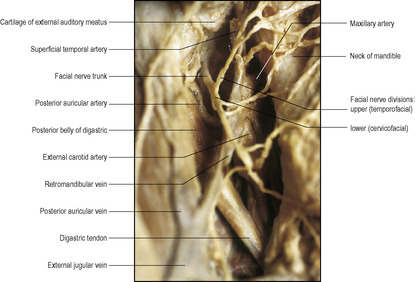
Between the angle of the mandible and the tip of the mastoid process the investing layer is strong and splits to enclose the parotid gland. The superficial part extends superiorly as the parotidomasseteric fascia and reaches up to the zygomatic arch. The deep part extends to the base of the skull; between the styloid process and the angle of the mandible it is thickened as the stylomandibular ligament.
Below, the investing layer is attached to the spine and acromion of the scapula and the clavicle with the trapezius, and to the clavicle and the manubrium of the sternum with the sternocleidomastoid. In the intervals between these muscles, it is attached to both clavicles and to the jugular (suprasternal) notch by two layers into which it splits a short distance above them. The layers are attached to the anterior and posterior borders of the jugular notch, enclosing between them the suprasternal space which contains the lower parts of the anterior jugular veins, an anastomotic arch between them, the sternal heads of the sternocleidomastoids and sometimes a lymph node. Of the two layers that adhere to the middle third of the clavicle, the deeper splits around the inferior belly of the omohyoid, forming a fascial sling which keeps this muscle belly low down in the neck (see Fig. 2.2, p. 39). The two layers are pierced by the external jugular vein.
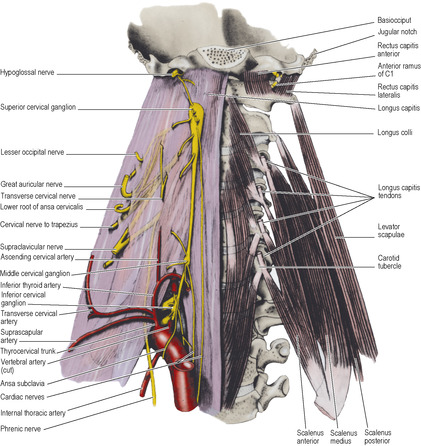
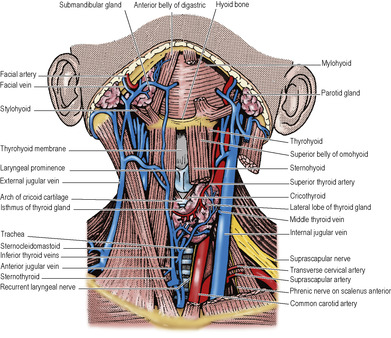
Prevertebral fascia
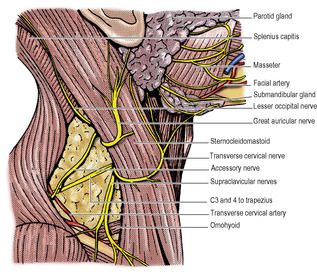
This is a firm, tough membrane that lies in front of the prevertebral muscles (Fig. 6.1). It extends from the base of the skull, in front of the longus capitis, rectus capitis lateralis and longus colli muscles, downwards to blend with the anterior longitudinal ligament on the body of T4 vertebra. It extends sideways across the scalenus anterior, scalenus medius and levator scapulae muscles (Fig. 6.8), getting thinner further out and fading under cover of the anterior border of trapezius. It covers the muscles that form the floor of the posterior triangle of the neck and all the cervical nerve roots (thus the cervical plexus and trunks of the brachial plexus lie deep to it). The lymph nodes of the posterior triangle and the accessory nerve lie superficial to it. The third part of the subclavian artery lies deep to the fascia, which becomes prolonged over the artery and the brachial plexus below the clavicle as the axillary sheath to a varying extent in the axilla. It does not invest the subclavian or axillary vein; these lie in loose areolar tissue anterior to it, free to dilate during times of increased venous return from the upper limb. The fasica is pierced by the four cutaneous branches of the cervical plexus (great auricular, lesser occipital, transverse cervical and supraclavicular nerves).
Pretracheal fascia
This thin fascia lies deep to the infrahyoid strap muscles (sternothyroid, sternohyoid and omohyoid) so that its upward attachment is limited by the respective attachments of those muscles, namely, the body of the hyoid bone and the oblique line of the thyroid cartilage. It splits to enclose the thyroid gland, to which it is not adherent except to the back of the isthmus where it is also attached to the second, third and fourth rings of the trachea. Laterally, it fuses with the front of the carotid sheath on the deep surface of the sternocleidomastoid and inferiorly it passes behind the brachiocephalic veins to blend with the adventitia of the arch of the aorta and the fibrous pericardium. The pretracheal fascia is also described in some accounts as being part of a cervical visceral fascia that surrounds the pharynx, oesophagus, larynx and trachea.
Carotid sheath
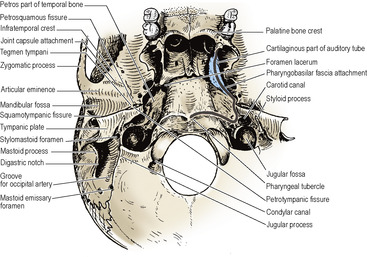
This is not a fascia in the sense of a demonstrable membranous layer, but consists of a feltwork of areolar tissue that surrounds the common and internal carotid arteries, internal jugular vein, vagus nerve and some deep cervical lymph nodes (Fig. 6.1). It is thin where it overlies the internal jugular vein, allowing the vein to dilate during increased blood flow. The sheath is attached to the base of the skull at the margins of the carotid canal and jugular fossa, and is continued downwards along the vessels to blend with the adventitia of the aortic arch. In front the lower part of the sheath fuses with the fascia on the deep surface of the sternocleidomastoid. Where they lie alongside, the sheath blends with the pretracheal fascia. Behind the carotid sheath there is a minimum of loose areolar tissue between it and the prevertebral fascia; the cervical sympathetic trunk lies here in front of the prevertebral fascia (Fig. 6.8). The carotid sheath is described further on page 366.
Tissue spaces of the neck
Behind the prevertebral fascia is the closed prevertebral space from which an anterior escape can only be made by a perforation in the fascia. Hence pus from an abscess in a cervical vertebra can lift the prevertebral fascia as far down as the superior mediastinum.
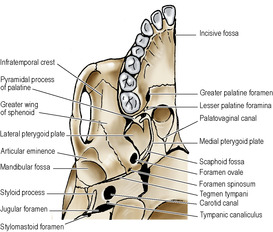
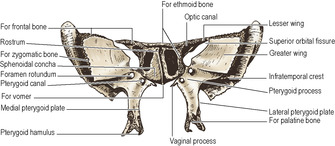
Immediately in front of the prevertebral fascia is a space that extends from the base of the skull to the diaphragm passing through the superior into the posterior mediastinum as it does so (see Fig. 4.9, p. 189). Its upper part is the retropharyngeal space, which is continuous laterally with a parapharyngeal space at the side of the pharynx; the upper part of this space is in the infratemporal fossa (see p. 361), bounded laterally by the pterygoid muscles and the parotid sheath.
In the upper part of the neck is the submandibular space below the mylohyoid muscle and deep to the investing layer of fascia between the hyoid bone and the mandible. This space communicates around the posterior border of mylohyoid with a sublingual space under the mucous membrane of the floor of the mouth. Ludwig’s angina is a rare but severe form of cellulitis that involves these spaces and spreads backwards into the parapharyngeal space.
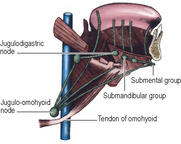
Three or four small submental lymph nodes lie beneath the chin, some superficial and others deep to the investing layer of deep cervical fascia (Fig. 6.6). They drain, across the midline, a wedge of tissue in the floor of the mouth opposite the four lower incisor teeth, including those teeth, gums and lip, and the tip of the tongue (Fig. 6.34). In their turn they drain to submandibular nodes or directly to the upper deep cervical group.
About half a dozen submandibular lymph nodes lie on the surface of the submandibular gland, some embedded within the gland (Fig. 6.6). They drain the submental nodes, the lateral parts of the lower lips, all the upper lip and external nose, and the anterior part of the tongue, mainly but not exclusively from their own side. They also receive lymph from the anterior half of the nasal walls and the paranasal sinuses that drain there (frontal, anterior and middle ethmoidal, and maxillary), and from all the teeth (except lower incisors).
Part two. Triangles of the neck
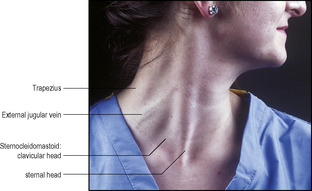
To assist the description of the topographical anatomy of the neck and the location of pathological lesions, each side is divided into anterior and posterior triangles by the obliquely placed sternocleidomastoid muscle (Fig. 6.2). The posterior triangle lies between the posterior border of sternocleidomastoid, the anterior border of trapezius and the clavicle, and the anterior triangle between the anterior border of sternocleidomastoid, the lower border of the mandible and the midline. The anterior triangle can be subdivided into submental, digastric, carotid and muscular triangles (see p. 344).
Sternocleidomastoid
This prominent neck landmark has two heads of origin below: that from the sternal manubrium is a rounded tendon, that from the clavicle a flat, fleshy mass (Fig. 6.2). A triangular interval exists between the two above the sternoclavicular joint, and the lower end of the internal jugular vein lies here, where it can be entered by needle or catheter. The manubrial tendon is attached to the front of the bone below the jugular notch; the clavicular head arises from the superior surface of the medial third of the clavicle. The muscle is attached by a tendon to the lateral surface of the mastoid process and by a thin aponeurosis to the lateral half of the superior nuchal line of the occipital bone. The clavicular fibres spiral behind the sternal fibres with the deep aspect of which they blend. The clavicular fibres are directed mainly to the mastoid process, while the sternal fibres run more obliquely chiefly to the occipital bone. The spinal accessory nerve enters the muscle under cover of the lobule of the ear, about 3cm below the tip of the mastoid process, accompanied by a branch to the muscle from the occipital artery. It runs through the deep part of the muscle to emerge from between a third and a half of the way down the posterior border of the muscle.
Sternocleidomastoid is enclosed within a sheath of the investing layer of deep cervical fascia, which splits to surround it (Fig. 6.1). The muscle is crossed superficially by the great auricular nerve, the external jugular vein and the transverse cervical nerve, in that order from above downwards. Deep to the upper half of the muscle lies the cervical plexus; deep to its lower part lies the carotid sheath and its contents, overlying scalenus anterior.
The blood supply of the muscle is from branches of the occipital and superior thyroid arteries.
Nerve supply. By the spinal part of the accessory nerve, from a branch which leaves the nerve proximal to its point of entry into the muscle. The pathway for innervation by the cerebral cortex of the anterior horn cells of the segments concerned (mostly C2 and 3) is disputed; projection to the muscle from either or both hemispheres has been described. Branches from the cervical plexus (C2, 3) carrying proprioceptive fibres enter the muscle directly or by joining the accessory nerve.
Action. Contraction of one muscle tilts the head towards the ipsilateral shoulder, and rotates the head and face to the opposite side. Both muscles acting together from below draw the head forwards. With the head fixed, the muscles can assist in raising the roof of the thorax in forced inspiration.
Test. The face is turned to the opposite side against resistance and the muscle palpated.
Posterior triangle
This is an area enclosed between the sternocleidomastoid and trapezius muscles. Its apex lies high up at the back of the skull on the superior nuchal line, where there is a small gap between the attachments of the two muscles. Its base is the middle third of the clavicle at the side of the root of the neck. Its roof is formed by the investing layer of deep cervical fascia. Its floor consists of the prevertebral fascia lying on, from above downwards, splenius, levator scapulae and scalenus medius. Depending on the size of the sternocleidomastoid and the degree of depression of the shoulder, scalenus anterior and the first digitation of serratus anterior may contribute to the floor, and at the apex of the triangle, splenius may be low enough to expose a little of semispinalis capitis.
Although the subclavian artery, the three trunks of the brachial plexus and branches of the cervical plexus are deep to the prevertebral fascia, they are listed as contents of the posterior triangle; in operations on the triangle all these structures are safe provided the prevertebral fascia is left intact. The pulsation of the subclavian artery can be felt by pressing downwards behind the clavicle at the posterior border of sternocleidomastoid.
The cutaneous branches of the cervical plexus pierce the investing fascia at the posterior border of sternocleidomastoid. The cervical branches to trapezius pass across the floor of the triangle deep to the prevertebral fascia.
Lying between the roof and floor are the lymph nodes of the posterior triangle. Two or three occipital nodes lie in the subcutaneous tissue at the apex and several supraclavicular nodes lie above the clavicle; the latter are really outlying members of the lower group of deep cervical nodes (see p. 410).
The accessory nerve emerges from sternocleidomastoid, about a third of the way or a little lower down its posterior border. It passes downwards and backwards, with a characteristic wavy course adherent to the inner surface of the fascia of the roof of the triangle, to disappear beneath the anterior border of trapezius, about a third of the way from its lower end and 3–5cm above the clavicle. These points of reference to the borders of sternocleidomastoid and trapezius enable the surface marking of the accessory nerve in the posterior triangle, where it is particularly liable to injury in operations involving the removal of lymph nodes, one or two of which may lie in contact with the nerve. More proximally, the nerve lies in front of the transverse process of the atlas (palpable between the mastoid process and mandibular ramus) and it enters the substance of sternocleidomastoid between the upper two quarters of the muscle.
The inferior belly of omohyoid crosses the lower medial part of the triangle and is kept in place by its sling of investing fascia. Deep to the omohyoid are the transverse cervical and suprascapular vessels, just above the clavicle. The external jugular vein pierces both split layers of the lower part of investing fascia to enter the posterior triangle on its way to the subclavian vein, which itself is too low to be a content of the triangle; the wall of the vein is adherent to the fascia as it passes through.
Cervical plexus
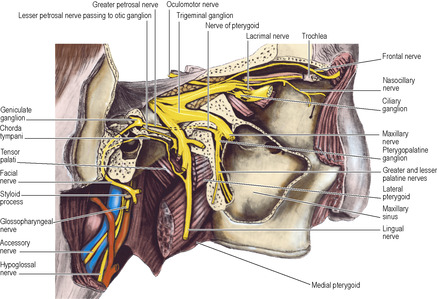
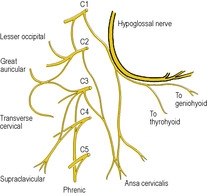
The cervical plexus (Fig. 6.3) is formed by loops between the anterior rami of the upper four cervical nerves, after each has received a grey ramus communicans from the superior cervical ganglion. It lies in series with the brachial plexus, on the scalenus medius, behind the prevertebral fascia. It is covered by the upper part of sternocleidomastoid, and does not lie in the posterior triangle. The upper three cervical nerves have meningeal branches for the posterior cranial fossa. C1 fibres ascend with the hypoglossal nerve, C1 and 2 fibres ascend with the vagus nerve and C2 and 3 fibres ascend through the foramen magnum.
 |
| Figure 6.3 |
Muscular branches. Muscular branches are given off segmentally to the prevertebral muscles (longus capitis, longus colli and the scalenes). Other muscular branches are:
• A branch from C1 to the hypoglossal nerve, by which the fibres are carried to the superior root of the ansa cervicalis and the nerves to thyrohyoid and geniohyoid.
• Branches from C2 and 3 to sternocleidomastoid, and from C3 and 4 to trapezius. These fibres are mainly proprioceptive, but occasionally the whole of trapezius is not paralysed when the accessory nerve is damaged, as some of the cervical fibres may be motor.
• The inferior root of the ansa cervicalis is formed by union of a branch each from C2 and C3. The nerve spirals around the lateral side of the internal jugular vein and descends to join the superior root (C1) at the ansa (see p. 344).
• The phrenic nerve is formed mainly from C4 with contributions from C3 and C5 and runs down vertically over the obliquity of the scalenus anterior muscle, passing from lateral to medial borders, beneath the prevertebral fascia, lateral to the ascending cervical branch of the inferior thyroid artery. It passes behind the subclavian vein into the mediastinum (see p. 195). It may be joined below the vein by a branch (the accessory phrenic nerve) from the nerve to subclavius; this branch may descend in front of the subclavian vein. The phrenic nerve is one of the most important in the body, being the sole motor supply to its own half of the diaphragm (see p. 187), and it also has an extensive afferent distribution, not only to the diaphragm but to the pericardium, pleura and peritoneum (see pp. 197, 212 and 238).
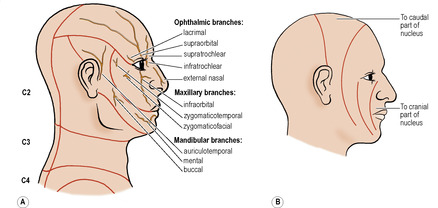
Cutaneous branches. Cutaneous branches of the plexus (Fig. 6.4) supply the front and sides of the neck and contribute to the supply of the scalp, face and chest.
The lesser occipital nerve (C2) is a slender branch that hooks around the accessory nerve and runs up along the posterior border of sternocleidomastoid to supply the posterior part of the upper neck and adjacent scalp behind the auricle. It may contribute to the supply of the auricle.
The great auricular nerve (C2, 3, mostly 2) is a large trunk passing almost vertically upwards over sternocleidomastoid; it is distributed to an area of skin on the face over the angle of the mandible and the parotid gland and to the parotid fascia. It also supplies the skin of the auricle over the whole of its cranial surface and on the lower part of its lateral surface below the external acoustic meatus, and skin over the mastoid region. Branches passing deep to the parotid gland supply the deep layer of the parotid fascia.
The transverse cervical nerve (C2, 3) curves round the posterior border of sternocleidomastoid, perforates the investing fascia and divides into ascending and descending branches that innervate the skin of the front of the neck from chin to sternum. The ascending branch communicates with the cervical branch of the facial nerve.
The supraclavicular nerve (C3, 4, but mostly 4) emerges with the other three nerves at the posterior border of sternomastoid and soon divides into several branches. They are distributed in three main groups (see Fig. 1.8, p. 12). The medial group supply the skin as far down as the sternal angle. The intermediate group proper pass anterior to the clavicle and supply skin as far down as the second rib. The lateral group cross the acromion to supply skin halfway down the deltoid muscle, and pass posteriorly to supply skin as far down as the spine of the scapula.
Dermatomes of the neck
In addition to the cutaneous branches of the cervical plexus described above, which supply the anterior and lateral skin of the neck, the greater occipital and third occipital nerves from posterior rami of C2 and C3 respectively provide sensory fibres for the back of the neck (Fig. 6.15). The first cervical nerve does not supply any skin. C2 supplies most of the superior part of the neck, extending into the occipital region of the scalp and forwards to the auricle and the face over the parotid gland. C3 supplies the cylindrical part of the neck, C4 extends over the clavicle to the sternal angle, across the top of the shoulder and down to the scapular spine at the back. There is much overlap across dermatome boundary lines.
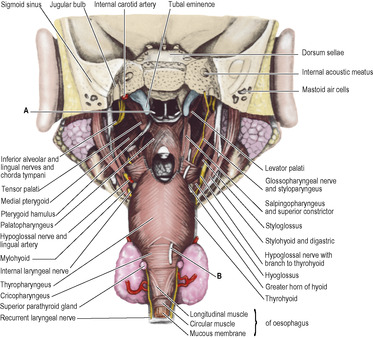
Anterior triangle
Beneath the investing layer of deep cervical fascia, between the mandible and the manubrium of the sternum, are longitudinal muscles supplied by the anterior rami of the upper three cervical nerves. They lie above or below the hyoid bone and there are four muscles in each group. The suprahyoid muscles comprise digastric, stylohyoid, mylohyoid and geniohyoid; the mylohyoids of each side unite to form the floor of the mouth, with the digastrics and stylohyoids superficial (below) and geniohyoids deep (above) to them. The infrahyoid muscles are sternohyoid and omohyoid, lying side by side in the same plane, and more deeply a wider sheet of muscle attached to the thyroid cartilage, namely thyrohyoid and sternothyroid. The last four are called the ‘strap muscles’ from their flat shape.
Suprahyoid muscles
Digastric
This arises as the posterior belly, from the digastric groove on the medial surface of the base of the mastoid process (Fig. 6.35). The triangular fleshy belly tapers down to the intermediate tendon, which is held beneath a fibrous sling attached to the junction of the body and the greater horn of the hyoid bone. The tendon is lubricated by a synovial sheath within the fibrous sling. The bifurcated tendon of insertion of stylohyoid which embraces the tendon plays no part in holding it down. The anterior belly lies on the inferior surface of mylohyoid, and connects the intermediate tendon to the digastric fossa on the inner surface of the mandible near the midline.
Nerve supply. The posterior belly is supplied by the facial nerve, by a branch arising between the stylomastoid foramen and the parotid gland, and the anterior belly by the nerve to mylohyoid.
Action. To depress and retract the chin, and to assist the lateral pterygoid in opening the mouth.
Stylohyoid
This arises from the back of the styloid process, high up near the base of the skull, and slopes down along the upper border of digastric. Its lower end divides to embrace the digastric tendon and is inserted by two slips into the junction of the greater horn and body of the hyoid bone.
Nerve supply. By the facial nerve, by a branch from that to the posterior belly of digastric.
Action. To retract and elevate the hyoid bone when swallowing.
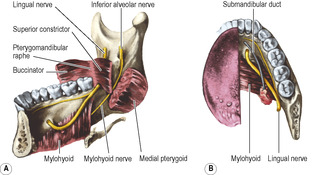
Mylohyoid
The muscles of each side unite to make a thin sheet forming the ‘diaphragm’ of the floor of the mouth (Fig. 6.6). Each arises from the whole length of the mylohyoid line of its own side on the inner aspect of the mandible from as far back as medial to the third molar tooth to below the mental spines (see Fig. 8.5B, p. 510). The two muscles slope downwards towards each other, and the posterior quarter of each is inserted into the anterior surface of the body of the hyoid bone. In front of this the anterior three-quarters of each interdigitate in a midline raphe which extends from the chin to the hyoid bone.
Nerve supply. By its own nerve, a branch of the inferior alveolar (from the mandibular division of the trigeminal nerve), which arises just before the parent nerve enters the mandibular foramen, pierces the sphenomandibular ligament and runs forward on the inferior surface of the mylohyoid, supplying it and the anterior belly of the digastric.
Action. It forms a mobile but stable floor of the mouth. The two muscles together form a gutter; contraction makes the gutter more shallow, thus elevating the tongue and the hyoid bone as when swallowing or protruding the tongue.
Geniohyoid
This slender muscle extends from the inferior mental spine (genial tubercle) of the mandible (see Fig. 8.5B, p. 510) to the upper border of the body of the hyoid bone (see Fig. 8.6, p. 512). The two muscles lie side by side between the mylohyoids and the base of the tongue (genioglossus), on the floor of the mouth.
Nerve supply. By a branch from the hypoglossal nerve, consisting of fibres from the C1 nerve and not from the hypoglossal nucleus.
Action. To protract and elevate the hyoid bone in swallowing, or if the hyoid is fixed, to depress the mandible.
Infrahyoid muscles
Sternohyoid
This flat strap of muscle is attached to the back of the upper part of the manubrium and the adjoining sternoclavicular joint and clavicle. Its upper attachment is to the lower border of the body of the hyoid bone. The two muscles lie edge to edge at the hyoid bone, but diverge from each other below.
Nerve supply. By a branch from the ansa cervicalis which enters the lower part of the muscle.
Omohyoid
This flat strap of muscle lies edge to edge with sternohyoid at its attachment to the lateral part of the inferior border of the hyoid bone (Fig. 6.5). As it descends it diverges somewhat from the sternohyoid and, passing deep to sternocleidomastoid, it comes to lie over the carotid sheath. Where it lies over the internal jugular vein, the muscle fibres are replaced by a flat tendon, a useful guide at operation to the underlying vein. A change of direction now occurs, and the inferior belly runs almost horizontally just above the level of the clavicle to pass back to its attachment to the upper border of the scapula and the transverse scapular ligament. The intermediate tendon and supraclavicular portion of the muscle are bound down close to the clavicle in a fascial sling derived from the deep layer of the investing layer of deep cervical fascia (see Fig. 2.2, p. 39), which results in the angulated course of the muscle.
 |
| Figure 6.5 |
Nerve supply. The superior root of the ansa cervicalis supplies the superior belly and the ansa supplies the inferior belly.
Thyrohyoid
This is a broader and shorter muscle that lies under cover of the upper ends of sternohyoid and omohyoid. It arises from the greater horn of the hyoid bone, and is inserted into the oblique line of the thyroid cartilage alongside sternothyroid.
Nerve supply. By a branch of the hypoglossal nerve, but the fibres are all ‘hitch-hiking’ from C1.
Sternothyroid
Broader than sternohyoid and lying deep to it, this muscle is attached lower down than sternohyoid to the posterior surface of the manubrium and the adjacent first costal cartilage. Its upper attachment is to the oblique line of the thyroid cartilage.
Nerve supply. By the ansa cervicalis, which gives a branch to the lower part of the muscle.
Actions of the infrahyoid muscles
They are all depressors of the larynx. Sternothyroid acts directly on the thyroid cartilage, the others act indirectly via the hyoid bone. Depression of the larynx increases the volume of the resonating chambers during phonation and thus affects the quality of the voice. The infrahyoid muscles also oppose the elevators of the larynx (mylohyoid, palatopharyngeus, stylopharyngeus, salpingopharyngeus), enabling them to act progressively and gradually. The infrahyoid muscles prevent ascent of the hyoid bone when the digastric and geniohyoid lower the mandible.
Submandibular gland
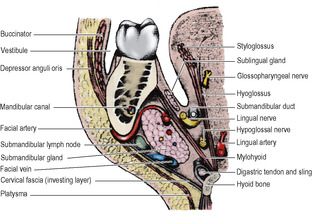
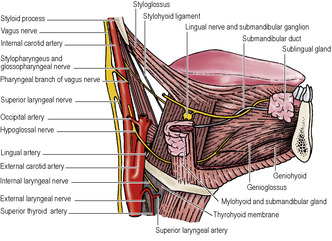
The submandibular gland, mixed mucous and serous in type, consists of a large superficial part and a small deep part which are continuous with one another round the free posterior margin of mylohyoid (Fig 6.24).
The superficial part (Fig. 6.6) has three surfaces: lateral, inferior and medial. The lateral surface lies against the submandibular fossa of the mandible (see Fig. 8.5B, p. 510), overlapping the front of the medial pterygoid insertion and being deeply grooved posteriorly by the facial artery which hooks under the mandible to reach the face at the front of the masseter muscle. The inferior or superficial surface is covered by skin, platysma and the investing fascia and is crossed by the facial vein and the cervical branch of the facial nerve, and sometimes by the marginal mandibular branch of the facial nerve (see p. 353), the nerves lying outside the investing fascia. Submandibular lymph nodes lie in contact with the surface of the gland and within its substance, hence the need to remove the gland as well as nodes in the operation of radical neck dissection. The medial surface lies against the mylohyoid, and behind it on the hyoglossus, lingual nerve, hypoglossal nerve and its accompanying veins. The facial artery is at first deep to the gland, and then grooves the posterosuperior part as it hooks over the top of the gland on to its lateral surface.
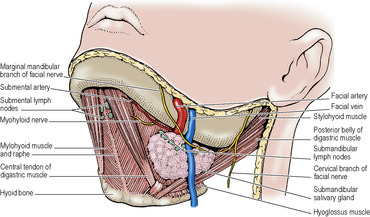 |
| Figure 6.6 |
The deep part of the gland extends forwards for a variable distance, between mylohyoid and hyoglossus, below the lingual nerve and above the hypoglossal nerve.
The submandibular duct (of Wharton) is 5cm long (the same length as the parotid duct) and emerges from the medial surface of the superficial part of the gland near the posterior border of mylohyoid. It runs with the deep part, forwards and slightly upwards, first between mylohyoid and hyoglossus, and then between the sublingual gland and genioglossus, to open into the floor of the mouth on the sublingual papilla beside the frenulum of the tongue. As it lies on hyoglossus, the duct is crossed laterally by the lingual nerve which then turns under the duct to pass medially to the tongue (Fig. 6.7).
Blood supply
From the facial artery, with veins draining into the facial vein.
Lymph drainage
To the submandibular lymph nodes.
Nerve supply
Secretomotor fibres to the gland have their cell bodies in the submandibular ganglion (see p. 22), which hangs suspended from the lingual nerve on the surface of hyoglossus. The preganglionic fibres pass from cell bodies in the superior salivary nucleus in the pons by way of the nervus intermedius, facial nerve, chorda tympani and the lingual nerve (see pp. 365–366). Postganglionic fibres pass to the submandibular gland and also to the lingual nerve for transmission to the sublingual gland. Sympathetic (vasoconstrictor) fibres come from the plexus around the facial artery.
Development
An ectodermal groove in the floor of the mouth becomes converted into a tunnel whose blind end proliferates to form the secreting acini.
Surgical approach
The gland is exposed by a skin crease incision about 4cm below the mandible, which continues through platysma and investing fascia on to the gland, to avoid the marginal mandibular branch of the facial nerve which may lie over the gland (see p. 353). Removal of the gland requires ligation of the facial vein which lies on the gland surface. The facial artery needs to be separated from its groove on the posterosuperior part of the gland, or a segment of the artery removed with the gland. The hypoglossal nerve and lingual nerve need to be safeguarded, the latter particularly when the duct is ligated and divided. The removal of a stone from the duct is carried out from within the mouth by incising the mucous membrane and duct over the stone; the mucosal and duct incisions are not sutured.
Thyroid gland
The thyroid gland is situated low down at the front of the neck. It consists of two symmetrical lobes united by an isthmus that lies in front of the second, third and fourth tracheal rings (Fig. 6.5). The lobes lie on either side of the larynx and trachea, extending from the oblique line of the thyroid cartilage to the sixth tracheal ring. It weighs about 25g. In addition to its own capsule, the gland is enclosed by an envelope of pretracheal fascia.
Each lateral lobe is pear-shaped with a narrow upper pole and a broader lower pole, and appears approximately triangular on cross-section with lateral, medial and posterior surfaces. The lateral (superficial) surface is under cover of sternothyroid and sternohyoid. The medial surface lies against the lateral side of the larynx and upper trachea, with the lower pharynx and upper oesophagus immediately behind. This surface is related to the cricothyroid muscle of the larynx and the inferior constrictor of the pharynx, as well as to the external and recurrent laryngeal nerves. The posterior surface overlaps the medial part of the carotid sheath, i.e. the part containing the common carotid artery; if enlarged, the lobe may extend across the more laterally placed internal jugular vein. The parathyroid glands usually lie in contact with this surface, between it and the fascial sheath.
The relationship of the recurrent laryngeal nerves (see p. 368) to the thyroid lobes has importance in thyroid surgery. As they approach the medial surface of the gland from below, the nerves lie in or in front of the groove between the trachea and oesophagus. The left nerve, which recurves around the arch of the aorta in the superior mediastinum, is more likely to have entered the groove and lies posterior (though occasionally anterior) to the inferior thyroid artery. The right nerve recurves around the right subclavian artery at the root of the neck and may be more lateral to the trachea, passing anterior or posterior to the inferior thyroid artery or in between its branches. Each nerve is behind the pretracheal fascia, and runs medial or lateral or through a thickening of the fascia attached to the cricoid cartilage and upper tracheal rings (the suspensory ligament of Berry). The nerve runs behind the cricothyroid joint and passes upwards under cover of the inferior constrictor. At the level of the upper border of the isthmus the nerve often divides into two. If so, the anterior (larger) branch is the motor branch to laryngeal muscles, and the posterior branch is sensory only. The rare non-recurrent right laryngeal nerve (see p. 27) may be a hazard during thyroid surgery.
The smaller external laryngeal nerve lies on the inferior constrictor, close behind the superior thyroid artery, as it runs down medial to the upper pole to supply cricothyroid.
The isthmus joins the anterior parts of the lobes, towards their lower poles. The posterior surface of the isthmus is firmly adherent to the second, third and fourth rings of the trachea, and the pretracheal fascia is here fixed between them. This fixation and the investment of the whole gland by pretracheal fascia are responsible for the gland moving up and down with the larynx during swallowing. An anastomosis between the two superior thyroid arteries runs across the upper border of the isthmus, and tributaries of the inferior thyroid veins emerge from its lower border.
A small portion of gland substance often projects upwards from the isthmus, generally to the left of the midline, as the pyramidal lobe and represents a devel-opment of glandular tissue from the caudal end of the thyroglossal duct (see p. 26). It may be attached to the inferior border of the hyoid bone by fibrous tissue; muscle fibres sometimes present in it are named levator glandulae thyroideae and are innervated by a branch of the external laryngeal nerve. Separate small masses of thyroid tissue (accessory thyroid glands) are not uncommonly found near the hyoid bone, in the tongue, in the superior mediastinum, or anywhere along the path of descent of the thyroglossal duct, though their presence may only be revealed by histological study.
Blood supply
The superior thyroid artery, the first branch from the anterior aspect of the external carotid (see p. 342), after giving off its sternocleidomastoid and superior laryngeal branches, pierces the pretracheal fascia as a single vessel to reach the summit of the upper pole. The external laryngeal nerve is immediately behind the artery as the vessel approaches the pole, but they part company as the artery reaches the gland and the nerve descends to supply the cricothyroid muscle. The artery divides on the gland into an anterior branch that runs down to the isthmus and a posterior branch that runs down the back of the lobe and anastomoses with an ascending branch of the inferior thyroid artery from the lower pole. In thyroidectomies the artery is ligated close to the upper pole, or its anterior and posterior branches are ligated instead, to avoid damage to the external laryngeal nerve.
The inferior thyroid artery, from the thyrocervical trunk (see p. 349), arches upwards and medially behind the carotid sheath and then loops downwards to the lower pole. It divides outside the pretracheal fascia into branches that pierce the fascia separately to reach the lower part of the gland. As described above, the recurrent laryngeal nerve has a variable relationship to the artery but always lies behind the pretracheal fascia. Ligating the inferior thyroid artery well lateral to the gland, or carefully ligating its small branches on the surface of the gland, helps to safeguard the nerve. The inferior thyroid artery gives off the ascending cervical artery and small pharyngeal, oesophageal, laryngeal and tracheal branches before its terminal distribution to the thyroid gland; the small inferior laryngeal artery ascends with the recurrent nerve.
A thyroidea ima artery enters the lower part of the isthmus in 3% of individuals. It arises from the brachiocephalic trunk, arch of the aorta or right common carotid artery.
From a venous plexus on the surface of the gland the superior thyroid vein follows the superior thyroid artery and enters either the internal jugular or facial vein in about equal proportions. The middle thyroid vein crosses anterior to the common carotid artery to drain into the internal jugular vein; early ligature and division of this vein during thyroid surgery facilitates mobilisation of the gland. The inferior thyroid veins are multiple and drain downwards mainly into the left brachiocephalic vein; one may enter the right brachiocephalic vein.
Lymph drainage
The lymphatics from the thyroid gland drain mainly to deep cervical nodes. A few pass into prelaryngeal, pre- and paratracheal nodes, and a few drain directly into the thoracic duct.
Nerve supply
Sympathetic (vasoconstrictor) nerves from the superior, middle and inferior cervical ganglia accompany the thyroid arteries.
Structure
The thyroid consists essentially of a mass of more or less rounded follicles containing varying amounts of colloid produced by the single layer of epithelial (follicular) cells that form the walls of the follicles. The thyroid is unique in being the only endocrine gland to store its secretion outside the cells. The colloid is iodinated when in the follicle and reabsorbed by the cells before being discharged into blood capillaries. The main hormonal products are thyroxine (T4) and triiodothyronine (T3). Less than 2% of the epithelial cells are the C or parafollicular cells which secrete calcitonin. The C cells are scattered on the outer aspects of the follicles and do not reach the lumina of the follicles. The thyroid gland is highly vascular.
Development
The gland develops as a proliferation of cells from the caudal end of the thyroglossal duct (see p. 26). The parafollicular calcitonin-producing cells develop from the ultimobranchial body (fifth pharyngeal pouch), under the influence of neural crest cells.
Surgical approach
The thyroid gland is approached surgically through a transverse incision in a low skin crease on the front of the neck. The investing fascia is divided vertically and the sternohyoid and the sternothyroid muscles retraced, or divided at a high level, to safeguard their nerve supply and to prevent adherence of their subsequent suture line to the closure of the skin incision. The pretracheal fascia needs to be divided to expose the gland proper.
Parathyroid glands
The small parathyroid glands normally lie behind the lobes of the thyroid gland. There are usually four glands (in 90% of subjects), two on each side. Each weighs about 50mg.
The superior gland is the more constant in position; it is usually within the thyroid’s pretracheal fascial capsule, at the middle of the back of the thyroid lobe, level with the first tracheal ring and above the inferior thyroid artery. The inferior gland is less constant in position. It is usually within the pretracheal fascial sheath behind the lower pole; but it may be in the gland itself, or outside the fascial sheath in a variable position in the neck, or in the superior or posterior mediastinum. The glands are not necessarily on the same level on each side. They are brownish-yellow, which helps to distinguish them from the deep red of the thyroid gland. They are easily subject to subcapsular haematoma formation on handling.
Blood supply
Both upper and lower parathyroids are usually supplied by the inferior thyroid artery, otherwise by an anastomosis between the superior and inferior arteries. Their minute veins join thyroid veins.
Nerve supply
Sympathetic vasoconstrictor fibres enter with the arteries.
Structure
The gland is a mass of small closely packed chief or principal cells which secrete the parathyroid hormone (PTH). The mass of cells bears a superficial resemblance to lymphoid tissue, but the number of blood capillaries in the gland provides a clear distinction. Scattered among the chief cells are small groups of slightly larger oxyphil cells.
Development
The superior gland is termed parathyroid IV because it develops from the fourth pharyngeal pouch. The inferior gland is parathyroid III, developed from the third pouch, but displaced caudally by the descent of the thymus from the same pouch (see p. 26); hence its liability to end up in unusual positions.
Surgical approach
For parathyroidectomy the lobes of the thyroid gland are exposed as for thyroidectomy, and then retracted forwards and medially so that the posterior surfaces can be inspected for the parathyroids. If not obvious, branches of the inferior thyroid artery are followed and should lead to the glands. Exposure of the thymus through a median sternotomy may be necessary.
Trachea
The trachea (Fig. 6.5) begins at the level of C6 vertebra in continuity with the larynx, being attached to the lower margin of the cricoid cartilage by the cricotracheal ligament. Of the total length of 10cm, 5cm are in the neck from the cricoid cartilage to the jugular notch. From the neck the trachea passes into the thorax.
The cervical part lies in the midline of the neck, in contact with the front of the oesophagus. In the groove between trachea and oesophagus runs the recurrent laryngeal nerve. To the side of the trachea is the carotid sheath. The isthmus of the thyroid gland is adherent to the second, third and fourth tracheal rings and the lobes of the gland lie against the lateral sides of the trachea as far down as the sixth ring. The inferior thyroid veins and anterior jugular venous arch lie in front, and also (if present) the thyroidea ima artery and the upper end of a persistently large thymus. On account of the shape of the lower cervical and upper thoracic parts of the vertebral column, the trachea passes downwards and backwards as it enters the thorax. Although close to the skin at the upper end, it is 2cm or more deep to the front of the jugular notch.
The thoracic part of the trachea and other features are described on page 194.
Tracheotomy and tracheostomy
Tracheotomy implies making an incision in the trachea; tracheostomy involves removing a small part of the wall (making a stoma), but the strict distinction between these terms is often ignored. In an emergency, laryngotomy (incising the cricothyroid ligament, see p. 393) provides a subglottic airway; the procedure also gives access to the trachea for sucking out excess secretions. Depending on the speed with which tracheostomy needs to be performed, the skin incision is vertical from the lower border of the thyroid cartilage to the jugular notch, or (preferably) transverse 2cm below the cricoid cartilage. The sternohyoid and sternothyroid muscles are retracted laterally. The isthmus of the thyroid gland is usually divided and an opening made by removing part of the second and third tracheal rings so that a tracheostomy tube can be inserted. In the narrow trachea of children only a vertical incision is made in the trachea (tracheotomy), as removal of any segment of tracheal wall tends to lead to tracheal stenosis.
Oesophagus
The oesophagus commences in continuity with the pharynx at the level of the lower border of the cricoid cartilage (C6 vertebra). It lies in front of the prevertebral fascia behind the trachea. It is overlapped on either side by the lower poles of the thyroid gland, beyond which, on the left side, its edge is visible posterolateral to the trachea. The thoracic duct runs upwards behind the lower part of its left border. The recurrent laryngeal nerves are on each side in the groove between trachea and oesophagus.
The oesophagus continues into the thorax and is further described on page 208.
Great vessels of the neck
Common carotid artery
The common carotid artery arises on the left side from the arch of the aorta, where it lies in front of the subclavian artery up to the sternoclavicular joint. Here the two arteries diverge. On the right the brachiocephalic trunk bifurcates behind the sternoclavicular joint into common carotid and subclavian arteries. The common carotid gives off no branches proximal to its bifurcation. It lies within the medial part of the carotid sheath, with the internal jugular vein lateral to it and the vagus nerve deeply placed between the two vessels. The sympathetic trunk is behind the artery and outside the sheath, which is overlapped superficially by the infrahyoid muscles and sternocleidomastoid. Medial to the sheath is the trachea and oesophagus and, at a higher level, the larynx and pharynx. The thyroid gland overlaps the sheath anteromedially and the inferior thyroid artery crosses from the thyrocervical trunk to the gland behind the sheath.
The common carotid artery usually bifurcates at the level of the upper border of the lamina of the thyroid cartilage (upper border of C4 vertebra) into the external and internal carotids; it may do so higher near the tip of the greater horn of the hyoid bone (C3 vertebra). The terminal portion of the artery often shows a slight dilatation, the carotid sinus, which includes the commencement of the internal carotid artery.
The carotid pulse can be felt by pressing backwards between the trachea and lower larynx medially and sternocleidomastoid laterally, pressing the artery against the anterior tubercle of the transverse process of C6 vertebra (carotid tubercle of Chassaignac). The surface marking of the common carotid artery is along a vertical line from the sternoclavicular joint to the level of the upper border of the thyroid cartilage. The vessel can be surgically exposed by retracting the lower part of sternocleidomastoid backwards and incising the carotid sheath. The middle thyroid vein is divided between ligatures.
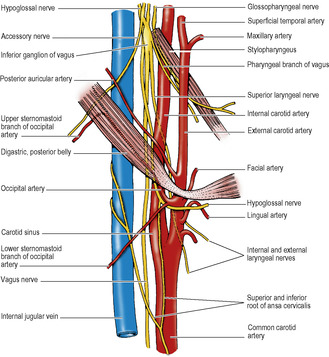
External carotid artery
The external carotid artery at its commencement lies against the side wall of the pharynx somewhat anteromedial to the internal carotid artery. It then ascends in front of the internal carotid deep to the posterior belly of digastric and stylohyoid, above which it pierces the deep lamina of the parotid fascia and enters the gland. It divides within the gland behind the neck of the mandible into the maxillary and superficial temporal arteries. As the external carotid artery lies in the parotid gland it is separated from the internal carotid by the deep part of the gland and its fascia, styloid process and its continuation the stylohyoid ligament, styloglossus and the ‘pharyngeal’ structures: stylopharyngeus muscle, glossopharyngeal nerve and pharyngeal branch of the vagus (and, if present, the track of a branchial fistula, see p. 26). At the commencement of the artery the internal jugular vein lies lateral, but higher up it is posterior and deep to the artery. The facial vein crosses the artery, with the hypoglossal nerve lying between. Except at its commencement the vessel lies in front of the anterior border of sternocleidomastoid.
The surface marking of the external carotid is along a line from the bifurcation of the common carotid passing up behind the angle of the mandible to a point immediately in front of the tragus of the ear.
Surgical approach. The vessel can be exposed in front of the upper part of sternocleidomastoid before it enters the parotid gland by ligating the facial vein. The hypoglossal nerve which crosses the external and internal carotids superficially must not be damaged.
Branches. Before it divides into its two terminal branches the external carotid artery gives off six branches, three from in front, two from behind and one from its deep (medial) aspect. The three from in front are the superior thyroid, lingual and facial, and they diverge widely. The two from behind are the occipital and posterior auricular, which pass up deep to and above the posterior belly of digastric respectively. The branch from the medial side is the ascending pharyngeal, which ascends to the base of the skull on the side wall of the pharynx, alongside the internal carotid artery.
The superior thyroid artery arises at the commencement of the external carotid. It runs almost vertically downwards, with the vein, to the upper pole of the thyroid gland (see p. 339), with the external laryngeal nerve close behind it, alongside the larynx (Fig. 6.24). Before reaching the thyroid gland it gives off infrahyoid, sternocleidomastoid, superior laryngeal and cricothyroid branches. The superior laryngeal artery pierces the thyrohyoid membrane with the internal laryngeal nerve. The cricothyroid artery crosses the upper part of the crico-thyroid membrane to anastomose with the contralateral artery.
The lingual artery arises from the front of the external carotid above the superior thyroid, near the tip of the greater horn of the hyoid bone. It forms a short loop (Fig. 6.22), then passes forwards along the upper border of the greater horn, deep to hyoglossus (p. 381). It is accompanied by the lingual vein. The loop of the artery is crossed laterally by the hypoglossal nerve and its companion vein, the latter opening into the facial vein.
The facial artery arises from the front of the external carotid above the lingual artery (sometimes by a common linguofacial trunk with the lingual) and runs upwards on the superior constrictor, deep to the digastric and stylohyoid muscles, then deep to the submandibular salivary gland. It grooves the posterosuperior part of the gland. As the artery lies on the superior constrictor muscle it gives off a tonsillar and an ascending palatine branch to the tonsil and soft palate. The facial artery then makes an S bend, curling over the submandibular gland (Fig. 6.7) and crossing the inferior border of the mandible, where its pulsation can be felt, at the anterior border of masseter. Before passing to the face it gives off the submental artery, which accompanies the mylohyoid nerve into the submandibular fossa and sends perforating branches through the mylohyoid to anastomose with a sublingual branch of the lingual artery.
The occipital artery arises from the back of the external carotid on a level with the facial artery. It courses backwards deep to the lower border of the posterior belly of digastric. It grooves the base of the skull at the occipitomastoid suture, deep to the digastric notch on the mastoid process (Fig. 6.35), and passes through the apex of the posterior triangle to supply the back of the scalp (see p. 356). The artery gives off two branches to sternocleidomastoid. The upper branch is a guide to the accessory nerve in front of the upper border of the muscle. At its origin the occipital artery crosses lateral to the hypoglossal nerve, which hooks around it from behind (Fig. 6.24), the nerve being held down here by the lower sternocleidomastoid branch of the artery (Fig. 6.23).
The posterior auricular artery arises above the level of the digastric muscle, often within the substance of the parotid gland. It runs up superficial to the styloid process above the digastric posterior belly and crosses the surface of the mastoid process to supply the scalp. Auricular branches supply the pinna of the ear. Its stylomastoid branch enters the stylomastoid foramen and supplies the facial nerve; this branch may arise instead from the occipital artery.
The ascending pharyngeal artery arises just above the commencement of the external carotid, from its deep aspect. It runs up along the side wall of the pharynx in front of the prevertebral fascia, deep to the internal carotid artery. It supplies the pharyngeal wall and the soft palate and sends meningeal branches through the nearby foramina in the base of the skull (foramen lacerum, jugular foramen, hypoglossal canal).
Internal carotid artery
The internal carotid artery arises at the bifurcation of the common carotid (see p. 342) and continues upwards within the carotid sheath (see p. 366). At its commencement it shows a slight bulge, the carotid sinus. Here the arterial wall is thin and its contained baroreceptors are supplied by the glossopharyngeal and vagus nerves, which mediate blood pressure impulses to medullary centres. The carotid body is a small structure lying behind the bifurcation of the common carotid artery, or between its branches, from which it receives two or three very small glomic arteries. Its cells are chemoreceptors concerned (like the aortic bodies, see p. 192) with respira-tory reflexes, and are innervated by the glossopharyngeal and vagus nerves. Carotid body tumours form a swelling at the anterior border of sternocleidomastoid at the level of the carotid bifurcation, and exhibit transmitted pulsation from the arteries.
The internal carotid artery is lateral to the external carotid at its origin, but soon passes up posteriorly to a medial and deeper level. It has no branches and passes straight up in the carotid sheath, beside the pharynx, to the carotid canal in the base of the skull; its intracranial course is considered on pages 445 and 449.
Behind the internal carotid artery in the neck is the sympathetic trunk (outside the carotid sheath), pharyngeal veins and the superior laryngeal branch of the vagus. The ascending pharyngeal artery is medial to it. The internal jugular vein is lateral, with the vagus nerve deeply placed between artery and vein. Superficially near its origin it is crossed by the lingual and facial veins, the occipital artery and hypoglossal nerve. The superior root of the ansa cervicalis runs downwards along it, embedded in the carotid sheath. At a higher level it is crossed by the posterior belly of digastric and stylohyoid and the posterior auricular artery, and by the structures that separate it from the external carotid (see above).
The surface marking of the internal carotid artery in the neck is along a line from the bifurcation of the common carotid artery to the head of the mandible.
Surgical approach. The internal carotid is exposed in the neck by an incision along the anterior border of sternocleidomastoid. The muscle is retracted backwards, the facial and lingual veins divided between ligatures, and the carotid sheath is incised. The hypoglossal nerve must be safeguarded and this may require division of the lower sternocleidomastoid branch of the occipital artery. The emergence of branches from the external carotid artery ensures its differentiation from the internal carotid.
Internal jugular vein
The internal jugular vein emerges from the jugular bulb at the posterior compartment of the jugular foramen (Fig. 6.35). At first behind the internal carotid artery, it lies on the transverse process of the atlas, crossed by the accessory nerve. It receives the inferior petrosal sinus as its first tributary, just below the base of the skull; the sinus passing back lateral or medial to the glossopharyngeal, vagus and accessory nerves. The vein passes down to gain the lateral side of first the internal carotid artery and then the common carotid artery, within the loose lateral part of the carotid sheath, with the vagus nerve deeply placed between the vein and the arteries. In the lower part of its course the vein is overlaid by the sloping sternocleidomastoid. Deep cervical lymph nodes within the sheath are closely adjacent to the vein throughout its course. Its posterior relations include the cervical plexus lying on levator scapulae and scalenus medius, and the phrenic nerve on scalenus anterior. The thoracic duct crosses behind the left vein at the level of C7 vertebra. The inferior root of the ansa cervicalis curls round its lateral border, to unite with the superior root (from the hypoglossal nerve) at a variable level in front of the vein. Low down the tendon of omohyoid crosses the vein, providing a useful guide to its position. The terminal part of the vein lies deep to the triangular interval between the sternal and clavicular heads of sternocleidomastoid (Fig. 6.2). It joins the subclavian to form the brachiocephalic vein behind the sternal end of the clavicle.
The tributaries of the internal jugular vein below the inferior petrosal sinus are the pharyngeal, lingual, facial and superior and middle thyroid veins. The lingual and superior thyroid veins may join the facial vein and other variations are possible.
At its commencement and termination the vein is slightly dilated to form superior and inferior bulbs. There is a pair of valves above the inferior bulb.
The surface marking of the internal jugular vein is along a line from the lobule of the ear to the sternal end of the clavicle, between the two heads of sternocleidomastoid. The jugular venous pulse is a guide to jugular venous pressure, which is the same as right atrial or central venous pressure and thus an indicator of cardiovascular function. With a patient reclining at 45° the jugular venous pulse should be visible just above the clavicle.
Catheterization. The right internal jugular vein (on a direct path to the right atrium) can be cannulated for the insertion of a central venous line, for measurements of central venous pressure, or the rapid administration of drugs when a peripheral approach would be too slow. The vein is usually approached through the centre of the triangle formed by the two heads of sternocleidomastoid and the clavicle. The needle is directed caudally, parallel to the sagittal plane at a 30° posterior angle with the coronal plane, entering the vein at about 4–5cm depth. (The subclavian vein is an alternative, see p. 348). The most common complication is haematoma formation; others include common carotid artery puncture, vagus nerve injury and pneumothorax due to pleural perforation.
The ansa cervicalis lies on the front of the internal jugular vein and gives branches to the infrahyoid muscles. It is usually embedded within the anterior wall of the carotid sheath and classified as one of its contents. It is formed by union of superior and inferior roots. The superior root is a branch of the hypoglossal nerve containing only C1 fibres, which have hitch-hiked along the hypoglossal nerve. It runs down on the front of the internal and common carotid arteries, giving a branch to the superior belly of omohyoid.
The inferior root is formed by union of a branch each from C2 and C3 anterior rami in the cervical plexus. The single nerve so formed spirals from behind around the internal jugular vein and runs down to join the superior root in a wide loop over the lower part of the vein, from which branches arise for the infrahyoid muscles (sternohyoid, sternothyroid and inferior belly of omohyoid). Sometimes the inferior root passes forwards between internal jugular vein and internal carotid artery.
The uppermost part of the hypoglossal nerve in the neck is described on page 368. It emerges between the internal carotid artery and internal jugular vein deep to the posterior belly of digastric. Hooking round the occipital artery, which runs backwards lateral to the nerve, it curves forwards lateral to the internal and external carotids and the loop of the lingual artery (Fig. 6.23). As it crosses these arteries it lies just below the posterior belly of the digastric, behind its tendon and just above the tip of the greater horn of the hyoid bone. It gives off the superior root of the ansa cervicalis as it crosses the internal carotid and the branch to thyrohyoid (C1 fibres) as it crosses the lingual artery. It passes forwards on the lateral surface of hyoglossus deep to mylohyoid to enter the mouth, giving off the branch to geniohyoid (C1 fibres) as it does so (Fig. 6.24).
Summary of triangles of the neck
Posterior triangle
Boundaries. Sternocleidomastoid, trapezius, clavicle.
Contents. Occipital, transverse cervical, suprascapular and subclavian arteries; transverse cervical, suprascapular and external jugular veins; accessory nerve; cervical plexus branches and brachial plexus trunks (deep to prevertebral fascia); inferior belly of omohyoid; lymph nodes.
Anterior triangle
Boundaries. Sternocleidomastoid, mandible, midline. Subdivided into:
Carotid triangle
Boundaries. Sternocleidomastoid, posterior belly of digastric, superior belly of omohyoid.
Contents. Bifurcation of common carotid artery and branches of external carotid (except posterior auricular); lingual, facial and superior thyroid veins; hypoglossal, internal and external laryngeal nerves, and superior root of ansa cervicalis; lymph nodes.
Digastric triangle
Boundaries. Mandible, anterior and posterior bellies of digastric.
Contents. Submandibular gland and lymph nodes; facial, submental and mylohyoid vessels; hypoglossal and mylohyoid nerves.
Submental triangle
Boundaries. Anterior bellies of digastric, body of hyoid bone. (Triangle crosses midline.)
Contents. Anterior jugular veins; lymph nodes.
Muscular triangle
Boundaries. Sternocleidomastoid, superior belly of omohyoid, midline from hyoid bone to jugular notch.
Contents. Parts of larynx, trachea, pharynx, oesophagus, thyroid and parathyroid glands; their vessels and nerves; lymph nodes.
Part three. Prevertebral region
Prevertebral muscles of the neck
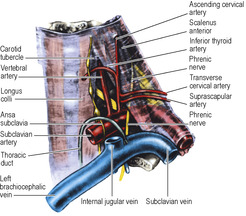
Some relatively weak flexor muscles extend in front of the vertebral column from skull to superior mediastinum. They are covered anteriorly by the strong prevertebral fascia (Fig. 6.8).
Rectus capitis anterior extends from just in front of the occipital condyle to the lateral mass of the atlas.
Rectus capitis lateralis lies edge to edge with the former muscle; it extends from the jugular process of the occipital bone to the transverse process of the atlas. The anterior ramus of C1, passing forwards lateral to the atlanto-occipital joint, supplies each muscle and then passes between them to sink into the overlying longus capitis muscle. It gives a branch to the hypoglossal nerve, which is distributed in the meningeal branch, the superior root of the ansa cervicalis and the branches to thyrohyoid and geniohyoid. These two small rectus muscles assist in flexion and lateral flexion of the head.
Longus capitis is attached to the basiocciput, in front of rectus capitis anterior and behind the wall of the nasopharynx (pharyngobasilar fascia, see p. 383), which it bulges forwards slightly. It is attached below by four tendons, in line with those of scalenus anterior, to the anterior tubercles of the transverse processes of the four ‘typical’ cervical vertebrae (C3–6). It is supplied by anterior rami of the upper four cervical nerves. It flexes the head.
Longus colli extends from the atlas into the superior mediastinum. It consists of upper, lower and central fibres, which together give the muscle a triangular shape, the elongated base of the triangle being close to the midline (Fig. 6.8). It is attached to the anterior tubercle of the altas, the front of the bodies of vertebrae C2–7 and T1–3, and to the anterior tubercles of the transverse processes of vertebrae C3–6.
Longus colli is supplied segmentally by the anterior rami of the spinal nerves. It is a flexor of the neck.
The prevertebral fascia is described on page 331.
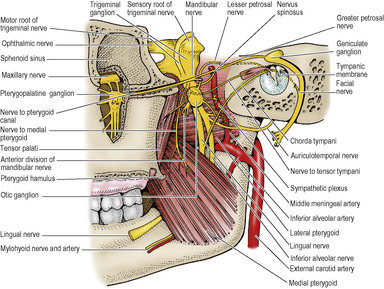
Cervical sympathetic trunk
The cervical part of the sympathetic trunk (Fig. 6.8) ascends from the thorax across the neck of the first rib, medial to the highest intercostal vein. It runs up medial to the vertebral artery and lies in front of the prevertebral fascia, behind the carotid sheath and medial to the vagus nerve. It ends at the superior cervical ganglion.
The superior cervical ganglion, containing about 1 million cell bodies, is about 3cm long and lies in front of C2 and C3 vertebrae. The middle cervical ganglion is a small, inconstant ganglion lying medial to the carotid tubercle (C6 vertebra) and in front of the inferior thyroid artery. The inferior cervical ganglion lies behind the commencement of the vertebral artery. A small mass when separate, it is often fused with the first thoracic ganglion to form the cervicothoracic (stellate) ganglion, in front of the neck of the first rib. The middle ganglion is connected to the inferior (or stellate) ganglion by two or more strands, one of which loops down in front of and under the subclavian artery, the ansa subclavia (Fig. 6.8).
No white rami enter the ganglia from the cervical nerves: all the preganglionic fibres ascend from the thoracic part of the trunk. As elsewhere, the branches of the ganglia are somatic and visceral in their distribution.
Grey rami pass to all eight cervical nerves. The superior ganglion gives grey rami to the first four (i.e. to the cervical plexus), the middle ganglion to the next two (5 and 6) and the inferior ganglion to the last two (7 and 8) anterior rami (i.e. to the brachial plexus for distribution to the upper limb).
Each ganglion gives a cardiac branch. The branch from the upper left ganglion runs down to the superficial cardiac plexus, the others all pass to the deep plexus. All six cardiac branches pass down behind the common carotid and subclavian arteries to reach the superior mediastinum.
Vascular branches ‘hitch-hike’ their way along arteries. The superior ganglion gives branches to the internal carotid and external carotid arteries. The internal carotid nerve accompanies the internal carotid artery into the skull and forms the internal carotid plexus, from which fibres are distributed to all branches of the artery, the pterygopalatine ganglion and the eye, the latter including the motor supply of the dilator pupillae of the iris. The plexus on the external carotid artery accompanies all branches of the vessel and in addition supplies sympathetic fibres to the pharyngeal plexus and the submandibular and otic ganglia.
The middle cervical ganglion gives branches to the inferior thyroid artery.
The inferior cervical ganglion gives branches to the subclavian artery and a large branch to the vertebral artery, which forms the vertebral plexus.
Interruption of the cervical sympathetic pathway gives rise to Horner’s syndrome, described on page 408.
Part four. Root of the neck
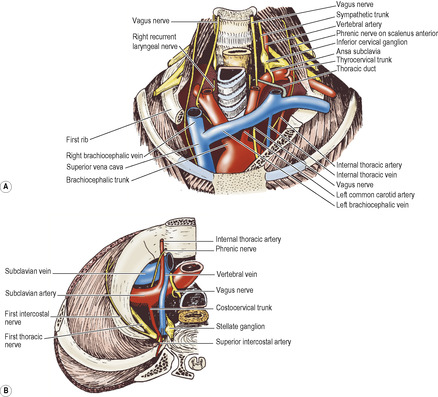
The root of the neck (thoracic outlet) is bounded by the first thoracic vertebra, the first pair of ribs and their cartilages and the manubrium of the sternum. The key to the root of the neck is the scalenus anterior muscle and its relations (Figs 6.8, 6.9 A and 6.10).
 |
| Figure 6.10 |
Scalenus anterior
This flat muscle arises from the anterior tubercles of the four ‘typical’ cervical vertebrae (3–6) by four slender tendons of origin which lie end to end with those of longus capitis (Fig. 6.8). The muscle passes forwards, laterally and downwards to end in a narrow tendon attached to the scalene tubercle and adjacent ridge on the inner border and upper surface of the first rib (see Fig. 4.34, p. 218).
Nerve supply. By separate branches from the anterior rami of C4–6 nerves.
Action. It is more important as a landmark than an active muscle. It assists in flexion and rotation of the neck, and helps to stabilize the first rib. Even in quiet respiration it shows some electromyographic activity.
Anterior relations
The phrenic nerve passes vertically down across the obliquity of the muscle, plastered thereto by the prevertebral fascia (Fig. 6.10) and a pad of fat lies in front of the prevertebral fascia. The nerve leaves the medial border of the muscle low down and crosses in front of the subclavian artery and its internal thoracic branch, behind the subclavian vein. (Occasionally the phrenic nerve may pass in front of the subclavian vein or posterior to the internal thoracic artery.) Lying on the suprapleural membrane it passes medial to the apex of the lung, crossing in front of the vagus nerve as it enters the superior mediastinum. The ascending cervical artery, a branch of the inferior thyroid artery or the thyrocervical trunk, runs up on the prevertebral fascia medial to the phrenic nerve.
In front of the prevertebral fascia the superficial cervical and suprascapular arteries lie between the scalenus anterior and the carotid sheath (internal jugular vein). The vagus nerve in the carotid sheath passes down in front of the subclavian artery, on the right side giving off its recurrent laryngeal branch. The latter hooks under the artery and passes upwards (Fig. 6.9A). The vagus nerve inclines posteriorly and runs on the medial surface of the apex of the lung to enter the superior mediastinum. The internal jugular vein has inferior deep cervical lymph nodes closely adjacent to it.
The subclavian vein lies in a groove on the first rib and, due to the slope of the rib, lies at a lower level than the insertion of scalenus anterior (Fig. 6.9A). Running medially it joins the internal jugular vein at the medial border of scalenus anterior to form the brachiocephalic vein; the thoracic duct on the left and the right lymph duct on the right enter the angle of confluence of the two veins.
Catheterization. The right subclavian vein can be used for the placement of a central venous line, instead of the internal jugular (see p. 344); it is preferred by many operators and is more comfortable for the patient. The usual approach is infraclavicular, from a point 2cm below the midpoint of the clavicle along a line that passes behind the clavicle towards the jugular notch of the sternum. The needle pierces the clavipectoral fascia and enters the vein just behind the fascia. Pneumothorax due to puncture of the pleura and lung, and puncture of the subclavian artery are complications of this procedure. The vein is also used for the placement of wires from cardiac pacemakers, which are usually implanted in connective tissue over the upper lateral part of pectoralis major.
Medial relations
The medial edge of scalenus anterior makes a pyramidal space with the lateral border of the lower part of longus colli. The prevertebral fascia in front of these muscles is attached to bone at their opposing margins and there is no fascial roof across the pyramidal space between the muscles. The base of the space is formed by the subclavian artery, lying on the suprapleural membrane. The apex of the space is the carotid (Chassaignac’s) tubercle on the transverse process of C6 vertebra (Figs 6.8 and 6.10).
The common carotid artery, medial to the internal jugular vein, lies deep to sternocleidomastoid immediately in front of the pyramidal space. Behind the artery and the carotid sheath, the space contains the inferior cervical sympathetic (or stellate) ganglion, with the vertebral artery and vein(s) in front of it. The inferior thyroid artery arches medially in a bold curve whose upper convexity lies in front of the apex of the pyramidal space (C6 level), with the sympathetic chain, usually the middle ganglion, in front of the artery. At a lower level, and further forward, the thoracic duct (or right lymphatic duct) makes a similar convexity behind the carotid sheath as it arches over the lung apex and subclavian artery to enter the confluence of the subclavian and internal jugular veins (Fig. 6.10).
The relationship of the scalenus anterior to the subclavian artery is used to descriptively divide the subclavian artery into three parts. The first part of the subclavian artery is medial to scalenus anterior. It arches over the suprapleural membrane and impresses a groove upon the apex of the lung. It has three branches. The vertebral artery is the first; this arises from the upper convexity of the subclavian and passes up to disappear, at the apex of the pyramidal space, into the foramen of the transverse process of C6 vertebra. The accompanying sympathetic nerve runs up behind the artery. Rarely this first part of the vertebral artery may initially enter the foramen of the transverse process of a higher vertebra than C6. A connecting loop between middle and inferior cervical ganglia passes in front of the subclavian artery and turns up behind it, forming the ansa subclavia. The recurrent laryngeal nerve recurves under the right subclavian artery, while the thoracic duct loops over the left artery. The thyrocervical trunk arises lateral to the vertebral artery from the upper surface of the subclavian. It divides immediately into superficial cervical, suprascapular and inferior thyroid arteries, which have already been noted. The proximal part of the superficial cervical is named transverse cervical artery when it gives off the dorsal scapular artery as a deep branch. The internal thoracic artery arises from the lower surface of the subclavian and passes downwards over the lung apex, crossed usually anteriorly by the phrenic nerve.
The vertebral vein emerges from the foramen in the transverse process of C6 vertebra and runs forward in front of the vertebral and subclavian arteries to empty into the brachiocephalic vein. It may be accompanied by a companion vein that passes through the foramen of the transverse process of C7 vertebra and passes behind the subclavian artery to the same destination.
Posterior relations
Scalenus anterior is separated from scalenus medius by the subclavian artery and the anterior rami of the lower cervical and first thoracic nerves. The second part of the subclavian artery lies behind scalenus anterior. Its only branch is the costocervical trunk. It passes back across the suprapleural membrane towards the neck of the first rib and there divides into a descending branch, the superior intercostal artery, which enters the thorax across the neck of the first rib, and an ascending branch, the deep cervical artery, which passes backwards between the transverse process of C7 vertebra and the neck of the first rib to run upwards behind the cervical transverse processes.
Lateral relations
The trunks of the brachial plexus and the third part of the subclavian artery emerge from the lateral border of scalenus anterior. They lie behind the prevertebral fascia on the floor of the posterior triangle (Fig. 6.10). The dorsal scapular usually arises from the third part. It runs laterally through the brachial plexus in front of scalenus medius and then deep to levator scapulae to take part in the scapular anastomosis (see p. 46). It is frequently replaced by the deep branch of the transverse cervical artery, and this branch then takes the name of dorsal scapular.
The surface marking of the subclavian artery in the neck is along a line arching upwards from the sternoclavicular joint to the middle of the clavicle and about 2cm above it.
Surgical approach. The artery can be exposed by dividing the clavicular head of sternocleidomastoid from the clavicle and then detaching scalenus anterior from the first rib, taking particular care not to damage the phrenic nerve.
Pressure on the subclavian artery and lowest root (T1) of the brachial plexus as they cross over a cervical rib or fibrous band, when present at the root of the neck, is described on page 422. Elevation of the first rib by scalenus anterior may also cause or aggravate such a thoracic outlet syndrome, and the muscle is usually divided close to its insertion when the syndrome is treated surgically.
Scalenus medius and scalenus posterior
Scalenus medius arises from the lateral ends of the transverse processes of atlas and axis and from the posterior tubercles of all the other cervical vertebrae and is inserted into the quadrangular area between the neck and subclavian groove of the first rib (see Fig. 4.34, p. 218).
Scalenus posterior is a small unimportant muscle that arises from the posterior tubercles of the lower cervical vertebrae, passes across the outer border of the first rib deep to the upper digitation of serratus anterior, and is inserted into the second rib.
Nerve supplies. Both muscles are supplied segmentally by the anterior rami of cervical nerves, scalenus medius by C3–8.
Actions. Scalenus medius, mainly a lateral flexor of the neck, can elevate the first rib as an accessory muscle of respiration.
Part five. Face
The face is the part of the front of the head between the ears and from the chin to the hairline (or where it ought to be).
Skin of the face
The skin of the face has numerous sweat and sebaceous glands. It varies in thickness and is very thin on the eyelids. The muscles underlying the skin of the face are attached to the dermis in places. Senile facial wrinkles lie at right angles to the line of pull of the underlying muscles (horizontal wrinkles on the brow, ‘crow’s foot’ wrinkles at the lateral canthus, vertical wrinkles on both lips). There is no deep fascia on the face.
Muscles of the face
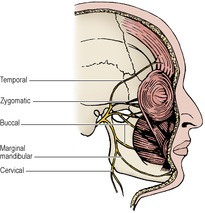
The muscles of ‘facial expression’ are developed from the mesoderm of the second pharyngeal arch, from which they migrate widely to their adult positions. They are supplied by the nerve of the second arch, the seventh cranial (facial) nerve. Functionally the muscles are differ-entiated to form groups around the orifices (Fig. 6.11). The orifices of orbit, nose and mouth are guarded by eyelids, nostrils and lips and there is a sphincter and an opposing dilator arrangement peculiar to each. The purpose of the facial muscles is to control these orifices. The varying expressions so produced on the face are side effects.
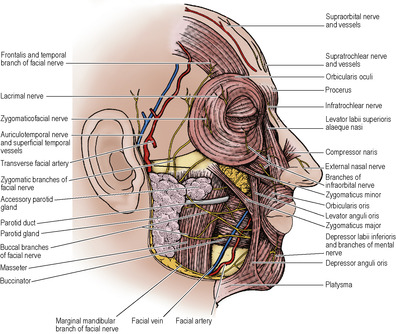 |
| Figure 6.11 |
Some of the muscles of the face participate in a superficial muscular aponeurotic system (SMAS). This is described on page 358.
Muscles of the eyelids
The palpebral fissure is surrounded by a sphincter, the orbicularis oculi, and has a dilator mechanism consisting of levator palpebrae superioris (considered with the orbital muscles, see p. 400) and occipitofrontalis which is part of the scalp (p. 355).
Orbicularis oculi has a palpebral part, confined to the lids, and an orbital part, extending beyond the bony orbital margins on to the face. The palpebral part consists of fibres that arise from the medial palpebral ligament (see p. 398), arch across both lids, anterior to the tarsal plates, and interdigitate laterally to form the lateral palpebral raphe. Fibres of a deeper lacrimal part are attached medially to the posterior lacrimal crest and lacrimal sac; laterally they join the upper and lower palpebral fibres. The orbital part, much the larger, arises from the nasal part of the frontal bone, the anterior lacrimal crest and the frontal process of the maxilla, whence the fibres circumscribe the orbital margin in a series of concentric loops.
Nerve supply. By temporal and zygomatic (mainly) branches of the facial nerve.
Action. Contraction of the palpebral fibres closes the lids gently without burying the eyelashes. Orbital and palpebral parts contracting together close the eyelids forcibly so that the eyelashes are buried and only their tips are visible. In normal closing of the eye, the lateral part of the upper lid comes down before the medial part, so helping to spread lacrimal secretion from the gland side (lateral) towards the nose.
Levator palpebrae superioris is the opponent of the upper palpebral fibres of orbicularis oculi; occipitofrontalis opposes the orbital part.
Muscles of the nostrils
The sphincter muscle of the nostril is the transverse part of nasalis (compressor naris), which forms an aponeurosis over the bridge of the nose with its fellow of the opposite side. Its opponent is the alar part of nasalis (dilator naris), which is inserted into the lateral part of the ala. Each arises from the maxilla. In addition, levator labii superioris alaeque nasi (see p. 352) and depressor septi contribute to widening the nostril. Depressor septi arises from the maxilla above the central incisor and is attached to the nasal septum. All these muscles are supplied by buccal branches of the facial nerve.
Muscles of the lips and cheeks
The sphincter is the orbicularis oris; the dilator mechanism consists of the remainder of the facial muscles, which radiate outwards from the lips like the spokes of a wheel.
Orbicularis oris consists of fibres proper to itself and fibres that are added to these from the dilators. The muscle is made up of four quadrants (upper, lower, right and left) each of which has a larger peripheral part and a smaller marginal part in the red zone of the lips. The bulk of the orbicularis muscle is formed of extrinsic fibres; most of these come from the buccinator. The fibres of buccinator converge towards the modiolus (see p. 352). At the modiolus they form a chiasma; the uppermost and lowermost fibres pass straight on into their respective lips, while the middle fibres decussate, the upper fibres of buccinator passing into the lower lip, the lower into the upper lip (Fig. 6.12).
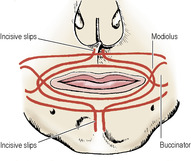 |
| Figure 6.12 |
Incisivus labii superioris and incisivus labii inferioris are attached to the incisive fossa of the maxilla and mandible, respectively, from where they arch laterally, interlacing with fibres of the peripheral part of orbicularis oris as they approach the modiolus. They are the deepest fibres in the lips and are attached to the mucous membrane.
Nerve supply. By buccal and marginal mandibular branches of the facial nerve. Damage to the latter branch (such as in the surgical approach to the submandibular gland) causes asymmetry of the mouth when speaking or smiling.
Action. Contraction of the orbicularis oris causes narrowing of the mouth, the lips becoming pursed up into the smallest possible circle (the whistling expression).
Buccinator has a bony origin from both jaws opposite the molar teeth, horizontally on the maxilla and from the oblique line of the mandible. Between the tuberosity of the maxilla and the hamulus at the bottom of the medial pterygoid plate (of the sphenoid), the muscle arises from a fibrous band (the pterygomaxillary ligament), above which the tendon of tensor palati hooks around the base of the hamulus (Fig. 6.13).
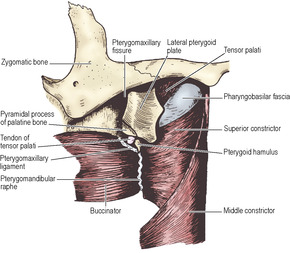 |
| Figure 6.13 |
From the tip of the hamulus the pterygomandibular raphe extends to the mandible just above the posterior end of the mylohyoid line; between them the lingual nerve is in contact with the mandible where the bone is often thinned by a shallow groove (Fig. 6.22). The buccinator arises from the whole length of the raphe, along which it interdigitates with the fibres of the superior constrictor (see p. 383). The muscle converges on the modiolus, where its fibres of origin from the raphe decussate; the maxillary and mandibular fibres pass medially without decussation into the upper and lower lips respectively. The muscle is pierced by the parotid duct opposite the third upper molar tooth. The duct also passes through the buccal fat pad which lies on the outer surface of buccinator and is particularly prominent in infants, giving them their chubby cheeks. Beneath the fat lie a few small molar glands; their ducts pierce the muscle to open on the mucous membrane of the cheek, which lines the muscle’s inner surface and to which muscle fibres are attached.
Nerve supply. By the buccal branches of the facial nerve. The buccal branch of the mandibular nerve supplies proprioceptive fibres.
Action. It is essentially an accessory muscle of mastica-tion, being indispensable to the return of the bolus from the cheek pouch to the grinding mill of the molars. It is, however, classified as a muscle of facial expression on account of being supplied by the facial nerve. When the cheeks are puffed out the muscle is relaxed, and the muscle contracts in forcible expulsion of air from the mouth, as in blowing a trumpet. (Buccinator is the Latin name for a trumpeter.)
Dilator muscles of the lips
Radiating from orbicularis oris like the spokes of a wheel is a series of dilator muscles, some inserted into the lips, some into the modiolus. All contracting together open the lips into the widest possible circle, an action that is usually accompanied by simultaneous opening of the jaws. Upper and lower lips have flat sheets of elevator and depressor muscles. Other muscles converge towards the angle of the mouth, where their decussating fibres form a knot of muscle with the chiasma in the buccinator fibres, bound together by fibrous tissue; this is termed the modiolus and is situated about 1cm lateral to the angle of the mouth, opposite the second upper premolar tooth. Its position and movements are of importance in prosthetic dentistry.
Levator labii superioris alaeque nasi arises from the frontal process of the maxilla and is inserted into the ala of the nose and the upper lip; it elevates both. Levator labii superioris arises from the inferior orbital margin and is inserted into the remainder of the upper lip, which it elevates. The muscle overlies the exit of the infraorbital nerve. From the canine fossa below the infraorbital foramen arises levator anguli oris; the infraorbital nerve lies sandwiched between it and the overlying levator labii superioris. The fibres of this muscle, deep to the superficial sheet of muscle, converge to the modiolus and pass through it to become superficial. They merge into the fibres of depressor anguli oris. Zygomaticus minor from the zygomaticomaxillary suture and zygomaticus major further out on the surface of the zygomatic bone converge to the modiolus. Risorius is a variable muscle that converges on the modiolus from the parotid fascia. All these muscles are supplied by buccal branches of the facial nerve.
Depressor anguli oris arises from the mandible below the mental foramen. It lies superficial but its fibres pass through the modiolus to the deeper stratum. Depressor labii inferioris arises from the mandible in front of the mental foramen, deep to the former muscle; its fibres are inserted into the lower lip. Mentalis is a muscle that arises near the midline of the mandible. Its fibres pass downwards to reach the skin. It is an elevator of the skin of the chin (which it sometimes dimples) and its contraction may disturb a lower denture. These muscles are supplied by the marginal mandibular branch of the facial nerve.
Nerve supply of face muscles
The supply from the facial nerve to the muscles described above is motor. Proprioceptive impulses from the facial muscles are conveyed centrally by the trigeminal nerve, whose cutaneous branches connect freely with branches of the facial nerve.
The facial nerve emerges from the base of the skull through the stylomastoid foramen, near the origin of the posterior belly of digastric. It immediately gives off the posterior auricular nerve which passes upwards behind the ear to supply auricularis posterior and the occipital belly of occipitofrontalis. A muscular branch is next given off which divides to supply the posterior belly of digastric and stylohyoid. The nerve now approaches the posteromedial surface of the parotid gland. Just before entering or within the gland it divides into an upper temporofacial and a lower cervicofacial division. Within the substance of the parotid gland each divides and rejoins to divide again and finally emerge from the parotid gland in five main groups of branches (Fig. 6.14). This plexiform arrangement, the pes anserinus, lies in the gland superficial to the retromandibular vein and the external carotid artery.
The temporal branches emerge from the upper border of the gland, cross the zygomatic arch, and supply auricularis anterior and superior, and part of frontalis. They are only important for wrinkling the forehead. (A branch is also termed a frontal branch in some texts.)
The zygomatic branches cross the zygomatic arch and zygomatic bone, lying directly on the periosteum. They may be damaged in fractures or operations in this region. These branches supply orbicularis oculi. Paralysis of this muscle prevents blinking and the precorneal film of tears is no longer spread. The dry cornea easily ulcerates. The resultant scar impairs vision and this is the most serious consequence of impaired facial nerve function.
The buccal branches run forwards close to the parotid duct, often one above and one below the duct. They supply buccinator and the muscle fibres of the nose and the upper lip. Paralysis of the buccinator prevents emptying of the cheek pouch; the bolus lodges there and cannot be returned to the molar teeth. Chewing has to be performed on the other side.
The marginal mandibular branch is frequently single and runs forwards above, along, or below the lower border of the mandible. From below the mandible it crosses the inferior border of the bone to reach the face just beyond the anterior border of the masseter muscle, passing superficial to the facial artery and vein. A small lymph node lies here (Fig. 6.63). The nerve is in danger when an incision is made at or near the lower border of the mandible. This nerve does not communicate with a buccal branch and damage to the nerve invariably causes detectable paralysis of the depressors of the lower lip and mouth angle, there being no alternate pathway for motor fibres to these muscles.
The cervical branch passes downwards from the lower border of the parotid gland and supplies platysma.
The details of the pattern of branching of the facial nerve differs in different individuals and even on the two sides of the face of the same person.
Sensory nerve supply of the face
The trigeminal nerve has three divisions (officially called branches): ophthalmic, maxillary and mandibular. The skin of the face is supplied in three zones by the branches of the three divisions of the trigeminal nerve (Fig. 6.15A). These zones meet at the lateral margins of the eyelids and the angle of the mouth, and the junctional lines of the zones curve outwards and upwards from there. The pattern of a facial haemangioma (port wine stain, as in Sturge–Weber syndrome), and the distribution of the vesicles when herpes zoster affects the trigeminal ganglion, is often in accordance with this arrangement of the sensory supply of facial skin. However, the spatial representation of the face in the spinal nucleus of the trigeminal nerve in the brainstem, particularly with regard to pain sensation, is probably different and more akin to an ‘onion skin’ pattern, with fibres from the central area of the face reaching the highest (cranial) part of the nucleus and fibres from the more posterior part of the face passing to progressively lower (caudal) levels of the nucleus (Fig. 6.15B).
The great auricular nerve supplies the skin over the parotid gland and part of the auricle of the ear (see p. 334); the fibres reach the C2 segment of the spinal cord.
Ophthalmic nerve
Five cutaneous branches:
The lacrimal nerve supplies a small area of skin over the lateral part of the upper lid.
A third of the way lateral to the medial end of the upper margin of the orbit, the supraorbital nerve indents the bone into a notch or a foramen. The nerve passes up, breaking into several branches which radiate out and supply the forehead and scalp up to the vertex.
The smaller supratrochlear nerve passes up on the medial side of the supraorbital nerve to supply the middle of the forehead up to the hairline.
The infratrochlear nerve supplies skin on the medial part of the upper lid and, passing above the medial palpebral ligament, descends along the side of the external nose, supplying skin over the bridge of the nose.
These four branches of the ophthalmic nerve also supply upper lid conjunctiva.
The external nasal nerve supplies the middle of the external nose down to the tip. It emerges between the nasal bone and the upper nasal cartilage.
The supraorbital and supratrochlear nerves are branches of the frontal nerve (see p. 402). The infratrochlear and external nasal nerves are derived from the nasociliary (see p. 403), the former directly and the latter via the anterior ethmoidal branch; when these nerves are involved in herpes zoster infection, the cornea (supplied by the ciliary branches of the nasociliary) may also become affected and lead to dangerous corneal ulceration.
Maxillary nerve
Three cutaneous branches:
The infraorbital nerve emerges through its foramen and lies between levator labii superioris and the deeper placed levator anguli oris. It is a large nerve that immediately breaks up into a tuft of branches; these radiate away from the foramen to supply the lower eyelid (including conjunctiva), cheek, nose, upper lip and labial gum.
The zygomaticofacial nerve emerges from a foramen on the outer surface of the zygomatic bone; its branches supply the overlying skin.
The zygomaticotemporal nerve emerges in the temporal fossa through a foramen in the temporal (posterior) surface of the zygomatic bone. It supplies a small area of temporal skin.
Mandibular nerve
Three cutaneous branches:
The auriculotemporal nerve passes around the neck of the mandible and ascends over the posterior root of the zygomatic arch behind the superficial temporal vessels. The auricular part of the nerve supplies the external acoustic meatus, surface of the tympanic membrane and skin of the auricle above this level. The temporal part supplies the hairy skin over the temple.
The buccal nerve gives off cutaneous twigs before it pierces the buccinator muscle to supply oral mucous membrane. They supply a small area over the cheek just below the zygomatic bone, between the areas of the infraorbital nerve and the great auricular nerve (see p. 334).
The mental nerve is a cutaneous branch of the inferior alveolar nerve. Like the infraorbital nerve it breaks up into a tuft of branches; these radiate away from the mental foramen to supply the skin and mucous membrane of the lower lip and labial gum from the midline to about the second premolar tooth.
Blood supply of the face
The facial artery hooks upwards over the inferior border of the mandible at the anterior border of the masseter muscle. It pursues a tortuous course towards the medial angle of the eye, lying on the buccinator deep to the sheet of dilator muscles that radiate out from the lips. Its labial branches are sizeable. Each superior and inferior labial artery runs across the lip beneath the red margin and anastomoses end to end with the corresponding artery of the opposite side. The larger superior labial artery gives a septal branch to the nasal septum. The transverse facial artery, a branch of the superficial temporal artery, runs across the cheek just above the parotid duct. The forehead is supplied from the orbit by the supraorbital and supratrochlear branches of the ophthalmic artery. The bigger supraorbital artery anastomoses with the superficial temporal artery, establishing communication between internal and external carotid systems. The dorsal nasal artery, a small terminal branch of the ophthalmic artery, supplies skin at the root of the nose.
The venous return from the face is normally entirely superficial. From the forehead the supraorbital and supratrochlear veins pass to the medial canthus, where they unite to form the angular vein. This becomes the facial vein which pursues a straight course behind the tortuous facial artery to a point just below the border of the mandible. Here in the neck it pierces the investing layer of the deep fascia and is joined by the anterior branch of the retromandibular vein, and sometimes by the superior thyroid vein. Blood from the temple is collected into the tributaries of the superficial temporal vein. The latter is joined by the maxillary vein from the pterygoid plexus to form the retromandibular vein. This passes downwards in the substance of the parotid gland and on emerging from its lower border divides into anterior and posterior branches. The anterior branch joins the facial vein which empties into the internal jugular. The posterior branch pierces the investing layer of deep cervical fascia and is joined by the posterior auricular vein to form the external jugular vein. This courses down in the subcutaneous tissue over sternocleidomastoid and pierces the investing layer of deep cervical fascia to enter the posterior triangle and empty into the subclavian vein. It has valves about 4cm above the clavicle and at its termination.
Deep venous anastomoses
At the medial angle of the eyelids there is a communication between the angular vein and the ophthalmic veins, which drain directly into the cavernous sinus. Blood from the forehead normally flows via the facial vein; if the latter is blocked by thrombosis, blood above the obstruction will flow through the orbit into the cavernous sinus. Hence the ‘danger area’ of infection of the upper lip and nearby cheek. A further communication is the deep facial vein. This passes backwards from the facial vein, between the masseter and buccinator muscles, to the pterygoid plexus. The plexus connects with the cavernous sinus by emissary veins that pass through the foramen ovale and the foramen lacerum. The danger area of the face lies between the angular and deep facial veins.
Lymph drainage of the face
The face drains into three superficial groups of nodes (see p. 410) from three wedge-shaped blocks of tissue. Centrally a small triangular area that includes the chin and tip of the tongue drains into submental nodes. A wedge of tissue above this, which extends laterally as far as the facial vessels, drains to submandibular nodes; this wedge extends from central forehead and frontal sinuses through the anterior half of the nose and maxillary sinuses to the upper lip and lower part of the face, and includes the tongue and the floor of the mouth. Beyond this wedge, forehead, temple, orbital contents and cheek drain to preauricular (parotid) nodes. Eventually all lymph from the face reaches deep cervical nodes.
Part six. Scalp
The scalp extends from the supraorbital margins anteriorly to the highest nuchal lines at the back of the skull and down to the ears and zygomatic arches at the sides. The forehead, from eyebrows to hairline (or where it should be), is common to the face and scalp. The composition of the scalp is traditionally recalled from the five letters of the words that indicate its five layers: Skin; Connective tissue; Aponeurosis with muscle at the front and back; Loose areolar tissue; and Pericranium.
The skin of the scalp is the thickest in the body and is thickest of all in the occipital region. Apart from being usually the hairiest part of the body it also contains a high concentration of sebaceous glands. Many of the fibres of the scalp muscle are inserted into it. Elsewhere it is firmly attached by dense connective tissue (the second layer) to the underlying muscle and aponeurosis. The vessels and nerves run within this firm tissue which unites the first and third layers.
Occipitofrontalis consists of occipitalis and frontalis muscular parts with an intervening epicranial aponeurosis (galea aponeurotica) into which they are inserted at the back and front respectively. Occipitalis arises from the highest nuchal line and passes forwards into the aponeurosis which lies over the top of the skull. The muscle bellies are separated across the midline by the aponeurosis which extends backwards to be attached to the external occipital protuberance and the most medial part of the highest nuchal line. Laterally the aponeurosis blends with the temporoparietal fascia (superficial temporal fascia) and comes down over the deep temporal fascia (see p. 357) to the zygomatic arch. Frontalis arises from the front of the aponeurosis and passes forwards to become attached to the upper part of orbicularis oculi and the overlying skin of the eyebrow. It has no attachment to the skull. The right and left frontalis muscles meet in the midline. The midline fibres blend with procerus, a small muscle that arises from the nasal bone and cartilage and inserts into the skin of the lower forehead; its contraction produces transverse wrinkles over the bridge of the nose.
Nerve supply. By the facial nerve; the posterior auricular branch to occipitalis, and temporal branches to frontalis.
Action. While occipitalis can pull the scalp back in certain individuals, usually it merely anchors the aponeurosis while frontalis elevates the eyebrows and produces wrinkles in the skin of the forehead.
Beneath the muscles and aponeurosis is a small amount of loose areolar tissue providing a plane above which the rest of the scalp can be moved and through which avulsion can occur (scalping). Through this plane a flap of the overlying scalp can be rotated on a vascular pedicle as a surgical procedure. This subaponeurotic space extends down beneath orbicularis oculi into the eyelids. Bleeding anywhere beneath the aponeurosis may appear as a ‘black eye’ by the blood tracking down through the space.
The pericranium is the periosteum of the vault of the skull. This is rather loosely attached to the bone and is easily stripped up by a subperiosteal haematoma. Such a haematoma outlines the bone concerned, since the pericranium is very firmly attached at the sutures at the margins of the bone.
Blood supply
The arteries of the scalp are derived from the external carotid artery by the occipital, posterior auricular and superficial temporal branches, and from the internal carotid artery by the supraorbital and supratrochlear branches. All these arteries anastomose very freely with each other. The arterial walls are attached to the dense connective tissue of the second layer of the scalp and tend to be held open and bleed profusely when cut. Scalping does not cause necrosis of the bones of the vault, most of whose blood comes from the middle meningeal artery.
The occipital artery emerges from the apex of the posterior triangle and runs with the greater occipital nerve to supply the back of the scalp up to the vertex. The smaller posterior auricular artery runs with the lesser occipital nerve to supply the scalp behind the ear.
The superficial temporal artery is a terminal branch of the external carotid. Running up behind the temporomandibular joint and in front of the ear and the auriculo-temporal nerve, it crosses the zygomatic arch, where its pulsation can be felt, and branches out widely into the skin that overlies the temporal fossa. One branch, the middle temporal artery, pierces the fascia, supplies temporalis and anastomoses with the deep temporal branches of the maxillary artery.
The supraorbital and supratrochlear arteries (from the ophthalmic) run with the corresponding nerves. The supraorbital is the larger and supplies the front of the scalp up to the vertex. Its anastomosis with the superficial temporal artery connects the internal and external carotid systems.
The veins of the scalp run back with the arteries. In forehead, temple and occipital regions they receive diploic veins from frontal, parietal and occipital bones.
The supraorbital and supratrochlear veins drain by the angular vein into the facial vein. The superficial temporal veins run into the retromandibular vein, and occipital veins reach the plexus around the suboccipital muscles which drains into the vertebral vein. The posterior auricular vein drains the scalp behind the ear to the external jugular vein; it also receives the mastoid emissary vein from the sigmoid sinus. Spread of infection to this emissary vein from mastoid air cells can be dangerous or fatal, from retrograde thrombosis of cerebellar and medullary veins. At the vertex a parietal emissary vein on either side of the midline connects scalp veins with the superior sagittal sinus.
Lymph drainage
There are no lymph nodes within the scalp; lymphatic channels from the posterior half of the scalp drain to occipital and mastoid nodes, and from the anterior half to preauricular (parotid) nodes. The lymph eventually reaches the nodes of the deep cervical chain.
Nerve supply
The main sensory nerves run with the arteries. Posteriorly the greater occipital and third occipital nerves (posterior rami of C2 and C3 respectively) extend to the vertex and the posterior scalp respectively. The lesser occipital (anterior ramus of C2) supplies skin behind the ear. The temple is supplied by the auriculotemporal and the zygomaticotemporal nerves, and the forehead and front of the scalp by the supratrochlear and supraorbital nerves.
Temporal fossa and zygomatic arch
The temporal fossa is the area bounded by the temporal lines above and the zygomatic arch below (see Fig. 8.1, p. 525). Its roof (lateral wall) is the temporalis fascia and its floor (medial wall) is the part of the side of the skull that includes the pterion, where the frontal, the parietal and the squamous part of the temporal bones articulate with the greater wing of the sphenoid. (It lies on the course of the anterior branch of the middle meningeal artery and marks the position of the stem of the lateral cerebral fissure.) The zygomatic processes of the frontal bone, the zygomatic bone, and the maxilla are in the anterior wall. The fossa is filled by the temporalis muscle which arises from the floor and the overlying fascia. Deep to the arch, at the level of the infratemporal crest of the greater wing of the sphenoid (Fig. 6.19), the fossa becomes continuous with the lateral part of the infratemporal fossa (see p. 361).
The zygomatic arch is formed by processes of the squamous temporal and zygomatic bones, which meet at a suture sloping downwards and backwards. The arch is completed anteriorly by the zygomatic process of the maxilla.
Nerves crossing the arch are vulnerable in incisions or in fractures. The auriculotemporal nerve crosses well back, just in front of the ear, and temporal and zygomatic branches of the facial nerve cross the arch, to reach the frontalis and orbicularis oculi muscles.
The temporal fascia (deep temporal fascia) is attached to the superior temporal line and passes down to the upper border of the zygomatic arch. Above the arch it splits into two layers, one attached to the lateral and the other to the medial margin of the upper border of the arch. The space between these two layers is occupied by fat, which is traversed by a branch of the superficial temporal artery and the zygomaticotemporal branch of the maxillary nerve. The temporal and zygomatic branches of the facial nerve, the superficial temporal vessels and the auriculotemporal nerve lie in or just deep to the overlying temporoparietal fascia (superficial temporal fascia, see p. 356). In surgical procedures in this region, the temporal fascia is divided at a high level and the space between its two layers entered at a lower level via the deep layer to access the zygomatic arch, thereby safeguarding the overlying neurovascular structures.
Temporalis
This muscle (one of the muscles of mastication) arises from the temporal fossa over the whole area between the inferior temporal line and the infratemporal crest, and from the deep surface of the temporalis fascia. The most anterior fibres are vertical and the most posterior are horizontal, turning downwards in front of the temporomandibular joint. The fan-shaped muscle converges towards the coronoid process of the mandible, becomes tendinous, and is inserted into a bevelled surface on the medial aspect of the coronoid process adjacent to its posterior border, apex and anterior border. From the anterior part of this insertion, two tendinous bands extend downwards and forwards to the posterior end of the alveolar process enclosing the retromolar fossa between them. The deep, larger tendinous band is attached to a slight (temporal) crest on the mandible, and is palpable through the vestibule of the mouth; a useful guide when performing an inferior alveolar nerve block.
The blood supply of the muscle is derived from the temporal branches of the maxillary and superficial temporal arteries.
Nerve supply. Two or three deep temporal branches of the mandibular nerve enter the deep surface of the muscle.
Action. Temporalis elevates the mandible when the open mouth is closed, and it retracts the protruded mandible.
Part seven. Parotid region
The part of the face in front of the ear and below the zygomatic arch is the parotid region. The principal features are the parotid gland and the masseter muscle.
Masseter
This quadrilateral muscle of mastication arises from the lower border of the zygomatic arch and is inserted into almost the whole of the lateral surface of the mandibular ramus. Most of its fibres slope downwards and backwards at 45°. The posteriormost fibres arise from the deep surface of the arch and pass vertically downwards to be inserted into the upper part of the ramus; these fibres blend with the lower fibres of temporalis. The upper anterior part of the muscle is covered by an aponeurosis on which the parotid duct and the accessory parotid gland lie.
The muscle receives blood supply from branches of the facial artery, maxillary artery and superficial temporal artery, particularly its transverse facial artery. These vessels form an anastomotic network on the surface of and within the muscle.
Nerve supply. By the masseteric branch of the mandibular nerve, which passes through the mandibular notch to enter the deep surface of the gland.
Action. Masseter elevates and draws forwards the angle of the mandible when the jaws are approximated. The deep fibres assist temporalis in retracting the mandible.
Parotid gland
The parotid gland is the largest of the major salivary glands, i.e. glands that drain saliva into the mouth through ducts. It is a mainly serous gland, with only a few scattered mucous acini. It is a large, irregular, lobulated gland which extends from the zygomatic arch to the upper part of the neck, where it overlaps the posterior belly of digastric and the anterior border of sternocleidomastoid (Fig. 6.16). Anteriorly the gland overlaps masseter and a small, usually detached accessory parotid lies above the parotid duct on the aponeurotic part of masseter. The gland extends below the external acoustic meatus posteriorly onto the mastoid process. In transverse section the gland is wedge-shaped, occupying the gap between the ramus of the mandible and the mastoid and styloid processes of the temporal bone, and reaching close to the lateral wall of the oropharynx; hence the need to look at the region of the fauces when examining a patient with a parotid mass.
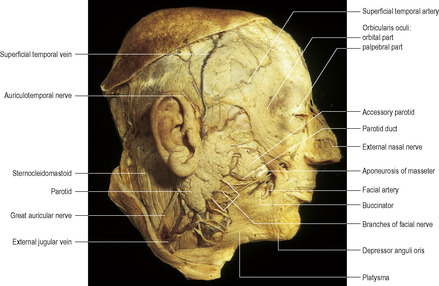 |
| Figure 6.16 |
The lateral (superficial) surface of the gland is covered by skin and superficial fascia. The investing layer of deep cervical fascia splits to envelope the gland and the inner leaf passes up to the base of the skull (see p. 330). The outer leaf extends superiorly as the parotidomasseteric fascia and reaches up to the zygomatic arch. On the gland, the fascia tends to be termed the parotid capsule and, more anteriorly, the masseteric fascia. Overlying the gland is a superficial muscular aponeurotic system (SMAS), which is continuous above with the temporoparietal fascia (see p. 356) and frontalis, below with platysma and over the gland with risorius. SMAS is adherent to the parotidomasseteric fascia in the pretragal area and becomes separate from it as the fascia enters the cheek where it overlies the parotid duct, facial nerve branches and buccal fat pad. The nerve branches penetrate the parotidomasseteric fascia as they proceed peripherally to inervate overlying facial muscles. The great auricular nerve supplies the fascia superficial and deep to the parotid gland, and transmits the pain caused by stretching of the fascial envelope when acute enlargement of the gland occurs as in mumps.
The anteromedial surface is grooved by the posterior border of the mandibular ramus, and is related to the masseter and medial pterygoid muscles which are attached to the ramus. The gland is also wrapped around the capsule of the temporomandibular joint. The anterior edge of this surface meets the lateral surface over, as well as below, the masseter forming the irregularly convex anterior border of the gland. The parotid duct and the facial nerve branches emerge from the anteromedial surface and run forwards deep to the anterior border. The terminal branches of the external carotid artery (superficial temporal and maxillary) leave this surface further back.
The posteromedial surface is in contact with the mastoid process with its attached sternocleidomastoid and posterior belly of digastric muscles. More medially, the styloid process and its attached muscles (stylohoid, stylopharyngeus and styloglossus) separate the gland from the carotid sheath and its contained internal jugular vein and internal carotid artery. The external carotid artery enters the gland through the lower part of this surface. The facial nerve trunk, or its temporofacial and cervicofacial divisions, enter the gland between the mastoid and styloid processes.
Within the gland the branches of the facial nerve run in different directions corresponding with their destinations, i.e. scalp, eyelids, mid-face, lower face and neck, and they do so in different (superficial to deep) planes. There is no specific, developmentally determined plane in which the facial nerve branches pass between superficial and deep lobes of the gland; the parotid is an integral gland, not divided into lobes. Within the gland the nerve branches communicate with each other, forming a plexiform arrangement that lies superficial to the retromandibular vein, which in turn is superficial to the external carotid artery. The retromandibular vein is formed within the parotid by the confluence of the superficial temporal and maxillary veins. The retromandibular vein emerges from the lower part (pole) of the gland and divides into an anterior branch which joins the facial vein and a posterior branch which joins the posterior auricular vein to form the external jugular vein; however, the division may occur within the gland and the two branches emerge from the lower pole. Lymph nodes of the preauricular (parotid) group lie on or deep to the fascial capsule of the parotid, as well as within the gland.
The parotid duct (of Stensen), about 5cm long, passes forwards across the masseter and turns around its anterior border to pass through the buccal fat pad and pierce the buccinator. It lies on the middle third of a line between the intertragic notch of the auricle and the midpoint of the philtrum (the vertical midline groove between the nasal septum and the upper lip) and is palpable on the clenched masseter muscle. The duct opens on the mucous membrane of the cheek opposite the second upper molar tooth (Fig. 6.17); it pierces the buccinator further back and runs forwards beneath the mucous membrane to its orifice. When intraoral pressure is raised this submucous part of the duct is compressed between the buccinator and the mucous membrane, preventing inflation of the gland.
An accessory parotid gland usually lies on the masseter between the duct and the zygomatic arch. Several small ducts open from it into the parotid duct. It and the duct lie on the aponeurotic part of the surface of the masseter muscle.
Blood supply
Branches from the external carotid artery supply the gland. Venous return is to the retromandibular vein.
Lymph drainage
Lymph drains to the preauricular (parotid) nodes and thence to nodes of the upper group of deep cervical nodes.
Nerve supply
Secretomotor fibres arise from cell bodies in the otic ganglion (see p. 22) and reach the gland by ‘hitch-hiking’ along the auriculotemporal nerve. As it passes backwards along the mandibular neck and ascends behind the temporomandibular joint, the auriculotemporal nerve is in contact with the anteromedial surface of the gland, which is penetrated by filaments from the nerve. The preganglionic fibres arise from cell bodies in the inferior salivary nucleus in the medulla, and travel by way of the glossopharyngeal nerve, its tympanic branch, the tympanic plexus and the lesser petrosal nerve to the otic ganglion. Sympathetic (vasoconstrictor) fibres reach the gland from the superior cervical ganglion by way of the plexus on the external carotid and middle meningeal arteries.
Development
A groove that appears in the ectoderm of the mouth pit (stomodeum, see p. 28) becomes converted into a tunnel, from the blind end of which cells proliferate to form the gland.
Surgical approach
The most common neoplasm of the parotid gland is a pleomorphic adenoma (mixed parotid tumour) which requires removal with a margin of normal parotid tissue, conserving the facial nerve and its branches. On account of the wide extent of the gland, it is approached through an S-shaped incision made from in front of the ear, backwards to the mastoid process and then downwards and forwards below the angle of the mandible. The gland is retracted forwards from the sternocleidomastoid to expose the posterior belly of digastric and stylohyoid and the cartilage of the external meatus. The facial nerve is approached along a plane in front of the anterior margin of the cartilage. The trunk emerges from the stylomastoid foramen, just deep to the junction of the cartilaginous and bony parts of the external meatus, about 1cm above and medial to the upper end of the posterior belly of digastric (Fig. 6.18). The cartilage in this region has a slight arrow-headed projection that points downwards to the emerging nerve trunk. The stylomastoid branch of the posterior auricular artery is superficial to the facial nerve and is a guide to its proximity. Once identified, the facial nerve is followed forwards into the gland and the required amount of parotid tissue removed with preservation of facial nerve branches. An alternative approach to facial nerve conservation is to first find a facial nerve branch as it leaves the gland and to follow this in a centripetal manner back to the trunk and other branches. The marginal mandibular branch may be identified as it lies superficial to the retromandibular vein or its anterior branch, aided by the colour contrast between the white nerve and the dark vein; occasionally this branch may pass behind the vein. Alternatively, the cervical branch may be followed up from its communication with the ascending branch of the transverse cervical nerve.
Part eight. Infratemporal region
Infratemporal fossa
This is a space lying beneath the base of the skull between the side wall of the pharynx and the ramus of the mandible. It is also referred to as the parapharyngeal or lateral pharyngeal space.
Boundaries
Its medial boundary is the lateral surface of the lateral pterygoid plate with, behind it, the tensor palati muscle and the superior constrictor. In front of the lateral pterygoid plate, between it and the maxilla, is the pterygo-maxillary fissure through which the infratemporal fossa communicates with the pterygopalatine fossa (see p. 369). The lateral wall is the ramus of the mandible and its coronoid process. The anterior wall is the posterior surface of the maxilla, at the upper margin of which is a gap between it and the greater wing of sphenoid—the inferior orbital fissure. The roof of the fossa is formed medially by the infratemporal surface of the greater wing of the sphenoid (perforated by the foramen ovale and foramen spinosum) and the adjacent squamous part of the temporal bone in front of the articular eminence (Fig. 6.19). This infratemporal surface of the sphenoid is bounded laterally by the infratemporal crest, where the bone takes an almost right-angled turn upwards to become part of the side of the skull, deep to the zygomatic arch and part of the temporal fossa. Thus the roof of the infratemporal fossa lateral to the infratemporal crest is not bony, but is the space deep to the zygomatic arch where the temporal and infratemporal fossae communicate. The posterior boundary is the styloid process with the carotid sheath behind it.
Contents
The fossa contains the deep part of the parotid gland, the medial and lateral pterygoid muscles, the insertion of temporalis into the coronoid process, the maxillary artery and its branches, the pterygoid venous plexus, the mandibular nerve and its branches together with the otic ganglion, the chorda tympani, and the posterior superior alveolar branches of the maxillary nerve.
Lateral pterygoid
This muscle arises by two heads: the upper from the roof of the infratemporal fossa and the lower from the lateral surface of the lateral pterygoid plate. The two heads, lying edge to edge, converge and fuse into a short thick tendon that is inserted into the pterygoid fovea on the front of the neck of the mandible. The upper fibres of the tendon pass back into the capsule and the articular disc of the temporomandibular joint (Fig. 6.20).
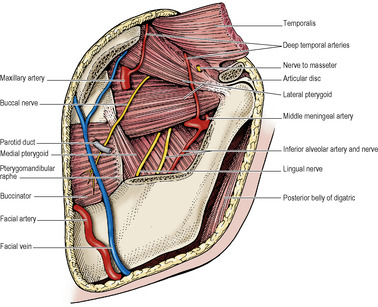 |
| Figure 6.20 |
Nerve supply. By a branch from the anterior division of the mandibular nerve.
Action. When the muscle contracts it draws condyle and disc forwards from the mandibular fossa down the slope of the articular eminence (Fig. 6.35). It is indis-pensable to active opening of the mouth. It participates with medial pterygoid in chewing movements.
Medial pterygoid
This muscle also arises by two heads. The larger deep head arises from the medial (deep) surface of the lateral pterygoid plate. The muscle diverges down from the lateral pterygoid muscle at nearly a right angle from their common origin on either side of the lateral pterygoid plate (Fig. 6.20). A small slip of muscle, the superficial head, arises from the tuberosity of the maxilla and the pyramidal process of the palatine bone which insinuates itself between the tuberosity and the lower end of the lateral pterygoid plate (Fig. 6.13). Passing over the lower margin of the lateral pterygoid muscle, the superficial head fuses with the main muscle mass. In this way the two heads, very unequal in size, embrace the lower edge of the lateral pterygoid. The muscle passes down and back at 45°, and laterally to reach the angle of the mandible. It is inserted into the rough area on the medial surface of the angle as far as the groove for the mylohyoid vessels and nerve (see Fig. 8.5B, p. 510). The muscle is characterized by tendinous intersections on its surface, which account for the roughness of the area of insertion on the mandible.
Nerve supply. By a branch from the main trunk of the mandibular nerve (Fig. 6.21).
Action. The pull of the muscle on the angle of the mandible is upwards, forwards and medially (i.e. it closes the mouth) and it moves the mandible towards the opposite side in chewing. Contracting with its opposite fellow and the two lateral pterygoids, it helps to protrude the mandible.
Maxillary artery
The maxillary artery is, with the superficial temporal artery, a terminal division of the external carotid. It enters the infratemporal fossa by passing forwards deep to the neck of the mandible, between the neck and the sphenomandibular ligament. Here the auriculotemporal nerve lies above it (Fig. 6.21), and the maxillary vein below it. It usually runs deep (sometimes superficial) to the lower head and passes forward and upward between the two heads of the lateral pterygoid muscle (Fig. 6.20). It then passes deeply into the pterygomaxillary fissure and so into the pterygopalatine fossa.
It is described conventionally in three parts, before, on and beyond the lateral pterygoid muscle and this is useful, since five branches come from each part. From first and third parts the five branches all enter foramina in bones, from the second part the branches are mainly muscular.
The five branches from the first part are the inferior alveolar, middle meningeal, accessory meningeal and two branches to the ear.
The inferior alveolar artery passes downwards and forwards (vein behind it) towards the inferior alveolar nerve and all three enter the mandibular foramen. It passes forwards in the mandible, supplying the pulps of the mandibular molar and premolar teeth and the body of the mandible. Its mental branch emerges from the mental foramen and supplies the nearby lip and skin.
The middle meningeal artery passes vertically upwards to the foramen spinosum. It is embraced by the two roots of the auriculotemporal nerve (Fig. 6.21). Its course and distribution are described on page 442. From the sympathetic plexus on the artery a branch enters the otic ganglion.
The accessory meningeal artery passes upwards through the foramen ovale and supplies the dura mater of the floor of the middle fossa and of the trigeminal (Meckel’s) cave. It is the chief source of blood supply to the trigeminal ganglion.
The remaining two arteries pass upwards to enter the ear and run superficial and deep to the tympanic membrane. The deep auricular artery is the more superficial of the two and supplies the external acoustic meatus, passing between the cartilage and bone. The deeper is the anterior tympanic artery which passes through the petrotympanic fissure to the middle ear to join the circular anastomosis around the tympanic membrane.
The second part of the maxillary artery gives off branches to the pterygoid muscles and masseter, and deep temporal branches to temporalis which ascend between the muscle and the temporal fossa. A small branch accompanies the buccal nerve.
The third part of the maxillary artery, in the pterygopalatine fossa, gives five branches (see below) which accompany branches of the maxillary nerve and the pterygopalatine ganglion (see p. 370). The artery then passes forwards, with the maxillary nerve, through the inferior orbital fissure into the orbit as the small infraorbital artery, which continues along the floor of the orbit and infraorbital canal to emerge with the infraorbital nerve on the face; its middle (occasional) and anterior superior alveolar branches supply maxillary incisor and canine teeth.
The sphenopalatine artery passes through the sphenopalatine foramen to enter the nasal cavity as its main artery of supply (see p. 374). The posterior superior alveolar artery gives branches that accompany the corresponding nerves through foramina in the posterior wall of the maxilla. The greater palatine artery gives off lesser palatine branches to the soft palate and passes through the greater palatine foramen to supply the hard palate (see p. 380). The very small pharyngeal artery enters the palatovaginal canal, and the artery of the pterygoid canal runs into its own canal.
The posterior superior alveolar nerve is a branch of the maxillary, given off in the pterygopalatine fossa and soon dividing into two or three branches which pierce the posterior wall of the maxilla separately. They are distributed to the molar teeth and the mucous membrane of the maxillary sinus. Another branch does not pierce the bone but runs along the alveolar margin of the maxilla as far forward as the first molar tooth, to supply the gingiva of the vestibule alongside the molar teeth. The posterior superior alveolar nerves can be blocked here by an injection through the vestibule of the mouth; on account of the proximity of the posterior superior alveolar vessels and the pterygoid venous plexus, a haematoma of some size may be a complication.
The pterygoid plexus is a network of very small veins that lie around and within the lateral pterygoid muscle. The veins draining into the pterygoid plexus correspond with the branches of the maxillary artery, but they do not return all the arterial blood, much of which returns from the periphery of the area by other routes (facial veins, pharyngeal veins, diploic veins). On the other hand the pterygoid plexus receives the drainage of the inferior ophthalmic vein (see p. 403), via the inferior orbital fissure, and the deep facial vein. The pterygoid plexus drains into a short maxillary vein which lies deep to the neck of the mandible. It runs back to join the superficial temporal vein and form the retromandibular vein. The plexus is valved and acts as a ‘peripheral heart’, aiding venous return by the pumping action of the lateral pterygoid muscle. Emissary veins connect the pterygoid plexus with the cavernous sinus through the foramen ovale and the foramen lacerum.
The sphenomandibular ligament is a flat band of tough fibrous tissue extending from a narrow attachment on the spine of the sphenoid. It broadens as it passes downwards to be attached to the lingula and inferior margin of the mandibular foramen (see Fig. 8.5B, p. 510). It is derived from the perichondrium of Meckel’s cartilage (see Fig. 1.20, p. 25). Between it and the neck of the mandible pass the auriculotemporal nerve and the maxillary artery and vein. Between it and the ramus of the mandible the inferior alveolar vessels and nerve converge to the mandibular foramen. Any remaining space between the ligament and the mandible is occupied by parotid gland tissue. The ligament is pierced by the mylohyoid nerve, a branch from the inferior alveolar nerve, and the accompanying small mylohyoid artery and vein.
Mandibular nerve
The mandibular branch from the trigeminal ganglion lies in the dura mater of the middle cranial fossa lateral to the cavernous sinus. With the motor root of the trigeminal nerve it enters the foramen ovale, where the two join and emerge as the mandibular nerve (like spinal nerve roots in intervertebral foramina). The nerve lies deep to the upper (infratemporal) head of the lateral pterygoid, between it and the tensor palati muscle, with the otic ganglion applied to the deep surface of the nerve (Fig. 6.21). This point is 4cm deep to the articular tubercle on the zygomatic arch, when accessed through the mandibular notch. After a short course the nerve divides into a small anterior (mainly motor) and a large posterior (mainly sensory) branch.
Branches from the main trunk
One sensory and one motor. The meningeal branch, or nervus spinosus, re-enters the middle cranial fossa via the foramen spinosum, or the foramen ovale, supplying the meninges of the middle cranial fossa, and the mastoid air cells.
The nerve to the medial pterygoid runs forwards to the muscle, and gives a branch which passes through the otic ganglion without synapse to supply the two tensor muscles, tensor palati and tensor tympani.
Branches from the anterior division
This division is motor, except for one branch (the buccal nerve).
Two deep temporal branches to temporalis pass above the upper border of the lateral pterygoid muscle; one may be a branch of the buccal nerve.
The masseteric nerve, passing above the upper border of the lateral pterygoid, emerges through the mandibular notch to enter the deep surface of the masseter. It gives an articular branch to the temporomandibular joint.
The nerve to the lateral pterygoid runs with the buccal nerve and supplies both heads of the muscle.
The buccal nerve contains all the fibres of common sensation in the anterior division of the mandibular nerve. It emerges between the two heads of the lateral pterygoid (Fig. 6.20) and courses downwards and forwards on the buccinator, giving branches to the skin over the cheek. It then pierces the buccinator (giving proprioceptive fibres to it) and supplies the mucous membrane of the cheek and the gum of the lower jaw opposite the lower molars and second premolar (i.e. up to the mental foramen).
Branches from the posterior division
This division is sensory except for the motor fibres which are distributed via the mylohyoid nerve. There are three branches.
The auriculotemporal nerve is derived by two roots from the posterior division; they embrace the middle meningeal artery (Fig. 6.21). The nerve passes backwards between the neck of the mandible and the sphenomandibular ligament, lying above the maxillary vessels. It gives a branch to the temporomandibular joint, and ascends over the lateral aspect of the zygomatic arch behind the superficial temporal vessels (Fig. 6.11). The auricular part innervates the skin of the tragus and upper part of the lateral surface of the pinna, the external acoustic meatus and the outer surface of the tympanic membrane. The temporal part is distributed to the skin of the temple. The auriculotemporal nerve is in contact with the anteromedial surface of the parotid gland, and supplies it with postganglionic secretomotor fibres from the otic ganglion.
The inferior alveolar (dental) nerve emerges below the lower head of the lateral pterygoid and curves down on the medial pterygoid (Fig. 6.20). The nerve lies anterior to its vessels between the sphenomandibular ligament and the ramus of the mandible, and enters the mandibular foramen. It is into this region, just above the foramen, that anaesthetic solution is introduced for inferior alveolar nerve block (see p. 379). The inferior alveolar nerve lies midway between the anterior and posterior borders of the mandibular ramus at the level of the midpoint of the posterior border of the ramus. The mylohyoid nerve leaves the inferior alveolar at the foramen. It pierces the sphenomandibular ligament and lies on a groove on the mandible in front of the insertion of the medial pterygoid (see Fig. 8.5B, p. 510), accompanied by small branches of the inferior alveolar artery and vein. The mylohyoid nerve then runs forward on the superficial (cervical) surface of the mylohyoid supplying it and the anterior belly of the digastric (Fig. 6.6); the nerve often carries sensory fibres from a small area of submental skin and may participate in the sensory supply to lower incisors.
The inferior alveolar nerve runs with its vessels in the mandibular canal. It supplies the three molar and two premolar teeth. Then it divides into the mental nerve (see p. 354) and the incisive nerve. The latter nerve supplies the canine and both incisors, with some overlap into the opposite central incisor.
The lingual nerve appears below the lateral pterygoid and passes forwards and downwards on the medial pterygoid (Fig. 6.20). It then comes into contact with the mandible, where the bone is thinned to form a shallow groove below and medial to the third molar, just above the posterior end of the mylohyoid line (see Fig. 8.5B, p. 510). This groove separates the attachments of the pterygomandibular raphe above and mylohyoid muscle below (Fig. 6.22). The nerve is characteristically flattened here, rather than round, and it enters the mouth on the superior surface of the mylohyoid. It gives off a gingival branch which supplies all the lingual gum and mucous membrane of the floor of the mouth. The lingual nerve then crosses the submandibular duct (see p. 338) and runs forwards and medially to the tongue.
The chorda tympani (from the facial nerve, see p. 417) emerges through the petrotympanic fissure (Fig. 6.35), grooves the medial surface of the spine of the sphenoid, and joins the lingual nerve at an acute angle (Fig. 6.21), 2cm below the base of the skull, and is distributed with it to the anterior two-thirds of the tongue. It carries parasympathetic secretomotor fibres to the submandibular ganglion and taste fibres from the anterior two-thirds of the tongue (see p. 382).
Otic ganglion
This small body lies between the tensor palati and the mandibular nerve, just below the foramen ovale. It is a flat plaque, about 2–3mm in diameter, closely applied to the medial surface of the nerve (Fig. 6.21). It is a relay station for parasympathetic secretomotor fibres to the parotid gland; the lesser petrosal branch of the glossopharyngeal nerve brings these fibres. Postganglionic sympathetic fibres from the plexus around the middle meningeal artery, sensory fibres from the auriculotemporal nerve and a branch from the nerve to the medial pterygoid (to tensor tympani and palati) pass through the ganglion without relay. The connections of the otic ganglion are summarised on page 22.
Carotid sheath and cranial nerves
Carotid sheath
The carotid sheath extends from the base of the skull to the arch of the aorta. In its upper part it is attached to the margins of the carotid canal and the jugular fossa. It contains here the internal carotid artery and internal jugular vein (see p. 343) and the last four (ninth to twelfth) cranial nerves. Medial to it lies the pharynx; laterally the deepest part of the parotid gland touches the sheath, partly separated by the styloid process and its three muscles. Anteriorly is the infratemporal fossa. Behind the carotid sheath lies the cervical sympathetic trunk on the prevertebral fascia.
The carotid canal lies immediately in front of the jugular foramen (which lies deep to the external acoustic meatus). The internal jugular vein lies behind the internal carotid artery at the base of the skull, but slopes as it descends, and at a lower level lies lateral to the common carotid artery as the vessels lie on scalenus anterior. At all levels the vagus nerve lies deep in the groove between the two, within the carotid sheath. The glossopharyngeal and accessory nerves emerge at the base of the skull between artery and vein and immediately curve away from each other superficial to the vessels (Fig. 6.23). The hypoglossal nerve emerges from the hypoglossal canal medial to the sheath. It passes through the sheath behind the inferior vagal ganglion and turns forwards to emerge between the artery and vein.
Glossopharyngeal nerve
The glossopharyngeal nerve emerges from the anterior part of the jugular foramen on the lateral side of the inferior petrosal sinus (see p. 447). It makes a deep notch in the inferior border of the petrous bone and here its inferior ganglion bulges the nerve. The ganglion contains the cell bodies of most sensory fibres in the nerve. The nerve passes down on the lateral aspect of the internal carotid artery and curves forward around the lateral side of stylopharyngeus (Figs 6.23 and 6.41). It passes deep to the external carotid artery and continues forward deep to hyoglossus to reach the tongue (see p. 382).
The tympanic branch (Jacobson’s nerve) leaves the nerve at the jugular fossa and passes through a canaliculus on the ridge of petrous bone between the carotid and jugular foramina (Fig. 6.19) to enter the temporal bone and supply the middle ear, mastoid air cells and bony part of the auditory tube with sensory fibres. In this branch are also parasympathetic fibres from the inferior salivary nucleus. They run through the tympanic plexus on the promontory and continue in the lesser petrosal nerve. This nerve leaves the middle ear through its roof and runs along the floor of the middle cranial fossa to the foramen ovale, through which it passes to reach the otic ganglion (Fig. 6.27). The parasympathetic fibres relay in the otic ganglion for the secretomotor supply of the parotid gland and the other small glands of the vestibule of the mouth.
The motor branch to stylopharyngeus is given off as the nerve spirals around the posterior border of that muscle.
The carotid sinus nerve is the main supply to the carotid sinus and carotid body (baroreceptors and chemoreceptors.
One or more pharyngeal branches join the pharyngeal plexus on the middle constrictor muscle (see p. 386). They pierce the muscle and supply the mucous membrane of the oropharynx with common sensation and (a few) taste fibres.
The tonsillar branch supplies the mucous membrane over most of the (palatine) tonsil.
The lingual branch supplies the posterior one-third of the tongue with sensory fibres (common sensation and taste) and secretomotor fibres to the glands of the posterior third. These last relay in small ganglia in the mucous membrane.
Vagus nerve
The vagus nerve emerges through the middle compartment of the jugular foramen, in which a small enlargement constitutes the superior ganglion. Just below the base of the skull the elongated inferior ganglion dilates the trunk. The ganglia contain cell bodies of the afferent fibres of the vagus; the superior ganglion for the meningeal and auricular branches, the inferior ganglion for all the other sensory fibres. Just above the inferior ganglion the vagus is joined by a large branch from the accessory nerve (cranial part), comprising nucleus ambiguus fibres for the skeletal muscle of the soft palate, pharynx and larynx.
The nerve runs straight down the neck, within the carotid sheath, between and behind carotid (internal and common) artery and jugular vein. In the root of the neck it passes in front of the subclavian artery and so enters the mediastinum (see p. 196) to supply thoracic and abdominal viscera.
Meningeal branches pass up from the superior ganglion to supply the dura mater of the posterior fossa below the tentorium.
The auricular branch (Arnold’s nerve) runs laterally through a canaliculus in the lateral wall of the jugular fossa. It supplies the posteroinferior quadrant of the outer surface of the tympanic membrane and a small adjacent area of skin of the external acoustic meatus and a little area of skin on the cranial auricular surface.
The very fine carotid body branch forms a plexus with the carotid sinus branch of the glossopharyngeal for the supply of those structures.
The pharyngeal branch of the vagus passes forward between the internal and external carotid arteries (Fig. 6.23) and joins the pharyngeal plexus on the middle constrictor muscle. The fibres supply the muscles of the pharynx (except stylopharyngeus) and the muscles of the soft palate (except tensor palati, see p. 390).
The superior laryngeal nerve slopes downwards on the side wall of the pharynx deep to the internal carotid artery (Fig. 6.23). It divides into a large internal laryngeal nerve which pierces the thyrohyoid membrane to reach the piriform recess (see p. 388), carrying sensory fibres for the pharynx and larynx, and a small external laryngeal nerve which runs down close to the superior thyroid vessels, outside the larynx, to supply cricothyroid and contribute to the supply of the inferior constrictor.
The cervical cardiac branches are two on each side. They all pass down to the deep part of the cardiac plexus (see p. 194), except for the lower left branch which goes to the superficial part of the plexus.
The recurrent laryngeal nerve on the right hooks around the subclavian artery at the root of the neck (Fig. 6.9). On the left side the recurrent laryngeal nerve is given off in the superior mediastinum and recurves around the ligamentum arteriosum under the arch of the aorta (see Fig. 4.13, p. 192). Both nerves then ascend along the posterolateral border of the trachea, in a groove between it and the oesophagus, and pass under the lower border of the inferior constrictor. Both nerves have cardiac branches, and also supply the trachea, oesophagus and the cricopharyngeus part of the inferior constrictor, before entering the pharynx and larynx to supply the laryngeal muscles (except cricothyroid) and the laryngeal mucosa from the vocal folds downwards (see p. 396).
Accessory nerve
The accessory nerve is formed in the posterior cranial fossa by union of cranial and spinal (cervical) roots. The nerve occupies the middle compartment in the jugular foramen, just lateral to the vagus, with which it shares a meningeal sleeve. All the fibres of its cranial root leave the nerve in a branch which joins the vagus. The nerve, now consisting of cervical fibres only, runs downwards and backwards on the internal jugular vein (Fig. 6.23), where the latter lies on the transverse process of the atlas; the nerve crosses lateral (usually) or medial to the vein. It passes deep to the styloid process and posterior belly of the digastric, where it is crossed by the occipital artery. With the upper sternocleidomastoid branch of the occipital artery it reaches the sternocleidomastoid, supplies it and enters its deep surface. Emerging from the posterior border of the muscle it crosses the posterior triangle (see p. 333) to supply trapezius.
Hypoglossal nerve
The hypoglossal nerve emerges from the hypoglossal canal. It picks up a branch from the anterior ramus of C1 and then spirals behind the inferior ganglion of the vagus to emerge between the internal carotid artery and internal jugular vein, passing through the carotid sheath. It then descends on the carotid sheath, deep to the styloid muscles and the posterior belly of digastric. It is crossed by the occipital artery and its lower sternocleidomastoid branch and then turns forwards, superficial to both carotid arteries and the loop of the lingual artery (Fig. 6.23), just above the tip of the greater horn of the hyoid bone. It continues forwards on the hyoglossus (Fig. 6.24), accompanied by veins draining the tip of the tongue, to supply tongue muscles.
The C1 fibres that join the hypoglossal nerve leave it progressively in the superior root of the ansa cervicalis and in the branches to thyrohyoid and geniohyoid. The small meningeal branch which enters the posterior fossa through the hypoglossal canal also comprises C1 fibres.
Styloid apparatus
The styloid process is a part of the temporal bone. From its tip the stylohyoid ligament passes to the lesser horn of the hyoid bone (Fig. 6.24). Both process and ligament are remnants of the second pharyngeal arch cartilage (see Fig. 1.21, p. 25). Hence the styloid process is very variable in length, the ligament varying likewise, inversely with it.
Three muscles diverge from the styloid process and are described elsewhere. The stylopharyngeus (see p. 386) arises highest from the medial side of the base of the process and passes downwards to the larynx. The stylohyoid (see p. 335) arises from the posterior surface near the base, and the styloglossus (see p. 381) from in front low down and from the upper end of the stylohyoid ligament; they diverge as they pass downwards and forwards to the hyoid bone and side of the tongue respectively. Each of the three muscles has a different nerve supply. They all act significantly during swallowing.
The styloid apparatus (process and muscles) lies lateral to the carotid sheath. The external carotid artery passes between the muscles of the stylohyoid apparatus. It runs up deep to digastric and stylohyoid, but superficial to stylopharyngeus (Fig. 6.23), to enter the parotid gland. The retromandibular vein, on the other hand, passes down from the parotid gland superficial to stylohyoid and digastric.
Part nine. Pterygopalatine fossa
At the anterior end of the medial wall of the infratemporal fossa the lateral pterygoid plate is separated from the maxilla by the pterygomaxillary fissure, which leads into the small pterygopalatine fossa. At the bottom of the fissure, the pyramidal process of the palatine bone articulates with the lateral pterygoid plate and maxilla closing off the fissure and forming the narrow floor of the pterygopalatine fossa (Fig. 6.13). The roof is the body of the sphenoid. Medially the fossa is walled in by the perpendicular plate of the palatine bone (Fig. 6.25), part of the lateral wall of the nose (Fig. 6.31A). This plate splits at the top into an orbital process and a sphenoidal process which, with the roof of the fossa, bound the sphenopalatine foramen that communicates with the nasal cavity. The perpendicular plate articulates anteriorly with the maxilla and between the two lies the greater palatine canal which opens below at a foramen on the hard palate. The posterior wall of the maxilla forms the anterior wall of the fossa, which is interrupted at the top by the medial end of the inferior orbital fissure that opens into the orbit. The pterygopalatine fossa is bounded posteriorly by the sphenoid bone (root of the pterygoid process containing the pterygoid canal and greater wing containing the foramen rotundum; Fig. 6.26).
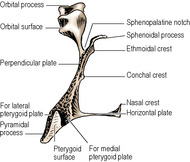 |
| Figure 6.25 |
The fossa contains the maxillary vessels and nerve and the pterygopalatine ganglion and fat (Fig. 6.21). The ganglion sends branches into the nose, palate and nasopharynx. The maxillary nerve supplies the posterior, upper teeth and passes forwards into the orbit. Branches of the maxillary vessels accompany all these nerves.
Maxillary nerve
The maxillary nerve, giving a meningeal branch to the front of the middle cranial fossa, passes through the foramen rotundum in the greater wing of the sphenoid bone into the pterygopalatine fossa. Deviating laterally in the inferior orbital fissure for about 1cm, it turns forwards to enter the infraorbital groove and canal in the floor of the orbit, changing its name to the infraorbital nerve and eventually emerging from the front end of the canal at the infraorbital foramen to supply skin on the face (see p. 354). The zygomatic nerve arises from the maxillary in the fossa and runs above the maxillary in the inferior orbital fissure to enter the orbit (see p. 402). The posterior superior alveolar nerve is also given off in the fossa. It passes through the pterygomaxillary fissure on to the posterior wall of the maxilla (see p. 364).
In the fossa the maxillary nerve is connected to the pterygopalatine ganglion by two branches that carry fibres going both to and from the ganglion.
Pterygopalatine ganglion
The pterygopalatine ganglion is a relay station between the superior salivary nucleus in the pons and the lacrimal gland and mucous and serous glands of the palate, nose and paranasal sinuses. It is the ganglion of hay fever (‘running nose and eyes’). Its connections are summarized on page 22.
The ganglion lies immediately in front of the opening of the pterygoid canal and the nerve of that canal runs straight into the back of the ganglion. The canal is below and medial to the foramen rotundum (Fig. 6.26), and so is the ganglion in relation to the maxillary nerve.
The autonomic root is the nerve of the pterygoid canal (Vidian nerve). This nerve is formed in the foramen lacerum by union of the greater petrosal nerve (see p. 417), containing mainly parasympathetic secretomotor fibres, with the deep petrosal nerve, containing sympathetic vasoconstrictor fibres. The former is a branch of the facial nerve and the latter is a branch from the internal carotid sympathetic plexus. The combined nerve passes forward in the pterygoid canal and joins the ganglion.
The postganglionic secretomotor fibres to the lacrimal gland leave the ganglion and join the maxillary nerve, pass in its zygomatic branch into the orbit, join the lacrimal branch of the ophthalmic nerve and so reach the lacrimal gland.
The rest of the fibres in the connections between the maxillary nerve and the ganglion are sensory and, like the sympathetic fibres in the deep petrosal nerve, they pass through the ganglion without relay. The only cell bodies in the ganglion are parasympathetic (secretomotor). The branches of the pterygopalatine ganglion are distributed to the nose, palate and nasopharynx. Every branch carries a mixture of all three kinds of fibres: sensory, secretomotor and sympathetic.
Medial posterior superior nasal nerves pass through the sphenopalatine foramen, cross the roof of the nose, and are distributed to the septum. The largest of these is termed the nasopalatine nerve, as it continues beyond the septum through the incisive canal to supply the anterior part of the hard palate.
The lateral posterior superior nasal nerves pass through the sphenopalatine foramen and turn forward to supply the posterosuperior part of the lateral wall of the nose.
The greater palatine nerve passes down through the greater palatine canal, between the perpendicular plate of the palatine bone and the maxilla (Fig. 6.27). At the greater palatine foramen it turns forward to supply the mucous membrane of the hard palate. As it descends it also supplies the posteroinferior part of the lateral wall of the nose and the medial wall of the maxillary sinus.
The lesser palatine nerves, two in number, pass down behind the greater palatine nerve and emerge through the lesser palatine foramina. They pass back to the soft palate and the mucous membrane of the palatine tonsil. They carry the only non-secretomotor fibres transmitted in the greater petrosal nerve; these are sensory (taste) fibres that have their cell bodies in the genicular ganglion of the facial nerve.
The pharyngeal nerve passes back through the palatovaginal canal (a little canal between the vaginal process of the medial pterygoid plate and the sphenoidal process of the palatine bone) and supplies the mucous membrane of the nasopharynx. A few fine orbital branches enter the orbit via the inferior orbital fissure and supply periosteum of the orbital floor and the mucous membrane of the sphenoidal and ethmoidal sinuses.
Maxillary vessels
The maxillary artery passes through the pterygomaxillary fissure, enters the pterygopalatine fossa in front of the ganglion and gives off five branches. These and the artery’s further course into the orbit are described on page 363. The branches of the maxillary artery in the pterygopalatine fossa may be ligated by an approach through the maxillary sinus (see p. 376), the fossa being entered instrumentally through the posterior wall of the sinus. An alternative endoscopic approach is via the sphenopalatine foramen.
Veins accompany the above arteries and, passing through the fossa, emerge at the pterygomaxillary fissure to drain into the pterygoid plexus. In general, vessels in the fossa lie anterior to the nerves.
Part ten. Nose and paranasal sinuses
The nose is for breathing; the design of its cavity results in warming and moistening the inspired air, and in cleaning it too. Since odours are airborne, the olfactory receptors are placed in the nose. The floor of the nose is the hard palate. Hence chewing can go on in the mouth cavity without interfering with breathing; the flap valve of the soft palate, in the dependent position, meanwhile shuts off the mouth cavity from the airway through the oropharynx. Breathing is arrested during swallowing; the soft palate is elevated and shuts off the nose (i.e. the nasopharynx) from the foodway through the oropharynx. Thus the oropharynx is the crossroads of airway and foodway; collisions between air stream and food are avoided by the control mechanism of the soft palate acting as the policeman on point duty.
The nose consists of the external nose and the nasal cavity, which is divided into right and left halves by the midline nasal septum.
External nose
The external nose projects forwards from the face. Its upper end or root is continuous with the forehead. At its lower end (base) are the nares (nostrils). The sides of the nose meet in the midline anteriorly to form the dorsum. The upper part of the dorsum is the bridge and at the lower end of the dorsum is the tip of the nose. The lower flared part of the side of the nose is the ala.
The supporting framework of the nose consists of bone and cartilage. The upper part is supported by the pair of nasal bones articulating posteriorly with the maxillae and above with the frontal bones. Inferiorly the nasal bones overlap the superior margins of the (upper) lateral cartilages, with fusion of their periosteum and perichondrium. In their lower parts the lateral cartilages are separated by a cleft in which the septal cartilage extends to the dorsum of the nose. The lateral cartilages are connected to the maxillae posteriorly and to the major alar (lower lateral) cartilages inferiorly by fibrous tissue. The latter cartilages are markedly curved, being bent upon themselves towards the nasal cavity, each having a lateral crus that supports the ala and a medial crus which, with its fellow of the opposite side, forms the columella that separates the nares in the midline. The lateral and medial crura are connected by a middle crus. The configuration of the two middle crura determines the shape of the tip of the nose. The lateral crus does not reach the margin of the naris, the rim being formed by fibrofatty tissue. The same tissue connects the posterior end of the lateral crus to the maxilla and two or three minor alar cartilages lie here.
The skin of the nose is thinnest at its upper part where it is loosely attached to the nasal bones and the upper lateral cartilages. The skin is thickest at the lower part where it has an abundance of sebaceous glands and is tightly bound down to the alar cartilages. The muscles of the nose are described with the muscles of the face on page 351.
The skin is supplied by the external nasal nerve (the terminal part of the anterior ethmoidal, which notches the inner surface of the nasal bone); this nerve emerges at the lower margin of the nasal bone and passes down on the upper and lower nasal cartilages to the tip of the nose. The infratrochlear branch of the nasociliary nerve and nasal branches of the infraorbital nerve also contribute to the supply of nasal skin (Fig. 6.15A).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree