http://evolve.elsevier.com/Edmunds/NP/
Therapeutic Overview
The adrenal cortex synthesizes and secretes several hormones. Among them are the glucocorticoid cortisol, the mineralocorticoid aldosterone, and a small amount of the sex steroid androgen. Aldosterone, under the influence of the renin-angiotensin system and other metabolic pathways, regulates sodium, potassium, and water retention in the body. Cortisol has a powerful antiinflammatory effect, modifies the body’s immune response, and influences metabolic processes. The production of cortisol is controlled by a negative feedback loop involving the hypothalamus-anterior pituitary-adrenal cortex (HPA) axis (Figure 51-1). A low level of plasma cortisol stimulates the anterior pituitary to increase production of ACTH, which, in turn, stimulates the adrenal cortex to increase cortisol secretion. Similarly, a high level of circulating cortisol prompts downregulation of ACTH production and a resultant decrease in adrenal cortex production of cortisol.
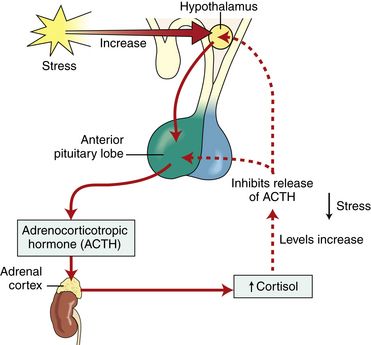
FIGURE 51-1 Adrenal-pituitary axis. From McKenry LM et al: Pharmacology in nursing, ed 22, St Louis, 2006, Mosby.
Cortisol is naturally secreted in an uneven pattern over 24 hours, totaling 10 mg/day in normal adults. Secretion is highest during the early morning hours—2:00 to 7:00 AM—and lowest in the evening—6:00 PM to midnight.
Mechanism of Action
Glucocorticoids affect the metabolism of carbohydrates, proteins, and fats. They have direct and indirect effects on immune response, modulate inflammatory response, and play a role in the body’s response to stressful stimuli (i.e., fasting states). All drugs in this class are remarkably similar and may be discussed as a group; the most important differences between these drugs consist of duration of action and degree of inherent mineralocorticoid activity, which causes sodium and fluid retention (Table 51-2). Mineralocorticoid activity is needed in adrenal insufficiency but not in severe inflammation. Both cortisone and hydrocortisone have glucocorticoid and mineralocorticoid properties. Their synthetic analogs prednisone, prednisolone, and methylprednisolone have both effects as well, although glucocorticoid effects predominate. By contrast, triamcinolone, dexamethasone, and betamethasone have exclusively glucocorticoid antiinflammatory activity.
TABLE 51-2
Pharmacokinetics of Selected Glucocorticoids
Modified from Brunton LL, Chabner B, Knollman B, editors: Goodman & Gilman’s the pharmacological basis of therapeutics, ed 12, New York, 2010, McGraw-Hill.
Carbohydrate and Protein Metabolism
Glucocorticoids maintain an adequate level of serum glucose by stimulating gluconeogenesis in the liver and inhibiting peripheral glucose use. They also stimulate protein breakdown, which results in increased plasma amino acid levels. In the liver, amino acids enhance enzymatic activity, which, in turn, supports increased glycogen deposition and decreased glycolysis. This action, intended to support homeostasis in the healthy body, can result in a diabetogenic state when large doses of exogenous glucocorticoids are used. Serum glucose rises in the fasting state; glucose tolerance decreases; insulin resistance develops; and glucosuria may be present. The result may be the clinical expression of latent diabetes or simply relative glucose intolerance while on steroid therapy.
Increased protein breakdown mobilizes amino acids from muscle, bone, skin, and lymph tissue. Muscle atrophy, osteoporosis, impaired wound healing, and thinning of the skin may result. In children, growth can be impaired.
Lipid Metabolism
Glucocorticoids affect the mobilization of fats from areas of deposition. Increased lipolysis occurs in areas of adipose accumulation, and serum fatty acid concentration increases. Long-term use of steroid therapy may result in increased deposition of adipose tissue in the back of the neck and in the supraclavicular area, sometimes described as a buffalo hump, and in the cheeks and the face, referred to as a moon facies. Relative loss of subcutaneous fat in the extremities may be noted.
Immune Response
Glucocorticoids mask the manifestations of both cellular and humoral immunity. Humoral immunity involves the interaction of B lymphocytes with macrophages and helper T-lymphocytes to create antibodies. Glucocorticoids do not cause a decrease in the level of circulating antibodies but may inhibit antibody creation by interfering with macrophage function and the production and activation of lymphokines. Cellular immunity is mediated primarily by T-lymphocytes. Glucocorticoids block several steps in the cascade of T-cell activation and thereby impede their ability to mount an effective cellular immune response. This action is used therapeutically to block rejection after transplant.
In addition, steroid administration has a direct effect on circulating white blood cells, causing a prompt drop in the numbers of lymphocytes, monocytes, and eosinophils in circulation and an increase in the number of circulating neutrophils. Lymphocytes are sequestered in lymph tissue, and T-cells are decreased in relatively greater numbers than B-cells. Neutrophils are released from the marrow in greater numbers and are removed from the circulation more slowly under the influence of exogenous glucocorticoids. The net result is a redistribution of white blood cell types rather than a true leukopenia.
Antiinflammatory Action
Lymphocytes, macrophages, and lymphokines all play a role in modulation of the body’s inflammatory response. Thus, the impact of exogenous glucocorticoids is an interactive one between the immune response and the inflammatory response. By many of the pathways mentioned earlier, glucocorticoids inhibit both early manifestations of inflammation, such as local edema, capillary dilation, migration and activation of white blood cells, and phagocytosis, and the later effects, including proliferation of capillaries and collagen deposition.
It is the simultaneous inhibition of inflammation and the immune response that accounts for the effectiveness of glucocorticoids in circumstances such as acute asthma and acute allergic reactions. However, the practitioner must remain cognizant of the attendant risks of such suppression. Serious infection or illness may be masked by the absence of the characteristic signs of inflammation or immune system activation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Key drug. Drugs listed in order of duration of action.
Key drug. Drugs listed in order of duration of action.