly enjoy doing—a lot now depends on my wife…I think the primary concern I have got is weight management. I managed to lose over 30 pounds after my heart surgery…and I have gained it all back…that was before I started on insulin…I used to bike around the neighbourhood, but one of the things that I have lost is balance…and I could not do much in the way of walking, because of the sciatica…and I have had a little bit of diabetes haemorrhaging in my left eye which bothers me…so arthritis in my knees and ankles and back is the most troublesome…and I am not tolerant of the opiate family of drugs at all—I itch like crazy—so acetaminophen is my primary pain medication…It actually has no impact on my work since I am punching my keyboard and talking on the phone…and as long as I can be productive I want to work.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


