Chapter 11 Haemopoietic and Lympho-Reticular Tissues
Haematology – Laboratory Tests
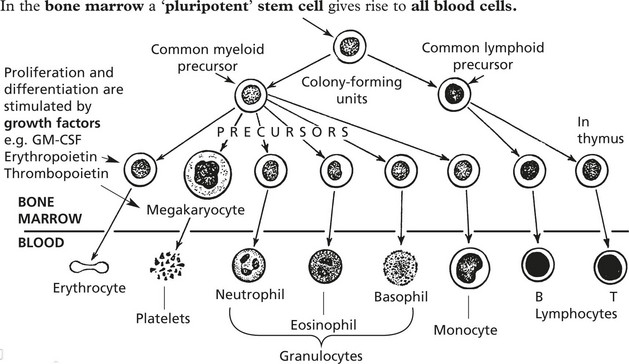
Investigation of blood diseases depends on examination of 1. peripheral blood and 2. bone marrow.
Blood count: this is normally done by sophisticated electronic machines.
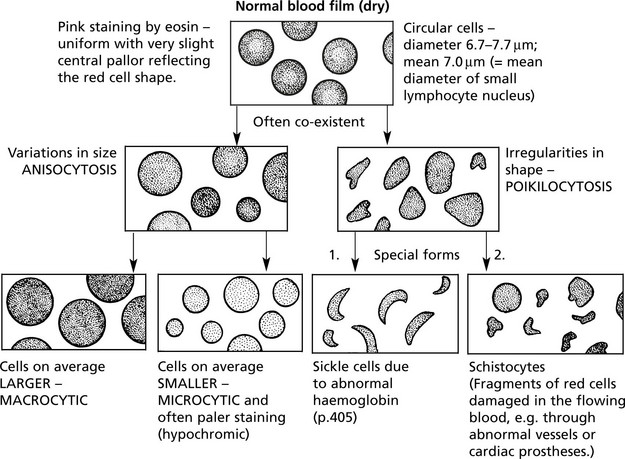
BLOOD FILM – stained by a Romanowski method.
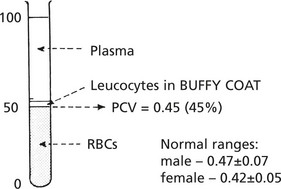
Another useful test is the measurement of the PACKED CELL VOLUME (PCV) or haematocrit.
This is obtained by centrifuging anticoagulated whole blood in a haematocrit tube.
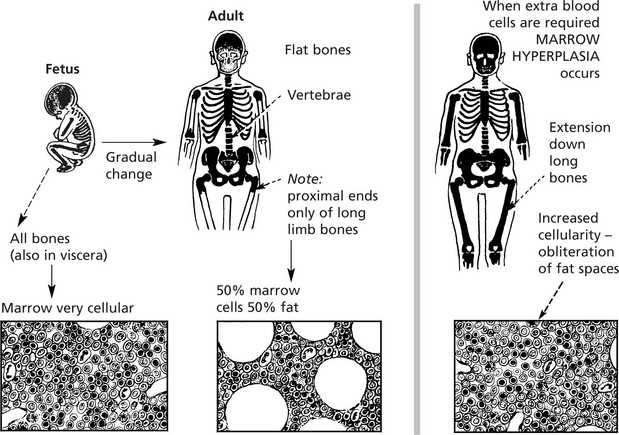
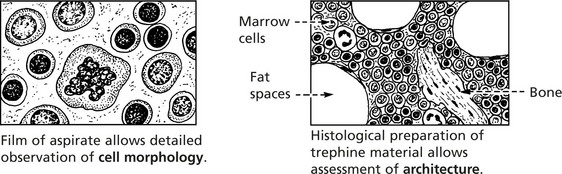
Examination of bone marrow is important in explaining abnormalities of the peripheral blood.
Anaemia
The most important function of the red cell is the transport of oxygen bound to haemoglobin. The most common and important disorder associated with disease of the red cells is ANAEMIA, which is defined as a reduction below normal of the concentration of haemoglobin in the blood.
Anaemia in men – Hb < 13 g/dl: in women – < 11.5 g/dl.
Clinical Associations
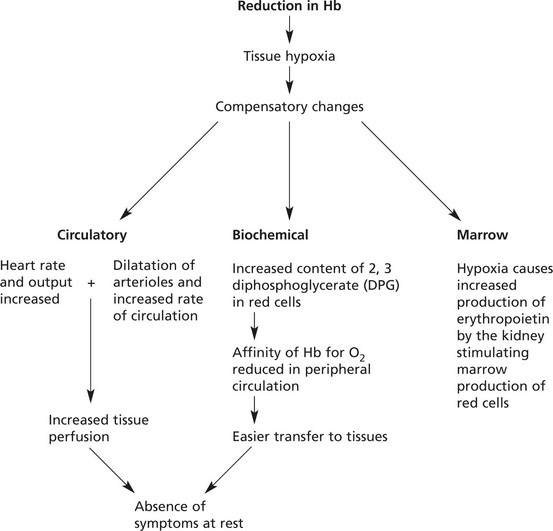
The effects of anaemia depend on its severity, rate of development and duration.
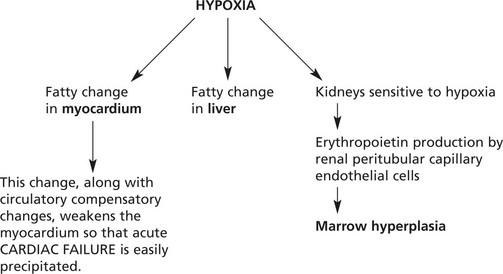
Pathological Complications of Anaemia
Causes of Anaemia
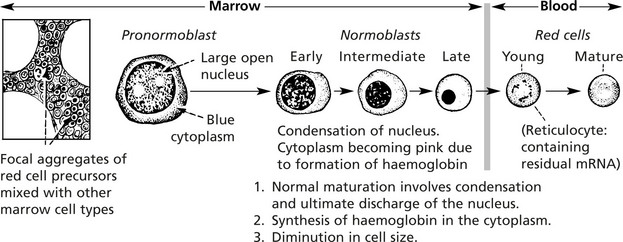
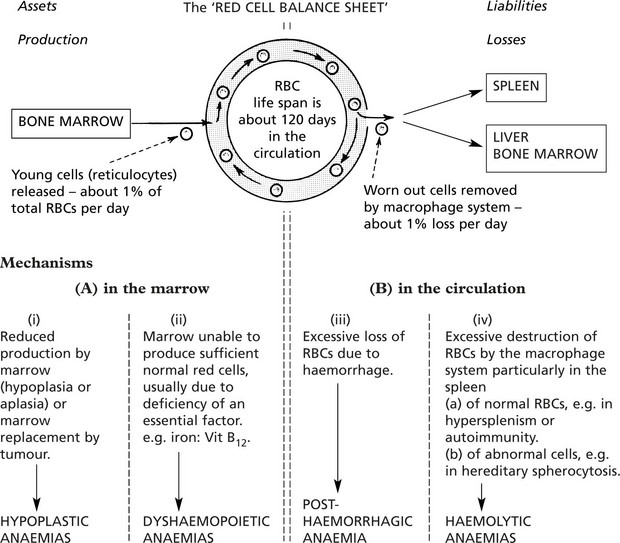
An understanding of the four main mechanisms by which anaemia develops depends on a knowledge of the life-cycle of red blood cells.
Note: Many forms of anaemia have more than one component.
Hypoplastic and Aplastic Anaemias
These are rare conditions and, as the names imply, are due to marrow failure with diminished numbers or absence of haemopoietic cells. Usually all three marrow cell lines are affected, resulting in pancytopenia in the peripheral blood.
Marrow failure of this type is dealt with in detail on page 407.
Marrow failure due to extensive tumour infiltration or fibrosis also occurs.
Iron Deficiency Anaemia
IRON DEFICIENCY ANAEMIA is the commonest anaemia on a world basis due to (a) poor nutrition, (b) intestinal parasites (esp. hookworm) causing bleeding and (c) multiple pregnancies.
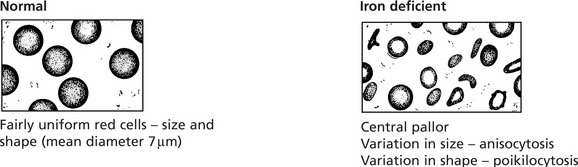
Changes in the blood: The red cells which show:
| Parameter | Low/High | Normal Range |
|---|---|---|
| MCV (mean cell volume) | LOW (< 80) | 80–92fl |
| MCH (mean cell haemoglobin) | LOW (< 27) | 27–32pg |
| MCHC (mean corpuscular haemoglobin concentration) | LOW (< 30) | 33 g/dl |
| Serum IRON | LOW | 10–30 mmol/l |
| Serum FERRITIN | LOW | 15–300 mg/l |
| Serum IRON BINDING CAPACITY | RAISED | 45–70 mmol/l |
Serum IRON SATURATION  | LOW | 16–60% |
Iron Metabolism
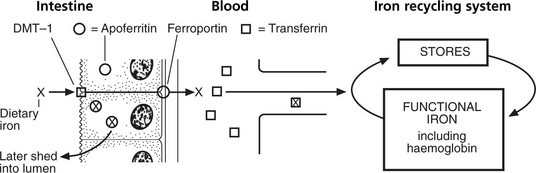
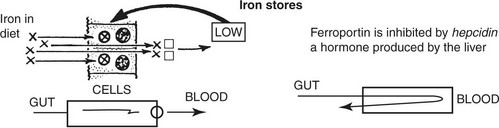
Iron is absorbed mainly in the duodenum and upper jejunum. Only small amounts are normally required to replace iron losses. Since the average diet contains more iron than is required, its absorption is controlled by the mucosal apoferritin mechanism.
Note: This bound iron is subsequently shed along with the cell into the lumen.
Acute Iron Overload
The iron balance may be summarised as follows.
| INPUT (Adult male) | BODY IRON Total 3–6g | OUTPUT |
|---|---|---|
| Average: 1 mg/day derived from foods | (a) Functional iron in haemoglobin, myoglobin, enzyme systems, transferrin  70% at least 70% at least | Average: 1 mg/day Skin desquamation and miscellaneous secretions |
| The average diet contains 10–20 mg iron, of which about 10% is absorbed. In the adult female, the average daily input is about 2 mg. | (b) Storage iron in liver, spleen, bone marrow as ferritin, haemosiderin  30% or less 30% or less | Menstruation This extra loss of about 0.5 to 1 mg requires extra input in the female |
Anaemia results when this balance is upset in:
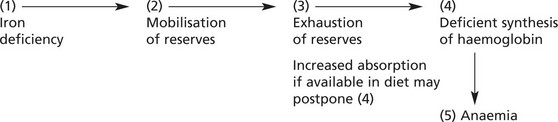
Usually anaemia develops slowly (except in cases of serious haemorrhage).
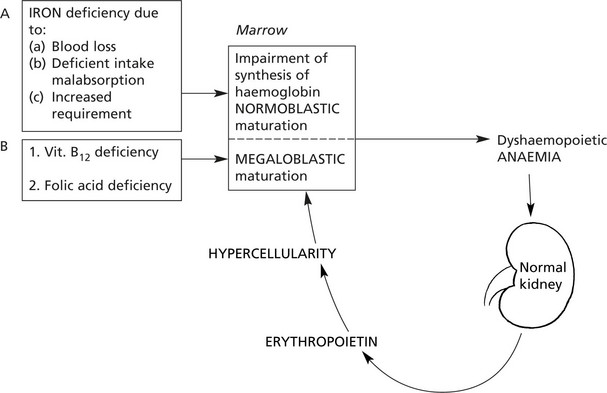
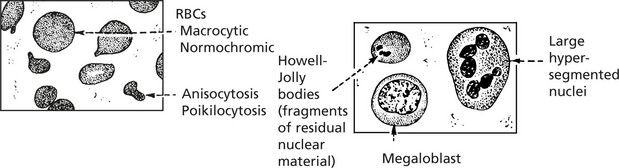
The Megaloblastic Anaemias
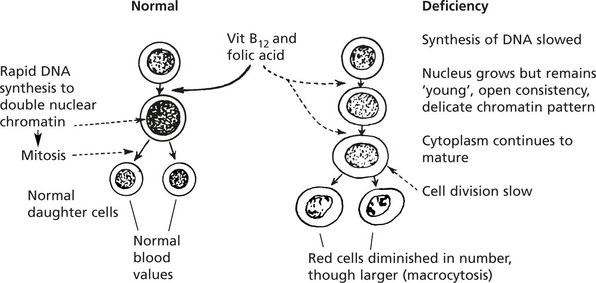
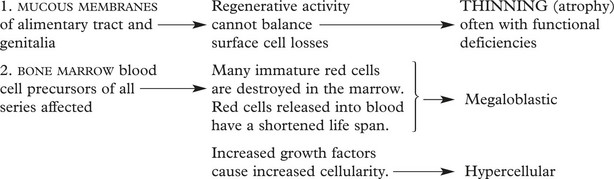
These dyshaemopoietic anaemias are almost always caused by deficiency of either vitamin B12 or folic acid which are intracellular co-enzymes, particularly important for the synthesis of DNA.
Pernicious Anaemia (PA)
This serious and severe anaemia was first described by the English physician Addison in the mid 19th century. At that time it was invariably fatal, but now is treatable. It is due to vitamin B12 deficiency and is always associated with achlorhydria and gastric mucosal atrophy, due to autoimmune gastritis.
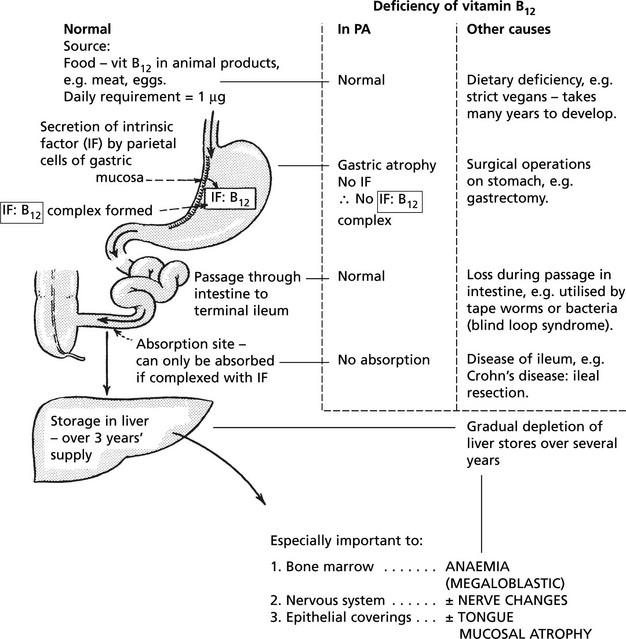
Vitamin B12 metabolism and causes of deficiency:
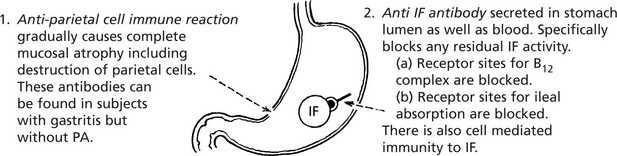
Mechanism of Production of Gastritis
PA is an autoimmune disease. The gastric atrophy is caused by an immune reaction against parietal cell cytoplasmic constituents and specifically by antibodies to intrinsic factor (IF).
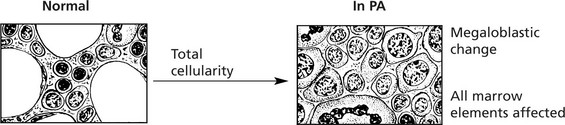
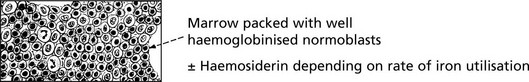
Marrow Changes
Hyperplasia – often complete cellularity in flat bones and extension down length of femur.
Folic Acid Deficiency
Folic Acid (Pteroyl-Glutamic Acid) Deficiency
| Normal metabolism | Deficiency |
|---|---|
| Source | Dietary |
| Polyglutamines in green vegetables, cereals, meat, fish and eggs (not milk) | Low intake of vegetables. Anorexia, alcoholism, poverty (elderly), infants (late weaning) |
| Minimum daily requirement | Increased requirements |
|---|---|
| 50 μg | Pregnancy (fetal growth) Infancy and childhood (rapid growth) |
| Body reserves 50–100 days | Haemolysis Malignancy |
| Absorption | Malabsorption |
|---|---|
As mono-glutamate in jejunum  | Coeliac disease Surgical by-pass |
| Utilisation | Utilisation block |
|---|---|
| For DNA synthesis. Vit B12 is necessary for synthesis of the active tetrahydrofolate form (FH4) | Drugs e.g. methotrexate in cancer chemotherapy also anti-convulsants e.g. phenytoin. |
The Haemolytic Anaemias
Haemolytic Anaemias
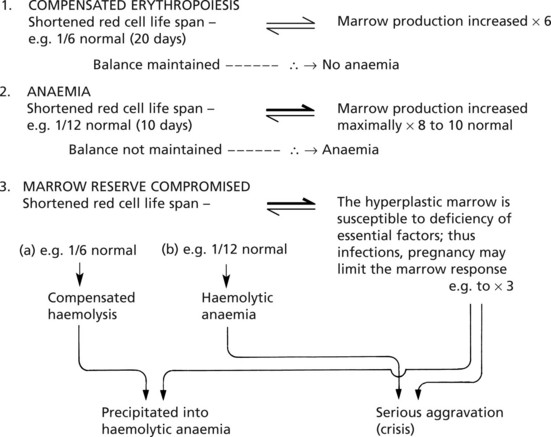
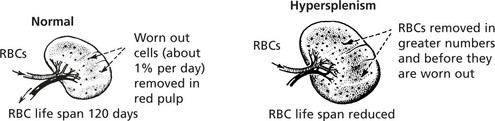
In all haemolytic anaemias, there is a reduction in the life span of the red cells; due to an increased rate of red cell destruction – haemolysis.
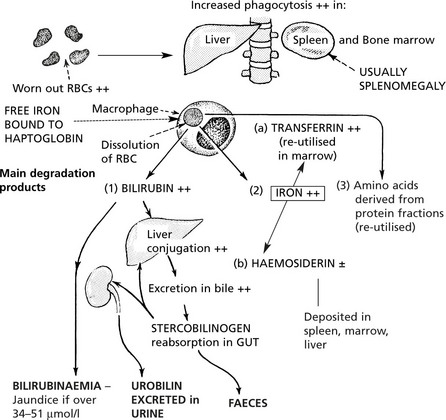
Effects of the Increased Degradation of Haemoglobin
In most haemolytic conditions, the red cells are removed and the haemoglobin degraded in the usual way, i.e. by phagocytosis by the macrophage system.
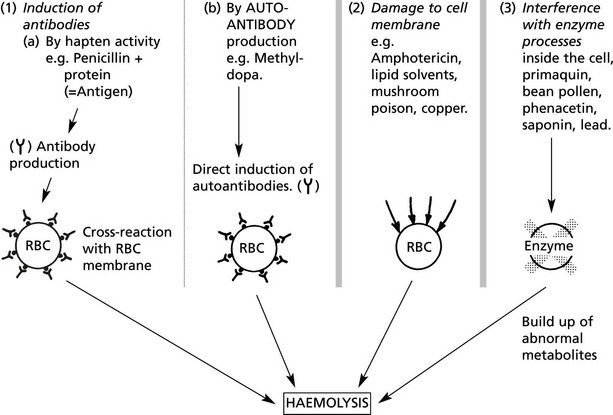
Extrinsic Haemolytic Anaemias
The causes of shortened red cell survival are divided into 2 main groups.
(1A) Autoimmune Haemolytic Anaemia
| warm (37 °C – usually IgG) | cold (< 30 °C – usually IgM) |
| Primary – so-called idiopathic haemolytic anaemia: usually in adults. | Idiopathic cold agglutination disease |
| Secondary – associated with | Mechanism 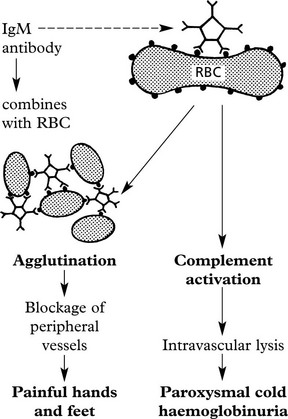 |
| Mechanism: Coating of RBC with IgG antibodies often against Rhesus ‘e’ antigens. 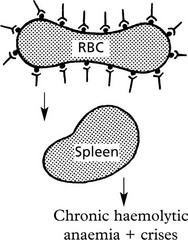 Destruction in spleen which is often enlarged. |
Incompatible Blood Transfusion/Haemolytic Disease of the Newborn
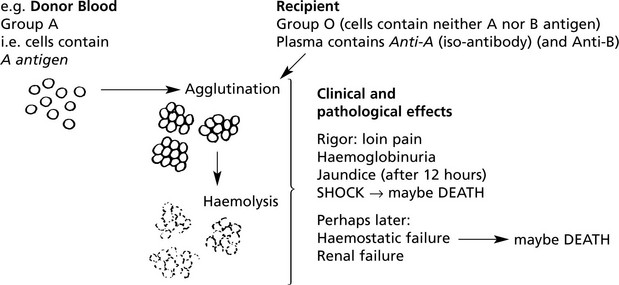
(1B) Destruction of RBCS is due to Iso-Antibodies
In these, the antibodies act against antigens which are derived from another individual of the same species.
Incompatible ABO blood transfusion is a classic example.
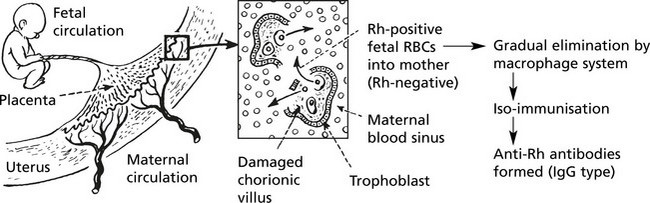
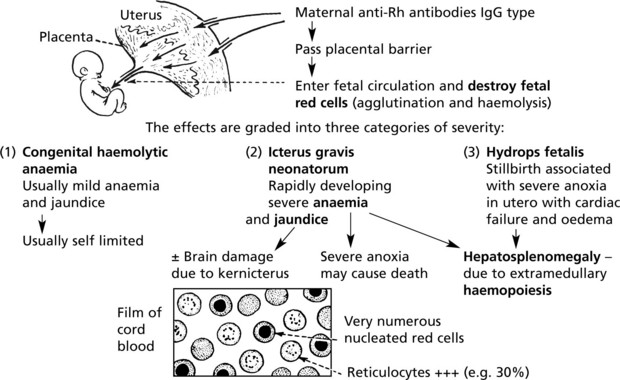
Haemolytic Disease of the Newborn
The basic mechanism is influenced by three important factors:
Injection of anti-Rh antibody minimises immune response.
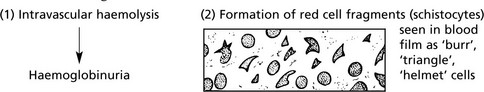
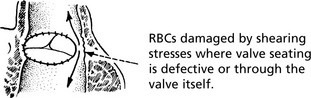
Extrinsic Haemolytic Anaemias
The results of damage to red cells within the circulation are:
The main circumstances in which red cells are damaged are:
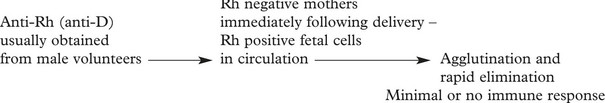
Other causes of haemolysis include:
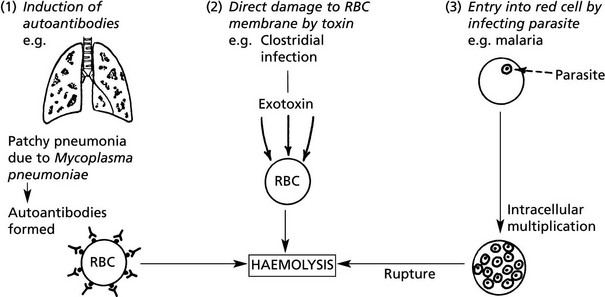
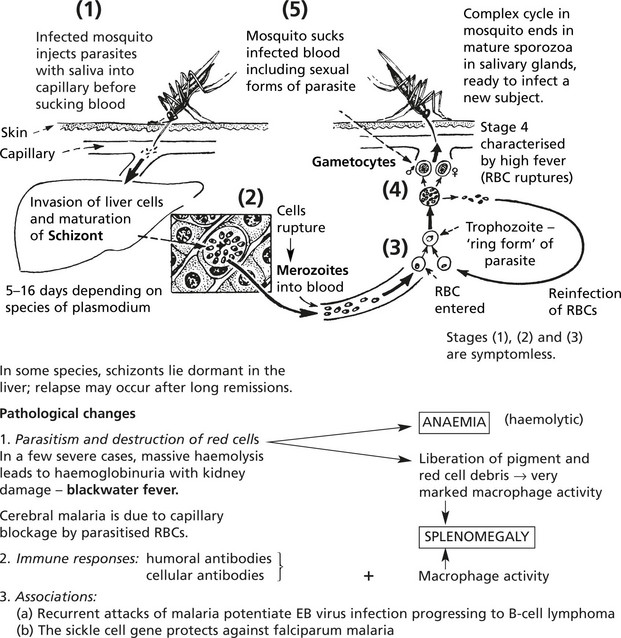
Extrinsic Haemolytic Anaemias – Malaria
Malaria is an endemic disease in many parts of Africa, Asia, Central and South America. Many millions of cases occur each year and the mortality is at least 1%. The disease is particularly severe in non-immune subjects from temperate climates; in endemic areas where the ‘herd’ immunity is high, a low grade chronic illness is common.