Granulomatosis with Polyangiitis (Wegener)
Surya V. Seshan, MD
Key Facts
Etiology/Pathogenesis
Form of ANCA-mediated small vessel vasculitis
Usually due to anti-PR3 antibodies (˜ 75%), others to MPO
Clinical Issues
Peak age at onset: 30-50 years
Kidney, upper airway, and lung involvement in 90% of cases
Present with acute or rapidly progressive renal failure
Steroids combined with cyclophosphamide; plasmapheresis beneficial in severe disease
Poor prognostic factors
High initial creatinine, concomitant lung disease
Frequency of renal relapses
Few preserved glomeruli
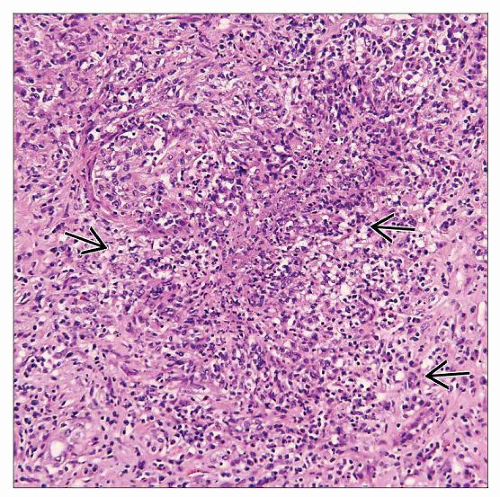
Microscopic Pathology
Fibrinoid necrosis, crescents (cellular, fibrocellular, and fibrous types)
Occasional interstitial (extravascular) granulomas
Interlobular and smaller arteries affected by vasculitis
Granulomatous inflammation in vessel wall, perivascular or interstitial locations
Isolated or concomitant medullary capillaritis
Ancillary Tests
Pauci-immune with little or no immunoglobulins or complement components by IF
Top Differential Diagnoses
ANCA(+) vasculitides (Churg-Strauss syndrome, microscopic polyangiitis), anti-GBM disease, HSP, drug-induced vasculitis
TERMINOLOGY
Abbreviations
Granulomatosis with polyangiitis (GPA)
Synonyms
Wegener granulomatosis (WG)
Rhinogenic granulomatosis
Definitions
Chapel Hill Consensus Conference
GPA is granulomatous inflammation of respiratory tract and necrotizing vasculitis of small to medium-sized vessels (capillaries, venules, arterioles, and arteries), commonly with necrotizing glomerulonephritis (GN) with no or very few deposits (“pauci-immune crescentic GN”)
Americal College of Rheumatology (ACR) criteria
Nasal or oral inflammation with purulent discharges or oral ulcers
Abnormal chest radiograph
Cavitating or noncavitating nodules
Infiltrates
Abnormal urinary finding (e.g., microhematuria)
Granulomatous inflammation in vessel wall, perivascular or interstitial locations
Any 2 or more of the above have high diagnostic specificity and sensitivity
ETIOLOGY/PATHOGENESIS
Antineutrophil Cytoplasmic Antibody (ANCA)-mediated Small Vessel Vasculitis
Autoantibodies to proteinase 3 (PR3) in most patients (> 75%)
ANCAs react to peptide sequences in complementary PR3-molecule
These sequences have significant homology with infectious agents, e.g., Staphylococcus
Minority (< 25%) have antimyeloperoxidase (MPO) ANCA
Proteinase-3 (PR3)
Serine proteinase related to neutrophil elastase (55% homology)
Inactivated by combining with α-1-antitrypsin
Neutrophil activation via feedback loop with ANCA
Activated neutrophils express PR3 on surface
Neutrophils activated via binding of ANCA
Release of oxygen radicals, lytic enzymes, and inflammatory cytokines
Alternative pathway complement activation and mediation by C5a
Increased adhesion of neutrophils to previously activated endothelium and transmigration
Mediate endothelial damage and vascular inflammation
Disease activity related to inhibition of PR3-α-1-antitrypsin complex formation
Other antibodies
Antiendothelial antibodies identified
Lysosomal membrane protein-2, on surface of endothelial cells
T cells, B cells needed to promote autoimmune response
Genetic Risk Factors
MHC class II gene HLA-DRB1*0401
Odds ratio 2-3
Retinoid X receptor B (RXRB) polymorphism (nearby on chromosome 6p21.3)
HLA-DRB1*0401 not associated with Churg-Strauss syndrome or microscopic polyangiitis
DNAM-1 polymorphism (Gly307Ser)
Codes for CD226, DNAX accessory protein
Also in type I diabetes, multiple sclerosis, Graves disease
Limited evidence for other gene polymorphisms
SERPINA1 (α-1-antitrypsin), PTPN22 (protein tyrosine phosphatase), CTLA4, PD-1 gene (also Kawasaki disease), FCGR3B (FcγRIIIb)
Potential Triggers of Autoantibody Response
Possible triggers of ANCA formation include infections (bacteria, viral)
GPA onset more common in winter
Exposure to allergens
Exposure to dust, heavy metal, respiratory toxins
Animal Model
Passive transfer of ANCA (anti-MPO) causes glomerulonephritis with crescents in immunodeficient mice (RAG1 knockout)
CLINICAL ISSUES
Epidemiology
Incidence
30-60/1,000,000
Higher incidence in North America and northern Europe; lower in Asia
Increased reporting in last 2 decades due to increased awareness of the disease
Age
GPA can develop at any age
Peak age at onset: 30-50 years
Mean: 40 years
Can also occur in children and the elderly
Gender
Slight male predominance
Ethnicity
No ethnic predilection
Presentation
Multisystemic involvement, often preceded by constitutional symptoms
Kidney, upper airway, and lung involvement in 90% of cases
A pulmonary renal syndrome
2 phases of disease
Granulomatous disease of upper respiratory tract
Vasculitic phase
Renal
Renal symptoms usually follow but sometimes precede respiratory disease up to several years
Macroscopic or microscopic hematuria
Red blood cell casts
Oliguria
Rapidly progressive or acute renal failure
Sometimes insidious onset of renal insufficiency with proteinuria &/or hematuria
Mass lesion (rare)
Occasionally presents with renal mass
Laboratory Tests
Hematuria, proteinuria, elevated BUN, Cr
Anemia, elevated ESR
˜ 95% positive for ANCA
ELISA: Anti-PR3 ANCA (˜ 75%) or anti-MPO (˜ 25%)
Indirect IF: c-ANCA (PR3) or p-ANCA (MPO)
Rheumatoid factor positive (20-30%)
Treatment
Steroids combined with cyclophosphamide
Plasmapheresis is beneficial in severe disease
Maintenance therapies have oral cyclophosphamide, cyclosporine, azathioprine, or mycophenolate mofitel
Clinical trials to assess benefit of
Anti-CD20, targets B cells
Blocking tumor necrosis factor-α
Prognosis
20% renal morbidity and end-stage renal disease
Lack of treatment or late diagnosis leads to ESRD
Trend toward improved renal and patient survival is observed
Clinical factors of poor prognosis
Older age
High creatinine level at initial presentation
High serum titer of ANCA (anti-PR3)
Severity of initial vascular damage
Multisystem involvement
Concomitant lung involvement or hemorrhage
Increased relapse rate (10-50%)
Clinical factors of good prognosis
Close to normal baseline renal function
Renal Transplantation
Patient and graft survival rates are comparable to those observed in non-ANCA patients
Both renal and extrarenal relapses occur after renal transplantation (though uncommon)
Recurrent disease or relapses are managed effectively by cyclophosphamide therapy
IMAGE FINDINGS
Radiographic Findings
Chest x-ray shows shifting infiltrates in lungs
Single or multiple nodular lung lesions
Diffuse pulmonary infiltrates suggesting hemorrhage
MACROSCOPIC FEATURES
Kidney
Usually normal in size or slightly enlarged
In acute phase, small scattered infarcts and petechial hemorrhages in cortex and medulla
Larger vessels appear grossly normal
Aneurysms or thrombi are rare
Focal or diffuse papillary necrosis
MICROSCOPIC PATHOLOGY
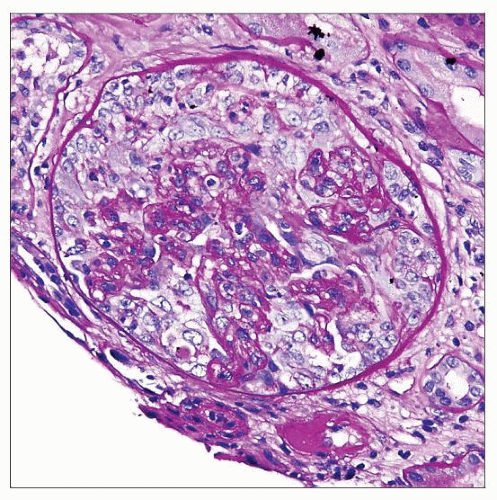
Histologic Features
Glomeruli
Wide range and extent of glomerular lesions with crescents
Segmental to severe capillary tuft thrombosis
Fibrinoid necrosis with rupture of basement membranes
Accumulation of neutrophils and karyorrhexis of cells in areas of necrosis
Crescents in different stages of healing (such as cellular, fibrocellular, and fibrous types) may be seen in same biopsy
Cellular crescent is composed of mainly parietal epithelial cells and exuded inflammatory cells (more than 2-3 layers thick)
Segmental/small to large, sometimes circumferential cellular crescents in Bowman space
A few crescents acquire granulomatous appearance with epithelioid and giant cells
Varying degrees of glomerular tuft compression
Acute and subacute periglomerular inflammation due to disruption of Bowman capsule
No intraglomerular cell proliferation
Later glomerulosclerosis, residual disruption of Bowman capsule
Tubulointerstitium
Mild to marked active interstitial inflammation may accompany glomerular crescentic lesions
Sometimes necrotizing neutrophilic granulomatous interstitial nephritis with palisading histiocytes (geographic pattern) or mass lesion
Occasional interstitial (extravascular) granulomas
Plasma cells can be prominent
Focal microscopic interstitial hemorrhages
Tubular red blood cells and RBC casts
Active tubulitis and epithelial cell injury
Peritubular capillaritis
Tubular atrophy and interstitial fibrosis
Vessels
Interlobular arteries are usual site affected by vasculitis
Segmental or circumferential fibrinoid necrosis
Cellular reaction composed of neutrophils, histiocytes, and sometimes prominent eosinophils
Occasional granulomatous inflammation
Smaller arteries down to pre- and postglomerular arterioles and venules involved
Isolated or concomitant medullary inflammation, capillaritis, and interstitial hemorrhages
Progressive vascular sclerosis with variable loss of elastic lamina by EVG stain
General comments
Vascular lesions and granulomata are more difficult to find in renal biopsies than in larger samples or autopsy kidneys
Small vessel vasculitis and capillaritis also seen in skin, lung, and other organs similar to other small vessel or ANCA-associated vasculitides
Other Organs
Lung
Pulmonary (nodular), extravascular granulomatous inflammation is a hallmark lesion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree