14 Haemostasis and thrombosis
Haemostasis
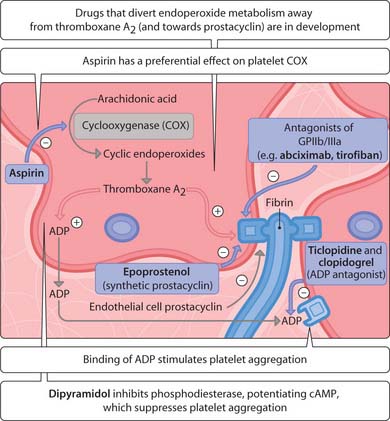
The body responds to a rupture of the blood vessels by constriction, platelet aggregation, plug formation and blood clotting. Disruption of blood vessels exposes underlying collagen, which platelets adhere to by binding von Willebrand factor (vWF). This results in platelet activation and release of vasoconstrictors such as thromboxane A2, thereby reducing blood flow to the affected area. This mediator, along with platelet-derived ADP, serotonin and thrombin (factor IIa), causes other platelets to aggregate. The surrounding undamaged endothelium releases prostaglandin I2 (prostacyclin) and nitric oxide, which serve to limit platelet adherence and aggregation. The activation of thrombin converts soluble fibrinogen to fibrin. Liquid blood is converted to a solid gel reinforcing the platelet plug, which consists of aggregating platelets, fibrin and trapped red blood cells. The pathological formation of a clot can cause occlusion within blood vessels, leading to myocardial infarction, stroke and peripheral ischaemia (arterial side), deep vein thrombosis (DVT) and pulmonary embolism (venous side) and death.
Treatment of thrombosis
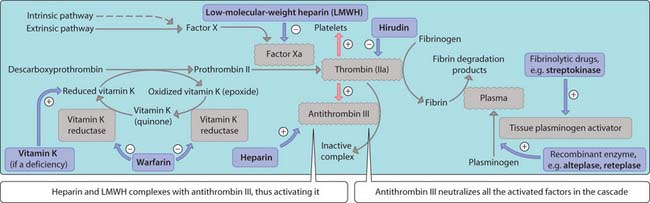
Drugs used in the treatment of thrombosis interfere with the coagulation pathway (Fig. 3.14.1), platelets (Fig. 3.14.2) or the fibrinolytic pathway (Fig. 3.14.1) and are generally used in combination for optimal results (Fig. 3.14.3).
Anticoagulants
Warfarin
Thrombin plays a central role in haemostasis and acts in a positive feedback loop to stimulate its own formation. Several coagulation factors, including factors II, VII, IX and X, require post-transcriptional carboxylation of their glutamic acid residues for full enzymatic activity and are dependent upon the oxidation of vitamin K, an essential cofactor in this process. Warfarin inhibits vitamin K epoxide reductase, a hepatic enzyme (Fig. 3.14.2). A delay (approximately 5 days) in the anticoagulant action of warfarin is observed because of slow clearance of existingg-carboxylated coagulation factors from the circulation (prothrombin has the longest elimination half-life). Warfarin is administered orally; side-effects include haemorrhage and teratogenicity (avoided in the first trimester).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree