CHAPTER 56 Heart and great vessels
PERICARDIUM
FIBROUS AND SEROSAL PERICARDIUM
Serosal pericardium
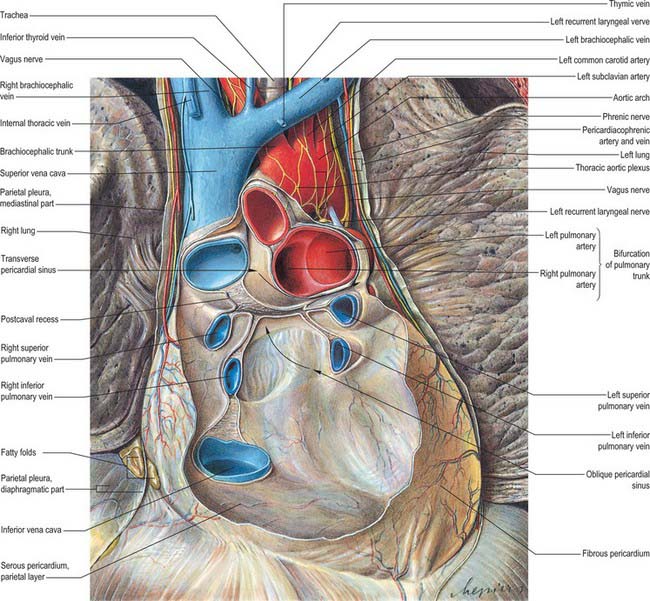
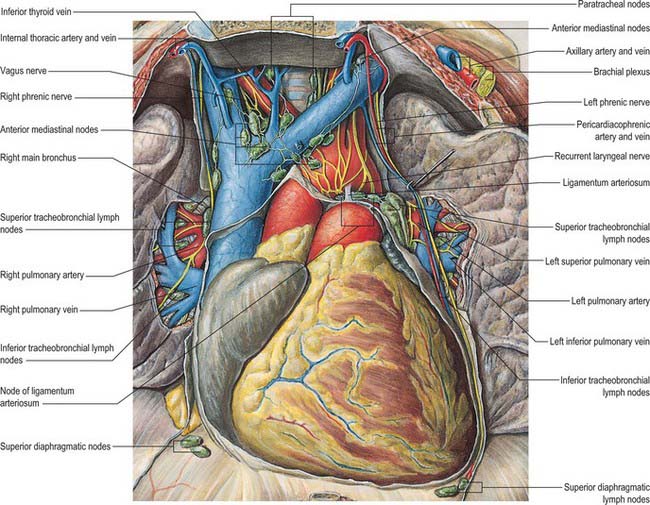
The serosal pericardium is a closed sac within the fibrous pericardium, and has a visceral and a parietal layer. The visceral layer, or epicardium, covers the heart and great vessels and is reflected into the parietal layer, which lines the internal surface of the fibrous pericardium. The reflections of the serosal layer are arranged as two complex ‘tubes’: the aorta and pulmonary trunk are enclosed in one, and the superior and inferior venae cavae and the four pulmonary veins in the other. The tube surrounding the veins has the shape of an inverted J. The cul-de-sac within its curve is behind the left atrium and is termed the oblique sinus. The transverse sinus is a passage between the two pericardial ‘tubes’ (Fig. 56.1). It has the aorta and pulmonary trunk in front and the atria and great veins behind (see Fig. 56.2B,D). The arrangement of the oblique and transverse sinuses, along with that of the main ‘principal’ cavity, is further affected by the development of complex three-dimensional pericardial recesses between adjacent structures. These recesses can be grouped according to the siting of their orifices or ‘mouths’. From the principal pericardial cavity, the postcaval recess projects towards the left behind the atrial termination of the superior vena cava. It is limited above by the right pulmonary artery and below by the upper right pulmonary vein. Its mouth opens superolaterally to the right. The right and left pulmonary venous recesses each project medially and upwards on the back of the left atrium between the superior and inferior pulmonary veins on each side, indenting the side walls of the oblique sinus. The superior aortic recess extends from the transverse sinus. From its mouth, located inferiorly, it ascends posterior to, then to the right of, the ascending aorta and ends at the level of the sternal angle. The inferior aortic recess, also extending from the transverse sinus, is a diverticulum descending from a superiorly located mouth to run between the lower ascending part of the aorta and the right atrium. The left pulmonary recess, with its mouth under the fold of the left vena cava, passes to the left between the inferior aspect of the left pulmonary artery and the upper border of the superior left pulmonary vein. The right pulmonary recess lies between the lower surface of the proximal part of the right pulmonary artery and the upper border of the left atrium.
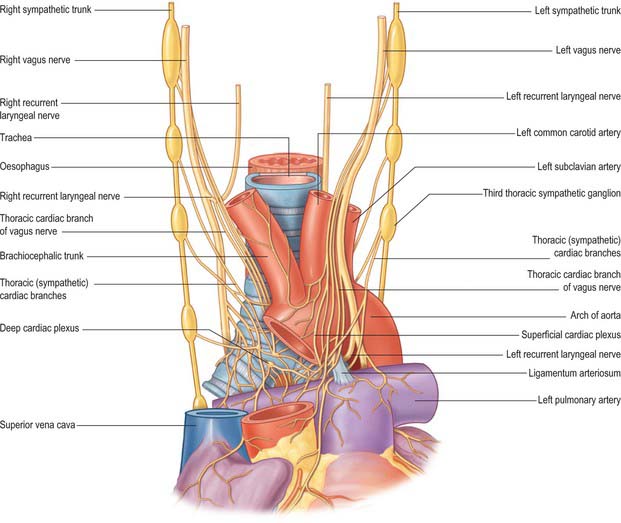
INNERVATION
The pericardium is innervated by the vagus, together with phrenic nerves and the sympathetic trunks (see Fig. 56.20; see Fig. 58.3). Pericardial pain is typically a sharp severe substernal pain. It may be exacerbated by lying back or on the left side and relieved by leaning forward. It occasionally radiates to the upper border of trapezius.
HEART
The microstructure of cardiac muscle is described in detail in Chapter 6.
GENERAL ORGANIZATION
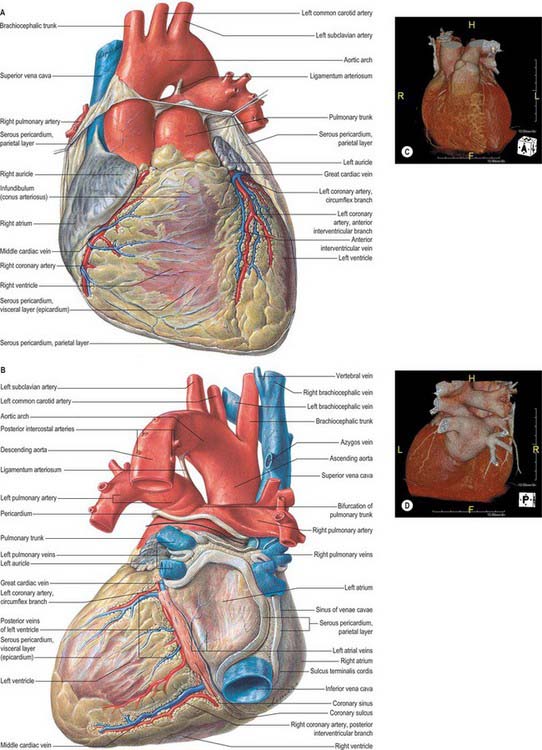
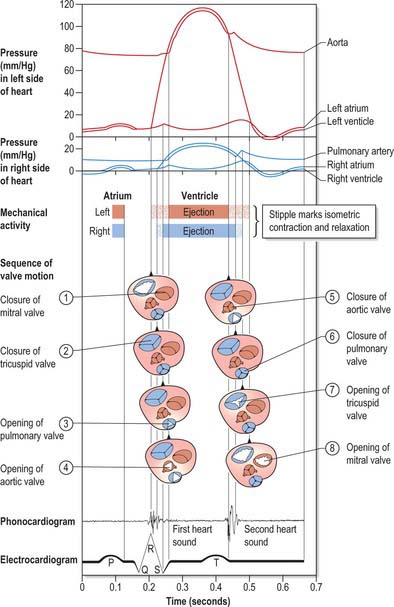
The heart is a pair of valved muscular pumps combined in a single organ (Fig. 56.2A–D). Although the fibromuscular framework and conduction tissues of these pumps are structurally interwoven, each pump (the so-called ‘right’ and ‘left’ hearts) is physiologically separate, and is interposed in series at different points in the double circulation. Despite this functional disposition in series, the two pumps are usually described topographically in parallel.
The left heart starts at the left atrium, which receives all the pulmonary inflow of oxygenated blood and some coronary venous inflow. It contracts to fill the left ventricle through the left atrioventricular orifice guarded by its mitral valve. The valve is the entry to the inlet of the left ventricle. Ventricular contraction rapidly increases the pressure in the apical trabecular component, closing the mitral valve and opening the aortic valve, enabling the ventricle to eject via the left ventricular outflow tract into the aortic sinuses and the ascending aorta, and thence to the entire systemic arterial tree, including the coronary arteries. This vast vascular bed presents a high peripheral resistance that, with large metabolic demands (especially the sustained requirements of the cerebral tissues), explains the more massive structural organization of the ‘left heart’. The ejection phase of the left ventricle is shorter than that of the right, but its fluctuations in pressure are very much greater. Because of its contrasting functional demands, the heart is far from a simple pair of (structurally combined) parallel pumps, even though the right and left ventricles must deliver more or less the same volume with each contraction. The heart has a complicated, spiral, three-dimensional organization which is markedly skewed when compared with the planes of the body. Terms such as ‘left’ and ‘right’, ‘anterior’ and ‘posterior’, ‘superior’ and ‘inferior’, therefore, do not always assist the descriptions of cardiac anatomy. Another potential source of confusion is the usual study of isolated whole or dissected hearts, with the subsequent difficulty in relating details to the heart as it is positioned within the body. The following preliminary description emphasizes such difficulties in order to circumvent certain misconceptions, before proceeding to an account of more detailed structure.
Cardiac size, shape and external features
The heart is a hollow, fibromuscular organ of a somewhat conical or pyramidal form, with a base, apex and a series of surfaces and ‘borders’. Enclosed in the pericardium, it occupies the middle mediastinum between the lungs and their pleural coverings (Fig. 56.1). It is placed obliquely behind the body of the sternum and the adjoining costal cartilages and ribs. Approximately one-third of the mass lies to the right of the midline.
An average adult heart is 12 cm from base to apex, 8–9 cm at its broadest transverse diameter and 6 cm anteroposteriorly. Its weight varies from 280 to 340 g (average 300 g) in males and from 230 to 280 g (average 250 g) in females. Cardiac weight is 0.45% of body weight in males and 0.40% in females. Adult weight is achieved between the ages of 17 and 20 years. The oblique position of the heart may be emphasized by comparing it to a rather deformed pyramid, with the base facing posteriorly and to the right, and the apex anteriorly and to the left. A line from the apex to the approximate centre of the base, projected posterolaterally, emerges near the right midscapular line. Some surfaces of the cardiac ‘pyramid’ are flat, others more or less convex, these aspects merging along rather ill-defined ‘borders’. Precise definition of surfaces and intervening ‘borders’ is, therefore, difficult. In the account that follows, official nomenclature (Terminologia Anatomica 1998) and more generally used terms from clinical practice are given as alternatives. The heart is described as having a base and apex, its surfaces being designated as sternocostal (anterior), diaphragmatic (inferior) and right and left (pulmonary). Its borders are termed upper, inferior (‘acute’ margin or border) and left (‘obtuse’ margin or border). Some name the right surface a ‘border’, despite its extent. One avoidable source of confusion is the use of ‘posterior’, which can be replaced with the unambiguous term ‘diaphragmatic’. If posterior is to be used for a cardiac surface, it should be reserved for the base. (However, compounding this difficulty, there are a number of different usages of the term ‘cardiac base’.)
The heart is placed obliquely in the thorax. The atrial and ventricular septal structures are virtually in line, but inclined forwards and to the left at 45° to a sagittal plane. The planes of the mitral and tricuspid valves, although vertical and not precisely co-planar, are broadly at right angles to the septal plane. The right atrium, therefore, is not only to the right, but also anterior and inferior to the left atrium. It is also partly anterior to the left ventricle, an important atrioventricular septum intervening. The right ventricle forms most of the anterior aspect of the ventricular mass (Fig. 56.3), only its inferior end is to the right of the left ventricle, its upper left extremity (pulmonary orifice) is to the left and superior relative to the aortic valve. The left atrium forms most of the posterior aspect of the heart, whereas the left ventricle is only prominent inferiorly, running along the left margin to reach the apex. The atria are essentially right of and posterior to their respective ventricles. These general dispositions are of the greatest importance in planning or interpreting radiographs, scans, angiocardiograms and echocardiograms.
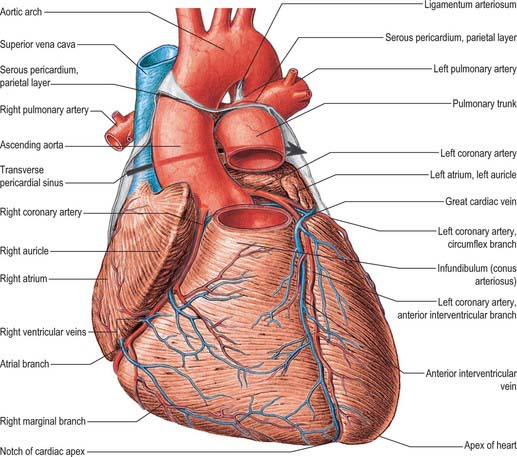
Grooves on the cardiac surface
The division of the heart into four chambers produces boundaries that are visible externally as grooves (sulci). Some are deep and obvious and contain prominent structures. Others are less distinct, even barely perceptible, and are sometimes obscured, in part, by the major structures that cross them. The interatrial groove is a shallow groove separating the two atria. The lateral limits are defined by the borders of the atria. The atrioventricular (coronary) groove (or sulcus) separates the atria from the ventricles. This groove, containing the main trunks of the coronary arteries, is oblique. It descends to the right on the sternocostal surface, separating the right atrium (and its auricle or appendage) from the oblique right margin of the right ventricle and its infundibulum. Its upper left part is obliterated where it is crossed by the pulmonary trunk and, behind this, the aorta, from which the coronary arteries originate. Continuing to the left, the groove curves around the ‘obtuse’ margin and descends to the right, separating the atrial base from the diaphragmatic surface of the ventricles (Fig. 56.2A,D). This diaphragmatic part of the atrioventricular groove then curves around the ‘acute’ margin at its lower right end to become confluent with the sternocostal part. Thus the groove passes from high on the left to low on the right, with the diaphragmatic part being a little to the left of the sternocostal. A section that includes the atrioventricular groove is at 45° to the sagittal plane and at a greater but variable angle to the transverse and coronal planes. It approximately traverses the lines of attachment of the atrioventricular valves and (even less precisely) those of the aortic and pulmonary valves. A line at right angles to the centre of this plane will descend forwards and leftwards to the cardiac apex.
Cardiac base, apex, surfaces and borders
The true cardiac base is somewhat quadrilateral, with curved lateral extensions. It faces back and to the right, separated from the thoracic vertebrae (fifth to eighth in the recumbent, sixth to ninth in the erect posture) by the pericardium, right pulmonary veins, oesophagus and aorta. It is formed mainly by the left atrium, and only partly by the posterior part of the right atrium (Fig. 56.2B,D). It extends superiorly to the bifurcation of the pulmonary trunk and inferiorly to the posterior part of the atrioventricular groove, which contains the coronary sinus and branches of the coronary arteries. It is limited to the right and left by the rounded surfaces of the corresponding atria. These are separated by the shallow interatrial groove. The point of junction of the atrioventricular, interatrial and posterior interventricular grooves is termed the crux of the heart. Two pulmonary veins on each side open into the left atrial part of the base, whereas the superior and the inferior vena cava open into the upper and lower parts of the right atrial basal region. The area of the left atrium between the openings of right and left pulmonary veins forms the anterior wall of the oblique pericardial sinus (Fig. 56.1). This description of the anatomical base reflects the usual position of the heart in the thorax. Some confusion is produced by other current usages of the term ‘base’. It is often applied to the segment of the atrioventricular and ventriculoarterial junctions seen after dissections through the atrioventricular groove. This area is better termed the base of the ventricles. In clinical practice, auscultation in or near the parasternal parts of the second intercostal spaces is often described as occurring at the clinical ‘base’, to make the contrast with the clinical ‘apex’. Such descriptions, while less than perfect anatomically, will almost certainly persist.
Anterior, sternocostal surface of the heart
Facing forwards and upwards, the anterior surface has an acute right and a more gradual left convexity (Fig. 56.3). It consists of an atrial area above and to the right, and a ventricular part below and to the left of the atrioventricular groove. The atrial area is occupied almost entirely by the right atrium. The left atrium is largely hidden by the ascending aorta and pulmonary trunk. Only a small part of the left appendage projects forwards to the left of the pulmonary trunk. Of the ventricular region, about one-third is made up by the left and two-thirds by the right ventricle. The site of the septum between them is indicated by the anterior interventricular groove. The sternocostal surface is separated by the pericardium from the body of the sternum, the sternocostal muscles and the third to the sixth costal cartilages. Because of the bulge of the heart to the left, more of this surface is behind the left costal cartilages than behind the right ones. It is also covered by the pleural membranes and by the thin anterior edges of the lungs, except for a triangular area at the cardiac incisure of the left lung. The lungs and their pleural coverings are variable in their degree of overlap of the heart.
Inferior, diaphragmatic surface of the heart
Largely horizontal, the inferior surface of the heart slopes down and forwards a little towards the apex (Fig. 56.2B,D). It is formed by the ventricles (chiefly the left) and rests mainly upon the central tendon but also, apically, on a small area of the left muscular part of the diaphragm. It is separated from the anatomical base by the atrioventricular groove and is traversed obliquely by the posterior interventricular groove.
This is atrial (mainly the left atrium). Anterior to it are the ascending aorta and the pulmonary trunk (Fig. 56.1). At its extremity, the superior vena cava enters the right atrium.
Right atrium
General and external features
The interatrial septum (or atrial septum) is oblique, so the right atrium is both anterior and to the right of the left atrium (Fig. 56.2A–D), also extending inferior to it. Its walls form the right upper sternocostal surface, the convex right (pulmonary surface) and a little of the right side of the anatomical base. The superior vena cava opens into its dome and the inferior vena cava into its lower posterior part (Fig. 56.2B,D). An extensive muscular pouch, the auricle, projects anteriorly to overlap the right side of the ascending aorta. The auricle is a broad, triangular structure and has a wide junction with the true atrial component of the atrium (Fig. 56.2A,C). The junction between the venous part (sinus venosus) and the atrium proper is marked externally by a shallow groove, the sulcus terminalis, extending between the right sides of the openings of the two venae cavae. The sulcus terminalis corresponds, internally, to the terminal crest (crista terminalis) which is the site of origin of the extensive pectinate muscles that arise serially at right angles from the crest. Posteriorly, the vertical interatrial groove descends to the crux.
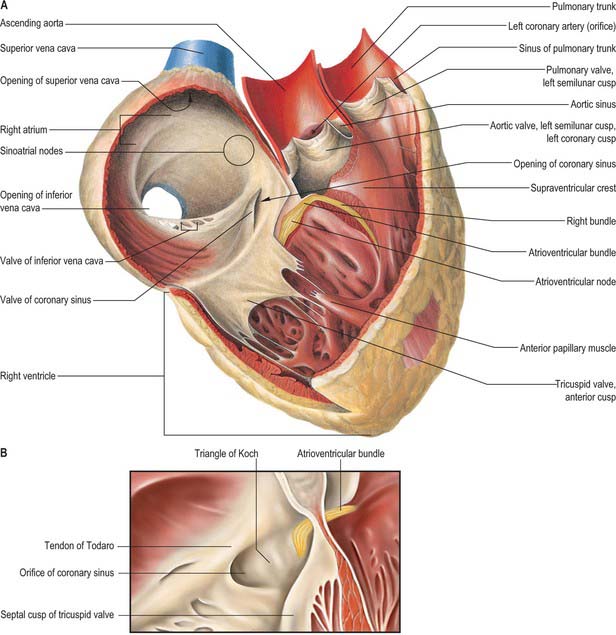
Interior surface
The interior surface of the right atrium can be divided into three regions: a smooth-walled venous component posteriorly that leads, anteriorly, to the vestibule of the tricuspid valve and the auricle (Fig. 56.4A,B). The wall of the vestibule is smooth, but its junction with the auricle is ridged all around the atrioventricular junction. The smooth-walled part receives the opening of the venae cavae and the coronary sinus. It represents the venous component (sinus venosus) of the developing heart. The wall of the vestibule has a ridged surface and that of the auricle is trabeculated. Both are derived from the embryonic atrium proper.
The superior and inferior venae cavae open into the venous component. The superior vena cava returns blood from head, neck and upper limb through an orifice that faces inferoanteriorly and has no valve, and also receives blood from the chest wall and the oesophagus via the azygos system. The inferior vena cava is larger than its superior counterpart: it drains blood from all structures below and including the diaphragm into the lowest part of the atrium near the septum. Anterior to its orifice is a flap-like valve, the Eustachian valve or valve of the inferior vena cava (Fig. 56.4A,B). Of varying size, this valve is found along the lateral, or right, margin of the vein. When traced inferiorly, it runs into the sinus septum (see below), where it is contiguous with the valve of the coronary sinus. The lateral part of the Eustachian valve becomes continuous with the lower end of the terminal crest. The valve is a fold of endocardium enclosing a few muscular fibres. It is large during fetal life, when it serves to direct richly oxygenated blood from the placenta through the foramen ovale of the atrial septum into the left atrium. The valve varies markedly in size in postnatal life; it is sometimes cribriform or filamentous but often is absent. A particularly prominent recess, behind the Eustachian valve, is seen posteroinferiorly relative to the ostium of the coronary sinus.
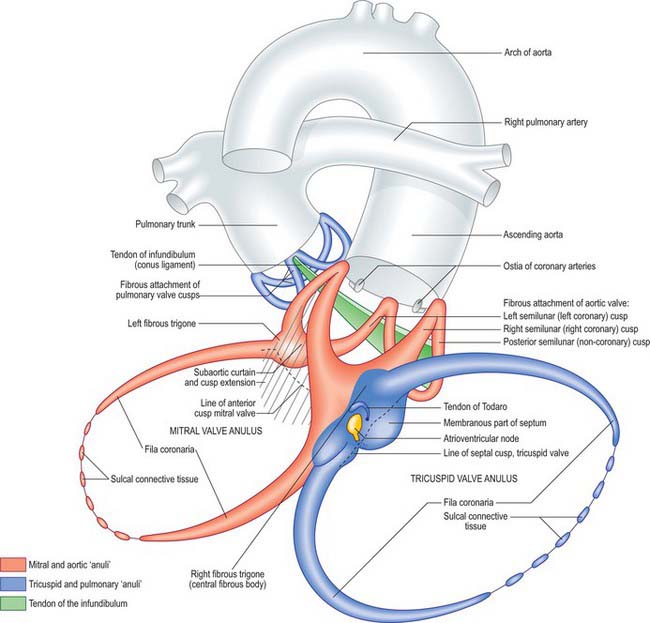
The coronary sinus opens into the venous atrial component between the orifice of the inferior vena cava, the fossa ovale and the vestibule of the atrioventricular opening (Fig. 56.4A,B). The coronary sinus is often guarded by a thin, semicircular valve that covers the lower part of the orifice (Thebesius’ valve, also known as the Thebesian valve). The upper limb of this valve joins the Eustachian valve; a tendinous structure, the tendon of Todaro, runs from this commissure into the sinus septum, which is the septum between the coronary sinus and the fossa ovale. The tendon of Todaro runs forwards to insert into the central fibrous body and is one of the landmarks of the triangle of Koch (see below). The ostium of the coronary sinus forms a prominent landmark in the right atrium. The sinus itself lies within the left atrioventricular groove (Fig. 56.2B,D), and is the conduit for return of most of the venous blood from the heart, although some atrial veins drain directly to the right or left atrial chambers. The coronary sinus begins at the point where the oblique vein of the left atrium joins the great cardiac vein. The sinus receives the middle and small cardiac veins close to its junction with the right atrium.
The atrium proper and the auricle are separated from the venous sinus by the crista terminalis. This smooth, muscular ridge begins on the upper part of the septal surface and, passing anterior to the orifice of the superior vena cava, skirts its right margin to reach the right side of the orifice of the inferior vena cava. It marks the site of the right venous valve of the embryonic heart, and corresponds externally to the terminal groove. The sinu-atrial node is located within the superior part of the groove, lateral to and extending below the orifice of the superior vena cava (Fig. 56.4A,B).
Anteroinferior in the right atrium is the large, oval vestibule leading to the orifice of the tricuspid valve. A triangular zone, the triangle of Koch, is defined between the attachment of the septal cusp of the tricuspid valve, the anteromedial margin of the ostium of the coronary sinus, and the round, collagenous, palpable, subendocardial tendon of Todaro (Fig. 56.4A,B). The triangle is a landmark of particular surgical importance, indicating the site of the atrioventricular node and its atrial connections. Anterosuperior to the insertion of the tendon of Todaro, the septal wall is formed by the atrioventricular component of the membranous septum, intervening between the right atrium and subaortic outlet of the left ventricle (Fig. 56.5). The atrial wall bulges anterosuperiorly above the membranous septum. This area is the aortic mound (torus aorticus) and marks the location of the non-coronary sinus of the aorta with its enclosed valvular cusp.
Right ventricle
External features
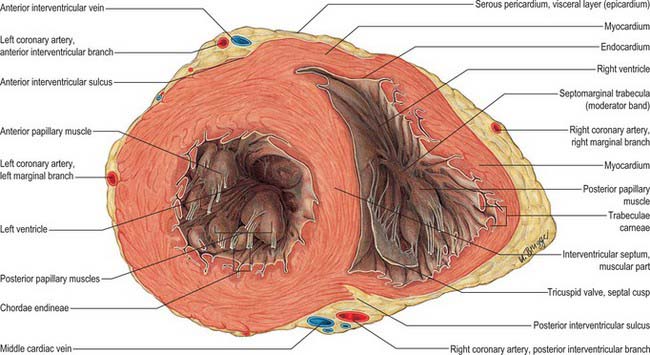
The convex anterosuperior surface of the right ventricle makes up a large part of the sternocostal aspect of the heart, and is separated from the thoracic wall only by the pericardium (Fig. 56.2A–D). The left pleura and, to a lesser extent, the anterior margin of the left lung are interposed above and to the left. The inferior surface is flat and is related mainly, with the interposition of the pericardium, to the central tendon and a small adjoining muscular part of the diaphragm. The left and posterior wall is the ventricular septum. This is slightly curved and bulges into the right ventricle so that, in sections across the cardiac axis, the outline of the right ventricle is crescentic. A delicate collagenous band, the tendon of the infundibulum (conus ligament), is believed by some to connect the pulmonary muscular infundibulum posteriorly to the root of the aorta. The wall of the right ventricle is significantly thinner (3–5 mm on average) than that of the left, the ratio of the thickness of the two walls usually being 1 : 3.
Internal features
The inlet and outlet components of the ventricle, supporting and surrounding the cusps of the tricuspid and pulmonary valves respectively, are separated in the roof of the ventricle by the prominent supraventricular crest (crista supraventricularis) (Fig. 56.4A). The crest is a thick, muscular, highly arched structure, extending obliquely forwards and to the right from a septal limb high on the interventricular septal wall to a mural or parietal limb on the anterolateral right ventricular wall. The posterolateral aspect of the crest provides a principal attachment for the anterosuperior cusp of the tricuspid valve. The septal limb of the crest may be continuous with, or embraced by, the septal limbs of the septomarginal trabecula. The inlet and outlet regions extend apically into and from the prominent coarsely trabeculated component of the ventricle. The inlet component is itself also trabeculated, whereas the outlet component (or infundibulum) has predominantly smooth walls. The trabeculated appearance is caused by a myriad of irregular muscular ridges and protrusions, which are known collectively as trabeculae carneae, and are lined by endocardium. These protrusions and intervening grooves impart great variation in wall thickness; the protrusions vary in extent from mere ridges to trabeculae, which are fixed at both ends but otherwise free. Other conspicuous protrusions are the papillary muscles, which are inserted at one end onto the ventricular wall and are continuous at the other end with collagenous cords, the chordae tendineae, inserted on the free edge and elsewhere on the free aspect of the atrioventricular valves. One protrusion in the right ventricle, the septomarginal trabecula or septal band, is particularly prominent. It reinforces the septal surface where, at the base, it divides into limbs that embrace the supraventricular crest. Towards the apex, it supports the anterior papillary muscle of the tricuspid valve and, from this point, crosses to the parietal wall of the ventricle as the ‘moderator band’ (this alternative name records an old idea that the septomarginal trabecula prevents overdistension of the ventricle). A further series of prominent trabeculae, the septoparietal trabeculations, extend from its anterior surface and run onto the parietal ventricular wall. The smooth-walled outflow tract, or infundibulum (conus arteriosus), ascends to the left above the septoparietal trabeculations and below the arch of the supraventricular crest to the pulmonary orifice.
Tricuspid valve
Tricuspid valvular orifice
The tricuspid valve orifice is best seen from the atrial aspect and measures on average 11.4 cm in circumference in males and 10.8 cm in females. It has a clear line of transition from the atrial wall or septum to the lines of attachment of the valvular cusps. Its margins are not precisely in a single plane. It is almost vertical, but at 45° to the sagittal plane and slightly inclined to the vertical, such that it ‘faces’ (on its ventricular aspect) anterolaterally to the left and somewhat inferiorly (Fig. 56.6). Roughly triangular, its margins are described as anterosuperior, inferior and septal, corresponding to the lines of attachment of the valvular cusps.
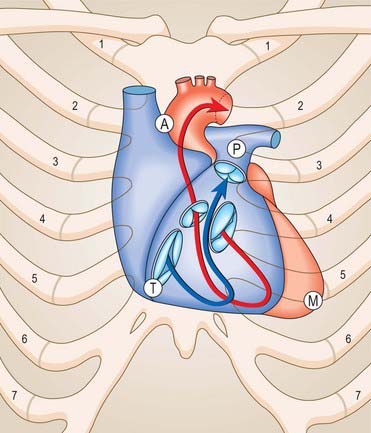
Fig. 56.6 Relation of the sternocostal surface and valves of the heart to the thoracic cage. The right heart is blue, the arrow denotes the inflow and outflow channels of the right ventricle; the left heart is treated similarly in red. The positions, planes and relative sizes of the cardiac valves are shown. The position of the letters A, P, T and M indicate respectively the aortic, pulmonary, tricuspid and mitral auscultation areas of clinical practice. Note that, for the purpose of illustration, the orifices of the aortic, mitral and tricuspid valves are shown with some separation between them. In reality, the cusps of the three valves are in fibrous continuity (see Fig. 56.10).
Tricuspid valve cusps
The anterosuperior cusp is the largest component of the tricuspid valve. It is attached chiefly to the atrioventricular junction on the posterolateral aspect of the supraventricular crest, but extends along its septal limb to the membranous septum, ending at the anteroseptal commissure. One or more notches often indent its free margin. The attachment of the septal cusp passes from the inferoseptal commissure on the posterior ventricular wall across the muscular septum and then angles across the membranous septum to the anteroseptal commissure. The septal cusp defines one of the borders of the triangle of Koch, thereby aiding location of the atrioventricular node, which lies at the apex of the triangle, and ensuring that this area can be avoided when operating on the tricuspid valve (Figs 56.4A,B; 56.5).
Chordae tendineae (tendinous cords)
The chordae tendineae are fibrous collagenous structures supporting the cusps of the atrioventricular valves. False chordae connect papillary muscles to each other or to the ventricular wall including the septum, or pass directly between points on the wall (or septum, or both); they are irregular in numbers and dimensions in the right ventricle. The true chordae usually arise from small projections on the tips or margins of the apical one-thirds of papillary muscles, but sometimes arise from the bases of papillary muscles or directly from the ventricular walls and the septum. They are attached to various parts of the ventricular aspects or the free margins of the cusps. They have been classified into first-, second- and third-order chordae according to the distance of the attachment from the margins of the cusps; this scheme has little functional or morphological merit.
Opening of the tricuspid valve
Despite its name, the tricuspid valve acts more like a bicuspid valve, because the septal cusp, the smallest of the three cusps, is fixed between the right and left fibrous trigones and the atrial and ventricular septa. The remainder of the tricuspid anulus is muscular. During diastole the right ventricle relaxes, the anulus dilates and the large anterior and posterior cusps move away from the plane of the anulus into the right ventricle. During systole the anulus constricts as the right ventricle contracts, and the two major cusps move like sails to abut a relatively immobile septal cusp and the septum itself (Fig. 56.7).
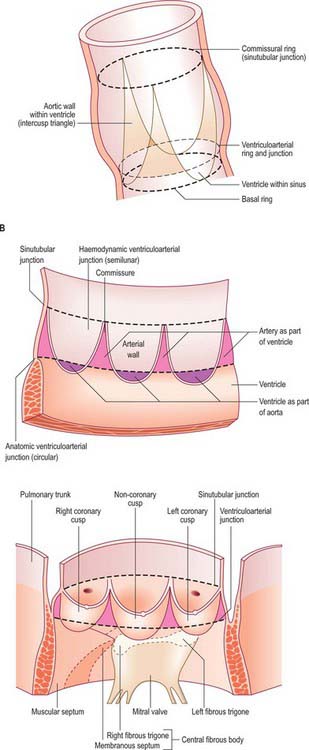
Pulmonary valve
The pulmonary valve, guarding the outflow from the right ventricle, surmounts the infundibulum and is situated at some distance from the other three cardiac valves (Figs 56.8, 56.9, 56.10). Its general plane faces superiorly to the left and slightly posteriorly. It has three semilunar cusps attached by convex edges partly to the infundibular wall of the right ventricle and partly to the origin of the pulmonary trunk. The line of attachments is curved, rising at the periphery of each cusp near their zones of apposition (the commissures) and reaching the sinutubular ridge of the pulmonary trunk (Fig. 56.11A–C). Removal of the cusps shows that the fibrous semilunar attachments enclose three crescents of infundibular musculature within the pulmonary sinuses, whereas three roughly triangular segments of arterial wall are incorporated within the ventricular outflow tract beneath the apex of each commissural attachment. There is, thus, no proper circular ‘anulus’ supporting the cusps of the valve, and the fibrous semilunar attachment is an essential requisite for snug closure of the nodules and lunules of the cusps (see below) during ventricular diastole. It is difficult to name the cusps and corresponding sinuses of the pulmonary valve and trunk precisely according to the coordinates of the body, because the valvular orifice is obliquely positioned. The official nomenclature (Terminologia Anatomica 1998) refers to an anterior, a posterior and a septal cusp, based on their position in the fetus. The position changes with development and in the adult there is one anterior semilunar cusp, and right and left semilunar cusps.
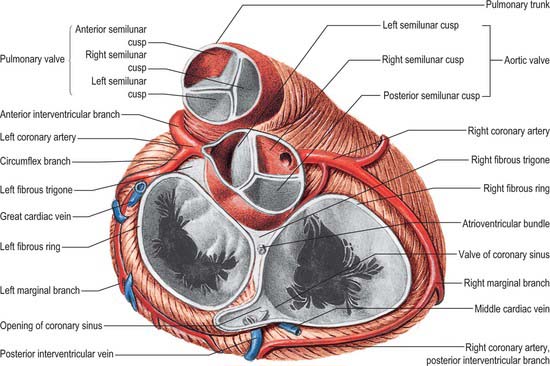
Fig. 56.9 The base of the ventricles, after removal of the atria and the pericardium. Coronary arteries and cardiac veins can be seen. Contrast the planes and positions of the aortic and pulmonary valves. Contrast with Fig. 56.10.
(From Sobotta 2006.)
Opening of the pulmonary valve
During diastole, the pulmonary valve is closed and all three cusps of the valve are tightly apposed. The pulmonary valve is difficult to visualize at echocardiography and usually only the posterior cusp is visible when the valve is closed; atrial systole may cause a slight posterior movement of the valve cusps. The pulmonary valve opens passively during ventricular systole and then closes rapidly at the end of systole (Fig. 56.7).
Left atrium
Although smaller in volume than the right, the left atrium has thicker walls (3 mm on average). Its cavity and walls are formed largely by the proximal parts of the pulmonary veins, which are incorporated into the atrium during development. The only clear derivative of the left part of the embryonic atrium is the auricle, together with the vestibule of the mitral valve. The left atrium is roughly cuboidal and extends behind the right atrium, separated from it by the obliquely positioned septum, thus the right atrium is in front and anterolateral to the right part of the left atrium. The left part is concealed anteriorly by the initial segments of the pulmonary trunk and aorta: part of the transverse pericardial sinus lies between it and these arterial trunks. Anteroinferiorly, and to the left, it adjoins the base of the left ventricle at the orifice of the mitral valve. Its posterior aspect forms most of the anatomical base of the heart and is approximately quadrangular, receiving the terminations of (usually) two pulmonary veins from each lung. It forms the anterior wall of the oblique pericardial sinus (Fig. 56.1). This surface ends at the shallow vertical interatrial groove, which descends to the cardiac crux. The left atrial auricle is constricted at its atrial junction and all the pectinate muscles of the left atrium are contained within it. It is characteristically longer, narrower and more hooked than the right auricle, its margins being more deeply indented. It turns forwards to the left of the pulmonary trunk, overlapping its origin (Fig. 56.8). Interiorly, the four pulmonary veins open into the upper posterolateral surfaces of the left atrium, two on each side. Their orifices are smooth and oval, the left pair frequently opening via a common channel. Some minimal cardiac veins return blood directly from the myocardium to the cavity of the left atrium. The left atrial aspect of the septum has a characteristically rough appearance, bounded by a crescentic ridge, concave upwards, which marks the site of the foramen ovale.
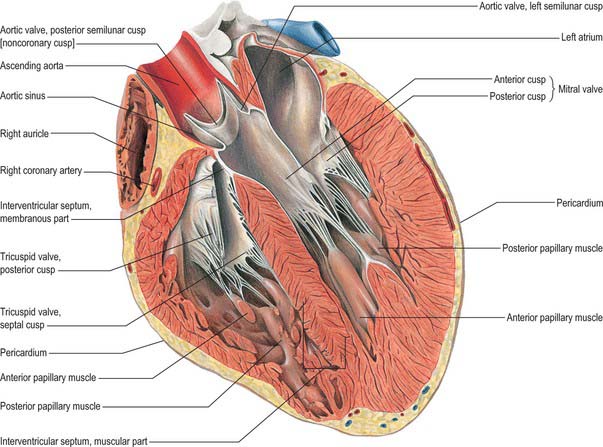
Left ventricle
General and external features
The left ventricle is constructed in accordance with its role as a powerful pump that sustains pulsatile flow in the high-pressured systemic arteries. Variously described as half-ellipsoid or cone-shaped, it is longer and narrower than the right ventricle, extending from its base in the plane of the atrioventricular groove to the cardiac apex. Its long axis descends forwards and to the left. In transverse section, at right angles to the axis, its cavity is oval or nearly circular, with walls about three times thicker (8–12 mm) than those of the right ventricle (Fig. 56.12). It forms part of the sternocostal, left and inferior (diaphragmatic) cardiac surfaces. Except where obscured by the aorta and pulmonary trunk, the base of the ventricular cone is superficially separated from the left atrium and atrial auricle by part of the atrioventricular groove; the coronary sinus runs in the posterior aspect of the groove to reach the right atrium (Fig. 56.2B,D). The anterior and posterior interventricular grooves indicate the lines of mural attachment of the ventricular septum and the limits of the left and right ventricular territories. The sternocostal surface of the ventricle curves bluntly into its left surface at the obtuse margin.
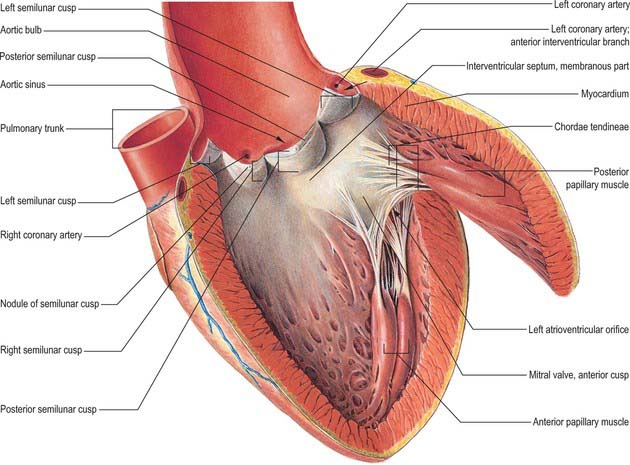
Internal features
The left ventricle has an inlet region, guarded by the mitral valve (ostium venosum), an outlet region, guarded by the aortic valve (ostium arteriosum), and an apical trabecular component. The left atrioventricular orifice admits atrial blood during diastole, flow being towards the cardiac apex. After closure of the mitral cusps, and throughout the ejection phase of systole, blood is expelled from the apex through the aortic orifice. In contrast to the orifices within the right ventricle, those of the left ventricle are in close contact, with fibrous continuity between the cusps of the aortic and mitral valves (the subaortic curtain; Fig. 56.13). The inlet and outlet turn sharply round this fibrous curtain (Fig. 56.9).
The anterolateral wall is the concavo-convex ventricular septum, a muscular wall the convexity of which is the posteromedial profile of the right ventricle as seen in section. It thus completes the circular outline of the left ventricle (Fig. 56.12). Towards the aortic orifice, the septum becomes the thin, collagenous interventricular component of the membranous septum, an oval or round area below and confluent with the fibrous triangle separating the right and the non-coronary cusps of the aortic valve.
Between the lower limits of the free margins of the cusps of the mitral valve and the apex of the ventricle, the muscular walls are deeply trabeculated. These trabeculae carneae are finer and more intricate than those of the right ventricle, but similar in structure. Trabeculation is characteristically well developed near the apex, whereas the upper reaches of the septal surface are smooth (Fig. 56.13).
Hypertrophy of heart muscle
In hypertrophic cardiomyopathy, there is an increase in the thickening of the myocardial walls, particularly the interventricular septum, which is disproportionately thickened in comparison with the posterior wall. Echocardiography allows accurate assessment of the thickening and of systolic function. Other features in hypertrophic cardiomyopathy are dynamic left ventricular outflow obstruction, systolic anterior motion of the anterior mitral valve cusp, and midsystolic closure of the aortic valve. A degree of diastolic dysfunction is also present in some cases of hypertrophic cardiomyopathy. Serial short-axis magnetic resonance imaging (MRI) allows accurate measurement of wall thickness and is particularly useful in assessing hypertrophy confined to the apex. Gradient-echo MRI also allows some functional assessment of the hypertrophy. A number of histological changes are observed, including disarray of the cardiac myocytes with replacement fibrosis, and expansion of the collagen component. Treatment is usually medical, except for refractory cases and those in whom the left ventricular outflow tract obstruction has a gradient of greater than 50 mmHg. Ventricular septal myotomy and myectomy are performed in such cases. More recently, catheter alcohol septal ablation has been introduced as a non-surgical alternative. A number of patients may also require implantation of cardiac defibrillators to prevent sudden cardiac death.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree