Overview
Overview
Headaches generally are classified as primary or secondary. Primary headaches, which account for the majority (approximately 90%) of headaches, are not associated with an underlying illness. Examples include episodic and chronic tension-type headaches, migraine headache with and without aura, cluster headaches, and medication-overuse headaches. Secondary headaches are symptoms of an underlying condition such as head trauma, stroke, substance abuse or withdrawal, bacterial and viral diseases, and disorders of craniofacial structures.
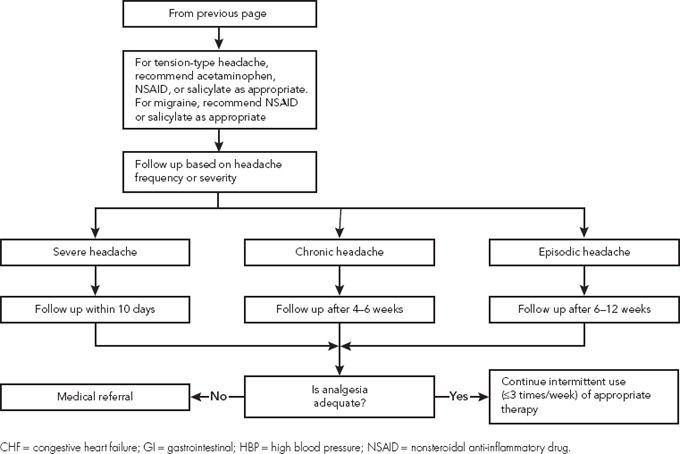
Tension-type headaches (i.e., stress headaches) and sinus headaches usually are amenable to self-treatment. A medical diagnosis of migraine headache is necessary before self-treatment can be recommended.
Medication-overuse headaches usually are associated with frequent (more than twice weekly) use of analgesics for ≥3 months. They occur within hours of stopping the agent; re-administration provides relief. Patients may have a nearly continuous headache that is particularly noticeable on awakening. When medication-overuse headache is suspected, use of the offending agent(s) should be tapered and eventually eliminated. This preferably should be done with medical supervision because prescription medications may be needed to combat the increased headaches that occur during the days to weeks of the withdrawal period.
 Epidemiology
Epidemiology
- More than 75% of the U.S. population will experience tension-type headaches at some time, with a 1-year prevalence of 38%.
- The prevalence of migraine headache in the United States is about 18% for women and 6% for men. Onset usually begins in the first three decades of life, with the greatest prevalence around 40 years of age. Menstrual migraines, which appear at the menstrual stage of the ovarian cycle, occur in <10% of women.
- Although headache is a frequently reported symptom in patients with acute sinusitis, the actual frequency of occurrence of sinus headache is quite low. As many as 90% of patients who complain of sinus headache may actually be experiencing migraine headache.
 Etiology
Etiology
- Tension-type headaches usually occur in response to stress, anxiety, depression, emotional conflicts, and other stimuli.
- Episodic tension-type headache is thought to have a peripheral pain source.
- Tension-type headache is considered to be chronic if it occurs at least 15 days per month for at least 6 months. Chronic tension-type headache is believed to have a central mechanism.
- Episodic tension-type headache is thought to have a peripheral pain source.
- Migraine headaches are believed to arise from a complex interaction of neuronal and vascular factors, most likely involving dysfunction of the trigeminovascular system. They can be triggered by a wide variety of stimuli, including a number of medications.
- It is likely that tension-type and migraine headache share pathophysiologic features, making them more similar than distinct.
- Sinus headache occurs when infection or blockage of the paranasal sinuses causes inflammation or distension of the sensitive sinus walls.
 Signs and Symptoms
Signs and Symptoms
- Headaches can be differentiated by the signs and symptoms shown in Table 1.
- It is possible for patients to have coexisting tension and migraine headaches. Treatment of the initiating headache type can abort the mixed headache problem.
- It can be difficult to differentiate sinus headache from migraine without aura. One notable difference is that sinus headache is not accompanied by nausea, vomiting, or visual disturbances.
- Persistent sinus pain, discharge, or both suggest possible infection and require referral for medical evaluation.
TABLE 1. Characteristics of Tension-Type, Migraine, and Sinus Headaches
Characteristic | Tension-Type Headache | Migraine Headache | Sinus Headache |
Location | Bilateral Over the top of the head, extending to the base of the skull | Usually unilateral | Face, forehead, or periorbital area |
Nature | Varies from diffuse ache to tight, pressing, constricting pain | Throbbing pain | Pressure behind eyes or face |
Onset | Gradual | Sudden | Simultaneous with sinus symptoms, including purulent nasal discharge |
Duration | Minutes to days | Hours to 2 days | Days (resolves with sinus symptoms) |
a Aura usually consists of shimmering or flashing areas or blind spots in the visual field, difficulty speaking, visual and auditory hallucinations, and (usually) one-sided muscle weakness.
 Treatment
Treatment
- Most patients with episodic headaches respond adequately to self-treatment with nonpharmacologic interventions and/or nonprescription analgesics.
- Some patients with episodic headaches and most with chronic headaches are candidates for prescription treatments.
 General/Nonpharmacologic Treatment Measures
General/Nonpharmacologic Treatment Measures
- Patients with chronic tension-type headaches often benefit from relaxation exercises and physical therapy that emphasizes stretching and strengthening of head and neck muscles.
- General treatment measures for migraine headaches include:
- Maintaining a regular sleeping and eating schedule.
- Practicing stress reduction techniques.
- Using ice (ice bags or cold packs) combined with pressure applied to the forehead or temple areas to reduce pain associated with acute attacks.
- Maintaining a regular sleeping and eating schedule.
- Patients with migraine headaches should be encouraged to minimize or avoid exposure to their known triggers.
 Pharmacologic Therapy
Pharmacologic Therapy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree