Hamartomatous Polyps, Juvenile
Amitabh Srivastava, MD
Key Facts
Terminology
Hamartomatous polyp that may occur sporadically or as part of polyposis syndrome
Etiology/Pathogenesis
Germline mutations in SMAD4 or BMPR1A present in juvenile polyposis patients
Clinical Issues
Patients usually present at early age with anemia, diarrhea, or bleeding
Juvenile polyposis syndrome patients typically have between 50-200 polyps
Risk of colorectal cancer
Mean age for colon cancer in juvenile polyposis patients is ˜ 35 years
Risk is approximately 68% by 60 years of age
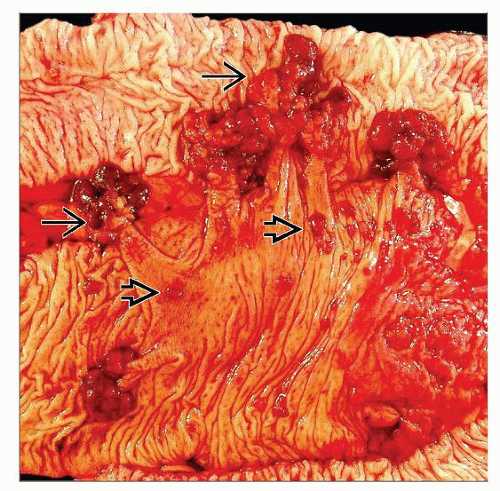
Macroscopic Features
JP patients usually have more than 50 polyps
Size is variable, but most measure around 1.0 cm in greatest dimension
Majority of polyps (> 2/3) are pedunculated
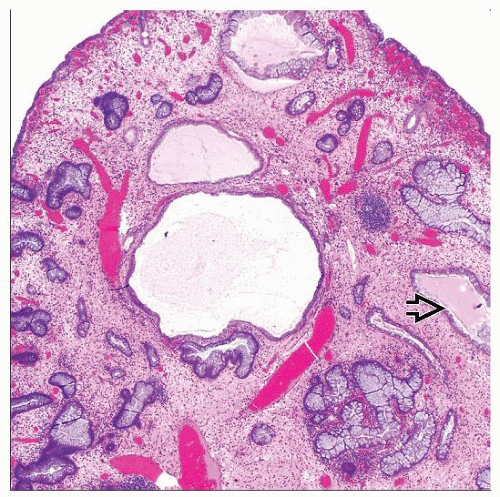
Microscopic Pathology
Marked expansion of lamina propria by loose, edematous, and inflamed stroma
Epithelial component is cystically dilated and shows variable degree of inflammation
Surface ulceration may be present
Gastric polyps resemble hyperplastic polyps or those seen in Cronkhite-Canada syndrome
Dysplastic change or carcinoma may be present in syndromic patients
TERMINOLOGY
Abbreviations
Juvenile polyp (JP)
Juvenile polyposis syndrome (JPS)
Definitions
Hamartomatous polyp
May occur sporadically
May be manifestation of inherited familial polyposis syndrome
Patients with JPS have increased risk of colorectal carcinoma
No increase in cancer risk in sporadic JP
ETIOLOGY/PATHOGENESIS Genetics
Germline mutations in SMAD4 (DPC4) gene on 18q21 present in about 20% of JPS patients
Exon 9 deletion is most common abnormality
Patients with SMAD4 germline mutations more likely to have
Polyps in upper gastrointestinal tract
Positive family history
Germline mutations in BMPR1A gene on 10q23 present in similar proportion of JPS cases
Variety of mutations have been identified in JP families
Mutations in SMAD4 and BMPR1A genes interfere with TGF-β signaling pathway
CLINICAL ISSUES
Presentation
Hematochezia
Anemia
Diarrhea
Prolapse
Juvenile polyps occur in distinct clinical settings
Sporadic juvenile polyp
90% of all polyps in children
20-50% may have more than 1 polyp
No increase in risk of colorectal carcinoma
Polyps histologically identical to those in JPS patients
Juvenile polyposis coli
Most common inherited form
Present clinically in 1st decade
Polyps confined to colon
Generalized juvenile polyposis
Diffuse involvement of gastrointestinal tract
Colon, stomach, and small intestine involved
Gastric juvenile polyposis
Rare form of disease
Polyps confined to stomach
Patients may present with protein-losing enteropathy and mimic Cronkhite-Canada syndrome
Juvenile polyposis of infancy
Rare, autosomal recessive disease
Usually associated with death in infancy
Diagnostic criteria for juvenile polyposis syndrome
More than 5 juvenile polyps (most patients have between 50-200)
Any number of polyps in patient with positive family history
Extracolonic juvenile polyps are almost always syndromic
Extracolonic manifestations present in about 2/3 of JPS patients
Macrocephaly, hydrocephalus, and mental retardation
Congenital heart disease
Pulmonary arteriovenous malformation
Cleft palate and polydactyly
Malrotation and Meckel diverticulum
Cryptorchidism
Risk of colorectal cancer
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree