Healthcare-Associated Infections and the Environment
Andrew J. Streifel
ENVIRONMENTAL RESERVOIRS AND THE EPIDEMIOLOGIC CHAIN
The relationship between the physical environment of healthcare facilities and infection control has long been debated. Continuing advances in medical technology and pharmacology have given physicians many options, unrelated to the physical environment, for preventing healthcare-associated infections. Restrictive and time-consuming barriers and procedures such as laminar-flow rooms with attendant aseptic technique have generally been in disfavor relative to the pharmacologic approach to preserving immune competence. At the same time, passive environmental controls such as filtration and pressurization systems to provide spore-free environments continue to be used in increasingly sophisticated ways. Legitimate questions remain as to the extent to which environmental reservoirs contribute to healthcareassociated infections. An argument can legitimately be made that cleanliness needs no further epidemiologic justification and that all hospitalized patients are entitled to a clean and odor-free environment. However, legitimate questions can also be raised as to allocation of resources to environmental controls that have no epidemiologic basis. An example is the extent to which chemical germicides should be used on environmental surfaces as opposed to nongermicidal cleaning methods that appear to yield equivalent microbiologic reductions (1). With such issues, new technology is adapting to the means of real-time sampling using indicators such as environmental adenosine triphosphate (ATP) (2) for determining cleanliness.
One reason for continued disagreement over the importance of environmental reservoirs is failure to consider historical perspective and thus the starting point for measuring significance. People have rightly come to expect a high level of sanitation in medical facilities, a level that has already achieved a major reduction in infection incidence, and are now dealing with a very different set of infection determinants focusing largely on patient susceptibility factors. The writings of Florence Nightingale based on her experiences in the Crimean War in the 1850s reveal the striking contrasts between conditions then and now (3). She devoted whole chapters to pure air, pure water, efficient drainage, cleanliness, and light, which she considered the cornerstones of good health and prevention of mortality. In her detailed journals, she documented survival data in the hospital where she cared for British soldiers of the Crimean War. She documented dramatic changes in mortality from February 1855 (420/1,000) to September 1855 (22/1,000), which she attributed to “nursing care and sanitary measures” (4). Her changes included such basics as scrub brushes, laundry tubs, and clean dressings for wounds, all replacing abominably filthy conditions associated with the pest houses of the time. Thus, the question that should be addressed today is not whether the environment is important—it obviously is—but how best to use available infection control practices most cost effectively to protect patients and healthcare workers from infectious hazards. In this chapter, a variety of environmental reservoirs are reviewed relative to evidence linking these reservoirs to disease and a distinction is made between proven linkage to disease and simple evidence of lower contamination levels (which may or may not be worthwhile, regardless of disease linkage). In this chapter, two developments are emphasized, which are considered the most significant in this ongoing attempt to define the role of the physical environment in healthcare-associated infections. First, as antibiotic resistance problems mount and higher percentages of infections become more difficult to treat, one has little choice but to fall back on environmental cleanliness as a cornerstone preventive component of infection control. The second development is the continuing refinement of DNA fingerprinting technology, which more and more enables identification of specific sources of infection and determines the relatedness of infection clusters. A number of examples are cited and predictions are made that this technology will eventually shed further light on the importance of environmental controls.
LITERATURE REVIEW
Association of Reservoirs with Healthcare-Associated Infections
Although the literature is replete with accounts of microbial contamination in a great variety of hospital settings, most of these articles describe contamination levels, not infection levels, and prescriptions for reducing these contamination levels do not necessarily translate into
reduced incidence of healthcare-associated infection. Even when specific correlation to infection rates is suggested, the evidence is often tenuous, and direct association to an environmental source is difficult to prove. One area where investigators seem to be convinced that environmental sources contribute to infection is that of Aspergillus infections in severely immunocompromised patients. Humphries et al. (5) attributed two invasive Aspergillus infections in an intensive therapy unit to spores accumulating in fibrous insulation material above a perforated metal ceiling. Arnow et al. (6) similarly attributed an increase in Aspergillosis incidence to growth of microorganisms on filters and claimed that improved environmental maintenance and filter replacement were associated with a fourfold reduction in aspergillosis incidence over a 2-year period. Table 71-1 lists environmental sources of fungi in the hospital (6,7,8, 9, 10, 11, 12 and 13,14,15, 16, 17, 18 and 19).
reduced incidence of healthcare-associated infection. Even when specific correlation to infection rates is suggested, the evidence is often tenuous, and direct association to an environmental source is difficult to prove. One area where investigators seem to be convinced that environmental sources contribute to infection is that of Aspergillus infections in severely immunocompromised patients. Humphries et al. (5) attributed two invasive Aspergillus infections in an intensive therapy unit to spores accumulating in fibrous insulation material above a perforated metal ceiling. Arnow et al. (6) similarly attributed an increase in Aspergillosis incidence to growth of microorganisms on filters and claimed that improved environmental maintenance and filter replacement were associated with a fourfold reduction in aspergillosis incidence over a 2-year period. Table 71-1 lists environmental sources of fungi in the hospital (6,7,8, 9, 10, 11, 12 and 13,14,15, 16, 17, 18 and 19).
Air
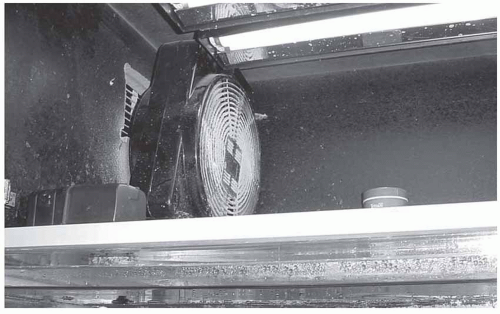
The controversy over the role of airborne microbes as a source of surgical site infections has gone on for many decades. In theory, a surgical site exposing sterile tissue is susceptible to invading microorganisms from many sources. Certainly, rigid aseptic techniques and the need to sterilize any item entering a surgical site has long been accepted practice. Similarly, the need for filtration and high dilution rates of operating room air has also been accepted. However, proof of airborne infection of surgical sites has been hard to come by, and demonstrated effectiveness of specific controls as a means of reducing infection incidence has similarly been hard to prove. Walter et al. (20) claimed to have demonstrated a specific airborne surgical infection, and Hart (21) published the results of a 29-year study claiming the significant benefits of ultraviolet installations for limiting surgical site infection. Other investigators, however, have failed to confirm these conclusions. In particular, Ayliffe and Beard (22) and Howe and Marston (23), while confirming that good filtration and dilution could reduce airborne contamination levels, could find no association of such reductions with infection prevention. In a general review of indoor microbial aerosols, Spendlove and Fannin (24) made the point that little is known about the true significance of these aerosols relative to human health and that continued research is needed. The sources of mold are many in the biologic world and the indoor environment can be controlled when emphasis is placed on filtration, air exchanges, and pressure management (25). It becomes imperative to control sources close to the patients at risk from opportunistic microbes such as Aspergillus fumigatus (see also Chapter 41). Such practice of source management also works for industrial hazards. These settings, however, provide easier identification for source management.
TABLE 71-1 Environmental Fungal Sources in Hospitals | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Water Reservoirs
The literature is replete with reports of improperly disinfected medical devices that are implicated in healthcare-associated infections, particularly devices such as respiratory therapy equipment that are associated with water reservoirs of one kind or another (26) or devices that have hard-to-clean channels such as fiberoptic endoscopes (27). Similarly, a number of environmental water reservoirs have quite clearly been associated with infection involving aerosolization from these sources. Examples include faucet aerators associated with Pseudomonas infections (28) and shower heads associated with legionellosis (29,30) (see also Chapter 36). Weber et al. (31) recently confirmed by pulsed-field gel electrophoresis that faucet aerators were contaminated with identical strains of Stenotrophomonas maltophilia found to colonize a cluster of patients in a surgical intensive care unit. They attributed the problem to low-level contamination of potable water subsequently amplified in the faucet aerators. Jonas et al. (32) used three methods of DNA typing to compare environmental and patient isolates of Legionella pneumophila. Although all three methods detected one prominent genotype, amplified fragment length polymorphism had better interassay reproducibility and concordance than either macrorestriction analysis (MRA) or arbitrarily primed polymerase chain reaction (AP-PCR). MRA was also cited as an important tool for epidemiologic investigation of healthcare-associated
infections by Luck et al. (33) who used that technique to match Legionella isolates from four patients with identical strains isolated from the hot water supply of the hospital. Legionellosis is a disease, important in the lexicon of healthcare-associated infections, for which an environmental reservoir has clearly been identified (warm water reservoirs in buildings) and for which specific preventive environmental protocols are recommended and generally accepted. Edelstein (34) reviewed some of these recommendations. They include hyperchlorination (6-20 mg/L) followed by long-term continuous chlorination at 1 to 2 mg/L or intermittent elevation of water temperature to 60°C to 70°C with or without chlorination. An additional example of aerosolization from a water reservoir was reported by Grieble et al. (35). They associated a rise in gram-negative septicemias with aerosolization from a waste hydropulping system that had been installed in a new Veterans Administration hospital. They also suggested that closing down the system halted the outbreak.
infections by Luck et al. (33) who used that technique to match Legionella isolates from four patients with identical strains isolated from the hot water supply of the hospital. Legionellosis is a disease, important in the lexicon of healthcare-associated infections, for which an environmental reservoir has clearly been identified (warm water reservoirs in buildings) and for which specific preventive environmental protocols are recommended and generally accepted. Edelstein (34) reviewed some of these recommendations. They include hyperchlorination (6-20 mg/L) followed by long-term continuous chlorination at 1 to 2 mg/L or intermittent elevation of water temperature to 60°C to 70°C with or without chlorination. An additional example of aerosolization from a water reservoir was reported by Grieble et al. (35). They associated a rise in gram-negative septicemias with aerosolization from a waste hydropulping system that had been installed in a new Veterans Administration hospital. They also suggested that closing down the system halted the outbreak.
Hydrotherapy pools and tanks are another water reservoir wherein the combination of organic debris from infected patients and elevated water temperature clearly supports growth of microorganisms; not surprisingly, several investigators have associated these tanks with infections. Examples include McGuckin et al. (36) reporting on an outbreak of Pseudomonas aeruginosa wound infection and Mayhall et al. (37) describing a bacteremia outbreak of Enterobacter cloacae. Rutala and Weber (38) reviewed the subject of water reservoirs of healthcare-associated pathogens. They listed more than a dozen such reservoirs identified in hospitals, including potable water, sinks, faucet aerators, showers, ice and ice machines, eyewash stations, dental-unit water systems, dialysis water, water baths, ice baths, tub immersion, toilets, and flower vases. All these sources have been specifically shown to harbor healthcare-associated pathogens, and regardless of the uncertain epidemiologic significance of such reservoirs, prudent control measures are available to limit microbial growth and such measures should be used. The authors also pointed out the growing importance of molecular epidemiology for typing pathogens in these reservoirs. DNA fingerprinting by pulsed-field gel electrophoresis is an example of a technique that can be used to match clinical and environmental strains. That technique was used by Buttery et al. (39) to link a P. aeruginosa outbreak to water-retaining bath toys in a toy box. Finally, Verweij et al. (40) used random arbitrary polymorphic DNA PCR analysis to link an infant death from S. maltophilia infection to contaminated tap water. They concluded that preterm infants should not be washed using tap water. Water has been implicated as a potential reservoir for filamentous fungi (41,42), and it is logical that spores could become entrapped in water and distributed to susceptible patients. This contamination was not associated with growth in water, but at the interface of water and air (43). Although eliminating all of these microbes seems easy to do with high-efficiency particulate air (HEPA)-quality filters, it would seem more effective to provide sterile water for drinking. The potential pathogenic sources in municipal water include soil, expansion tanks, evaporative pans, or accumulated biofilm within the water distribution system. Water usage is decreasing in healthcare facilities due to sustainable and green building concepts. Use of air-cooled med gas machines, digital radiology processors, and waterless hand cleaning is remarkably reducing water consumption. For example, at the University of Minnesota Medical Center, since 1990 the water usage volume has dropped from 164,000 to 82,000 g/day. This drop in water usage promotes stagnation, which increases bacteria levels in water. Incidents investigated by this author regarding resistant gram-negative bacteria confirm transmission from sink to patient with respiratory therapy equipment and feeding tubes. Inappropriate use of tap water is often the cause of such transmissions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree