Learning Objectives
- Understand the history of global health and the role of forces and interventions that have helped shape the current state of health in the world
- Identify and discuss the major health problems and challenges facing the world today
- Propose and discuss suitable and promising solutions for these challenges to be considered by policymakers, planners, and health workers around the world
Defining Global Health
There are many different views on the definitions of “global health.” To emphasize the need for collaborative actions across nations and geographic boundaries, Beaglehole and Bonita1 proposed that Global Health is “collaborative trans-national research and action for promoting health for all.” Other authors2 have defined it as “health issues that transcend national boundaries and governments and call for actions on the global forces that determine the health of people.” Still others3 consider it to be the “worldwide improvement of health, reduction of disparities, and protection against global threats that disregard national borders.” Koplan and colleagues4 suggest that “The Global in global health refers to the scope of problems, not their location. Thus … global health can focus on domestic health disparities as well as cross-border issues.” They propose that “global health is an area for study, research, and practice that places a priority on improving health and achieving equity in health for all people worldwide.”
Although there is considerable overlap in the framework for action provided by several of the definitions, some experts make a distinction of terms with the assertion that international health primarily focuses on health issues in low-income countries, whereas public health focuses on the health of the population of a specific country or community. Others,5 however, challenge such distinctions and contend that global, international, and public health all attempt to address the same underlying social, economic, and environmental factors that affect the health of populations whether locally, nationally, or globally.
Historical Perspective
Throughout human history, numerous advances have improved the quality and longevity of life around the globe. Dating back to ancient civilizations, there is evidence of societies working to improve the health of the general public. The Babylonian sewage systems were among the first designed to protect the water supply from contamination and disease. The discovery of pasteurization by Louis Pasteur in the 1860s helped to ensure the safety of food supplies throughout the world. With the implementation of the constitution of the World Health Organization (WHO) in 1948, the mass tuberculosis (TB) immunization campaign with bacillus Calmette-Guérin vaccine in 1950, and the onset of the Malaria Eradication Program in 1955, many of the important developments related to global health in modern times occurred in the post–World War II period of the 1940s and 1950s. In 1980, smallpox was officially eradicated from the planet, and although polio and measles have not yet been eradicated, rapid progress is being made globally toward the goal of entirely protecting children and communities from these once debilitating diseases.
Prior to these developments of the second half of the 20th century, improvements in living conditions and the availability of new technologies had already had a remarkable effect on the quality of life and health indicators in the industrialized countries of Europe, North America, and the Oceania. Public health is credited with adding almost 30 years to the life expectancy of people in the United States in the last century and more than 22 years elsewhere in the world. As a testament to the remarkable contributions of the field of public health for all peoples around the world, in 1999 the Centers for Disease Control and Prevention (CDC) formulated its list of 10 great public health achievements in the 20th century.6 An expanded list of public health milestones is shown in Table 1-1.
Immunizations |
Control of infectious diseases |
Pasteurization |
Fluoridation of drinking water |
Maternal-child interventions |
Family planning |
Wastewater systems |
Prevention and treatment of heart disease and stroke |
Motor vehicle safety |
Workplace safety |
Safer and healthier foods |
Tobacco control |
Reducing firearm-related injuries |
Preventing birth defects |
Compared with the collective impact of improved living conditions including nutrition, sanitation, housing, education, and income, the impact of disease-oriented medical care on the overall health status of a country has been relatively small. There is now widespread recognition of the inextricable link between health, development, and sociopolitical stability. Technological, socioeconomic, and political factors all contribute to the overall well-being of a community. Internal strife and protracted political conflicts in a country, in contrast, lead to socioeconomic instability that negatively affects the health and welfare of its citizens. Unfortunately, developing countries around the globe have track records of long-standing conflicts and widespread corruption. Every year billions of dollars are siphoned from developing countries to banks in developed countries. Some have suggested that improvement in the health status of populations, particularly those in developing countries, can occur only through sociopolitical change, a global outlook, and local empowerment. International aid agencies and voluntary groups are important partners in this effort. However, a lack of political will and geopolitical instability are major barriers in bringing about a positive change.
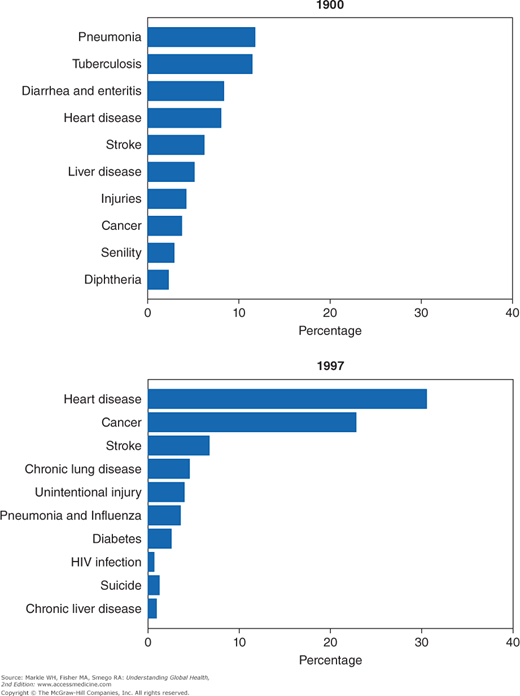
At the beginning of the 20th century, the most important public health problems throughout the world were largely infectious in nature. The life expectancy for a citizen living in the United States was 45.2 years, and the five leading causes of death were influenza and pneumonia, tuberculosis, diarrhea and enteritis, heart disease, and stroke (Figure 1-1). Life expectancy and median survival for persons residing in less developed countries was even less. However, 100 years later, life expectancy and health status of people all over the world had dramatically improved. In 2009, the average Japanese was living 83 years, the average American 79 years, the average Norwegian 81 years, and the average Malaysian 73 years. Many of the impoverished countries in Africa, Asia, and Latin America also made impressive public health gains in the last 100 years.7
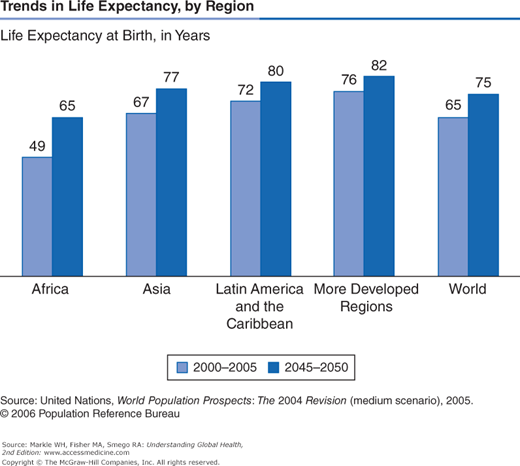
Unfortunately, these gains have not been uniformly distributed across continents or among countries on the same continent. In some developing countries marred by poverty and political strife, the achievements in socioeconomic conditions and health indicators have been less than dramatic. In 2009, the average life expectancy of a person in Afghanistan was 48 years, in Bangladesh 65 years, in Chad 48 years, and in Guatemala 69 years (Figure 1-2). Sadly, the human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) pandemic, with its epicenter in Africa during the 1980s and 1990s, has contributed to huge setbacks in longevity in much of the African continent and elsewhere in the 30 years since its recognition. For example, the life expectancy of a Ugandan man was approximately 47.4 years in 1980–1985, 39.7 years in 1985–1990, and 38.9 years in 1995–2000. In 2009, the life expectancy of a Ugandan man had climbed back to only 48 years.7
In the transition to modernity, global populations are trading one set of diseases for another. In many countries, improved socioeconomic conditions that led to a reduction in the prevalence of infectious diseases and associated reductions in morbidity and mortality have led to a tremendous increase in lifestyle-related diseases such as obesity, coronary artery disease, hypertension, and diabetes. In most middle-income and lower-income countries in Asia, Africa, and Latin America, both communicable (e.g., pneumonia, diarrheal diseases, HIV/AIDS, tuberculosis, and malaria) and noncommunicable diseases (heart disease, cancer, diabetes) concurrently present major public health challenges as these countries continue their developmental, demographic, and epidemiologic transitions.
The leading causes of mortality in most developed countries today are heart disease, cancer, stroke, chronic lung disease, and unintentional injury. In 2009, these diseases collectively accounted for 64% of all deaths in the United States, whereas pneumonia, influenza, and HIV/AIDS account for only 4.5% of annual deaths. However, the UN Population Division estimates that “group 1 diseases,” which include maternal, perinatal, nutritional, and communicable diseases, are largely responsible for a reduction of more than 15 years of life expectancy in African countries. If developed countries’ levels of group 1 diseases could be achieved in African countries, their life expectancy at birth would rise to about 72 years.8-10 In all parts of the globe there is a transition taking place from first-generation or “group 1,” diseases (e.g., common childhood infections, malnutrition, and reproductive risks) to second- (e.g., cardiovascular and cerebrovascular diseases, cancers, and degenerative diseases) and third-generation diseases (e.g., violence, drug abuse, and mental and psychosocial illness).11 With this background, in the following sections we discuss some of the notable public health achievements and global health challenges.
Global Health Achievements and Challenges
The 19th-century shift in population that accompanied industrialization and migration from countryside to cities led to overcrowding in poor housing served by inadequate or nonexistent public water supplies and waste-disposal systems. These conditions resulted in repeated outbreaks of cholera, dysentery, TB, typhoid fever, influenza, yellow fever, and malaria. Global urbanization accelerated dramatically during the last 4 decades of the 20th century, putting more and more people at risk for large-scale disease outbreaks. In 1960, an estimated 70% of the world’s population lived in rural areas. Today, almost the same percentage lives in cities and large metropolitan areas. In 1994, the city of Shanghai, China, experienced an outbreak of viral hepatitis A involving more than 400,000 cases. Throughout the Indian subcontinent, virtually every major city has experienced outbreaks of viral hepatitis E linked to contaminated municipal water systems, involving up to 200,000 persons per outbreak.
Public health control of infectious diseases after 1900 was based on the 19th-century discovery of microorganisms as the cause of many serious diseases such as cholera and tuberculosis.12,13 Successes in disease control resulted largely from improvements in sanitation and hygiene, the discovery of antibiotics, and the implementation of universal childhood vaccination programs. Scientific and technologic advances played a major role in each of these areas and are the foundation for today’s disease surveillance and control systems. In Western countries, the incidence of many infectious diseases began to markedly decline by 1900 because of public health improvements, implementation of which continued into the 20th century.
In Western countries, deaths from infectious diseases continued to decline at a steady pace during the 20th century. In particular, there has been a remarkable drop in infant and child mortality and a 29.2-year increase in life expectancy. For example, in the United States in 1900, 30.4% of all deaths occurred among children younger than 5 years; in 1997, that percentage was only 1.4%. In 1900, the three leading causes of death were pneumonia, tuberculosis, and diarrhea and enteritis, which (together with diphtheria) caused a third of all deaths. Of these deaths, 40% were among children younger than 5 years. In 1997, heart disease and cancers accounted for 54.7% of all deaths, with less than 5% attributable to pneumonia, influenza, and HIV infection.6
Despite this remarkable progress, infectious diseases remain among the greatest threats to persons living in developing countries of the world. More than 60% of children who die under the age of 5 die because of pneumonia, diarrhea, or measles. Together, pneumonia and diarrhea are still responsible for 40% of childhood deaths in the world, and only 39% of children with diarrhea receive oral rehydration therapy.14 Even as the number of TB cases is at an all-time low in the United States, the global prevalence of tuberculosis is at an all-time high, with about 8 million new cases and 3 million deaths annually.7 HIV/AIDS has become the most devastating epidemic in human history, supplanting the 1918 influenza pandemic that resulted in 20 million deaths. Since 1981, an estimated 33 million lives have been lost to HIV/AIDS, and almost 35 million more persons are believed to be infected worldwide, especially in sub-Saharan Africa, India, and Southeast Asia.15-17 This pandemic is still in progress. In addition, more than 30 new diseases were discovered in the last 30 years (Table 1-2), demonstrating the volatility of infectious diseases and the unpredictability of disease emergence. Many of the emerging infectious diseases, such as avian flu, severe acute respiratory syndrome (SARS), and hemolytic uremic syndrome, are zoonotic.
Avian influenza |
Acanthamebiasis |
Australian bat Lyssavirus |
Babesiosis |
Bartonella henselae |
Coronaviruses/Severe acute respiratory syndrome (SARS) |
Ehrlichiosis |
Hantavirus pulmonary syndrome |
Helicobacter pylori |
Hendra or equine morbilli virus |
Hepatitis C virus |
Hepatitis E virus |
HIV/AIDS |
Human herpesvirus 8 |
Human herpesvirus 6 |
Human T-cell lymphotropic virus I |
Human T-cell lymphotropic virus II |
Borrelia burgdorferi |
Microsporidia |
Encephalitozoon cuniculi |
Encephalitozoon hellem |
Enterocytozoon bieneusi |
Nipah virus disease |
Parvovirus B19 |
Variant Creutzfeldt-Jakob disease |
In many urban and rural areas of Asia, Africa, and Latin America, basic public health services such as provision of clean drinking water, sewage and solid waste disposal, food safety, and public education about hygienic practices (e.g., food handling and hand washing) are still lacking or inadequate. These deficiencies contribute to a continued global burden of major waterborne and foodborne diseases such as acute diarrheal illness (responsible for approximately 1.9 million deaths every year), viral hepatitis, enteric fever, and brucellosis. A third of the world’s population suffers from diseases caused by unsafe food, and many of these people experience long-term complications or death. Furthermore, animal and pest control programs are inadequate worldwide and contribute to the persistence of diseases such as malaria, rabies, viral encephalitis, trypanosomiasis, plague, and anthrax.7,9,10
Antibacterial drugs have been in civilian use for more than 60 years and have saved the lives of millions of individuals with streptococcal and staphylococcal infections, gonorrhea, syphilis, and other infections. Drugs have also been developed to treat viral diseases (e.g., herpes and HIV infection), fungal diseases (e.g., candidiasis and aspergillosis), and parasitic diseases (e.g., malaria). Penicillin, discovered fortuitously by Sir Alexander Fleming in 1928, was not developed for medical use until the 1940s, but it soon changed the face of medicine. The drug quickly became a widely available medical product that provided effective treatment for previously incurable bacterial illnesses, with a broader spectrum and fewer side effects than sulfa drugs.
Successes in reducing morbidity and mortality from infectious diseases during the first three quarters of the 20th century led to complacency about the need for continued research into the treatment and control of infectious microbes. However, the global appearance of AIDS, the emergence of multidrug-resistant (MDR) TB and extensively drug-resistant (XDR) TB, and an overall increase in infectious disease mortality during the 1980s and 1990s have provided additional evidence that as long as microbes can evolve, new diseases will appear.
Molecular genetics has provided valuable insights into the remarkable ability of microorganisms to evolve, adapt, and develop drug resistance in an unpredictable and dynamic fashion. Resistance genes are transmitted from one bacterium to another on plasmids, and viruses evolve through replication errors, reassortment of gene segments, and by crossing species barriers. Recent examples of microbial evolution include the development of a virulent strain of avian influenza in Hong Kong (1997–1998)18 and the MDR W strain of Mycobacterium tuberculosis in the United States in 1991. The emergence of vancomycin-intermediate Staphylococcus aureus (VISA), vancomycin-resistant S. aureus (VRSA), and extensively drug-resistant gram-negative bacterial infections have become major causes of global concern among clinicians and microbiologists.
The increased development and use of antimicrobial agents has hastened the development of drug resistance. The emergence of drug resistance in many microorganisms is reversing some of the therapeutic miracles of the last 50 years and underscores the importance of disease prevention. Antimicrobial multidrug resistance is a serious and growing problem worldwide for community-based infections caused by Plasmodium species, M. tuberculosis, Streptococcus pneumoniae, Salmonella, and Campylobacter species, Neisseria gonorrhoeae, Helicobacter pylori, and HIV, as well as for nosocomial infections due to staphylococci, enterococci, Enterobacteriaceae, Clostridium difficile, and systemic fungi. (See Chapter 12 for more information on antimicrobial resistance.)
For continued success in controlling infectious diseases, the global public health system must prepare to address diverse challenges including the emergence of new infectious diseases, the reemergence of old diseases (sometimes in drug-resistant forms), large foodborne outbreaks, and acts of bioterrorism. Continued protection of health requires improved capacity for disease surveillance and outbreak response at the local, state, national, and global levels; the development and dissemination of new laboratory and epidemiologic methods; continued development of antimicrobial agents and vaccines; and ongoing research into environmental factors that facilitate disease emergence.19 The global public health response to the SARS outbreak in 2004 and avian flu in 2010 demonstrated unprecedented cooperation in surveillance and dissemination of information. Ongoing research into the possible role of infectious agents (e.g., Chlamydia trachomatis, viruses) in causing or intensifying certain chronic diseases such as type 1 diabetes mellitus, some cancers, and atherosclerotic heart disease is also imperative.
Vaccine development to prevent the spread of communicable diseases is probably the single most important achievement in biomedical science and the most effective public health intervention in the history of humankind. At the beginning of the 20th century, infectious diseases exacted an enormous toll on the global population. It has only been since the middle of the 20th century that unprecedented achievements in the control of many vaccine-preventable diseases have been made.20 The eradication of smallpox and the 95% or greater decline in morbidity and complications resulting from vaccine-preventable diseases included in the Expanded Program on Immunizations (EPI), initiated by WHO in 1974, attest to the remarkable efficacy of vaccines.
Although the first vaccine against smallpox was developed by Edward Jenner in 1796, more than 100 years later its use was still not widespread as evidenced by an outbreak in the United States between 1900 and 1904 that resulted in more than 48,000 cases in each of the 4 years. Four other vaccines—against rabies, typhoid, cholera, and plague—were developed late in the 19th century but were also not used widely by 1900. Since 1900, vaccines have been developed or licensed against 22 other diseases (Table 1-3). In 2012, an American child required 27 doses of vaccines by age 15 months to be protected against 14 childhood diseases.21
Disease | Year |
|---|---|
Smallpoxa | 1798b |
Rabies | 1885b |
Typhoid | 1896b |
Cholera | 1896b |
Plague | 1897b |
Diphtheriaa | 1923b |
Pertussisa | 1926b |
Tetanusa | 1927b |
Tuberculosis | 1927b |
Influenzaa | 1945c |
Yellow Fever | 1953c |
Poliomyelitisa | 1955c |
Measlesa | 1963c |
Mumpsa | 1967c |
Rubellaa | 1969c |
Anthrax | 1970c |
Meningococcal Meningitis | 1975c |
Pneumococcala | 1977c |
Adenovirus | 1980c |
Hepatitis Ba | 1981c |
Haemophilus Influenza Type Ba | 1985c |
Japanese B Encephalitis | 1992c |
Hepatitis Aa | 1995c |
Varicellaa | 1995c |
Lyme Disease | 1998c |
Rotavirusa | 1998c, 2006c,d |
Human Papilloma Virus | 2005c |
Herpes Zoster | 2006c |
In 1974, when EPI was launched by the WHO, less than 5% of the world’s children were immunized against the six initial target diseases—diphtheria, tetanus, pertussis (whooping cough), polio, measles, and tuberculosis—during their first year of life. Until then, immunization programs had been largely restricted to industrialized countries, and even there they were only partially implemented. By 1990, and, after a slight interim drop in coverage rates, again in recent years, almost 80% of the 130 million children born each year were immunized before their first birthday. In 2010 alone, 109 million children under the age of 1 year were inoculated with the three doses of the diphtheria-tetanus-pertussis (DTP3) vaccine.22
As coverage for each of the childhood vaccines has increased, now involving over 500 million immunization contacts with children every year, there has been a corresponding drop in the incidence of the targeted infectious diseases. The EPI (which today includes yellow fever and hepatitis B vaccines) now prevents the deaths of at least 3 million children a year. In addition, at least 750,000 fewer children are blinded, physically disabled, or mentally retarded as a result of vaccine-preventable diseases. Indeed, WHO’s Millennium Development Goal # 4 (MDG4) essentially depends on widespread successful immunization of children to reduce by two thirds the global burden of under-5 mortality by the year 2015.22,23
The success of vaccination programs in the United States and Europe inspired the 20th-century concept of disease eradication, the idea that a carefully targeted disease could be eliminated from all human populations through global cooperation. In 1980, approximately a decade after it had been eliminated from the United States and the rest of the Western Hemisphere, smallpox was eradicated worldwide after a decade-long campaign involving 33 nations. International partnerships involving affluent industrialized nations, the WHO, and Rotary International are now seeking to eradicate polio. In fact, poliomyelitis caused by wild-type viruses has been nearly eliminated from all countries with the exception of Afghanistan, Nigeria, and Pakistan. Cases of measles and Haemophilus influenzae type b (Hib) among children younger than 5 years have been reduced to record low numbers. The disfiguring and debilitating disease known as dracunculiasis also shows the promise of being eradicated in the foreseeable future.23,24
Additional targets for disease control and eradication are presented by the relatively recent licensure of vaccines such as the seven-valent conjugated pneumococcal vaccine, tetravalent meningococcal vaccines, and the human papilloma virus vaccine. Anticipated new vaccines include those for influenza, parainfluenza, and chronic diseases (e.g., gastric ulcers and cancer caused by Helicobacter pylori, and rheumatic heart disease that occurs as a sequel to group A streptococcal infection). Given the constrained national health care resources in the 1990s, many developing countries were forced to re-examine epidemiologic data to set their infectious diseases priorities and choose between adding Hib or hepatitis B vaccine to their national EPI programs.24
Clinical trials are already Change to underway for a vaccine to prevent and/or treat HIV infection. The global immunization challenge of this century will be finding a way to finance the provision of an effective HIV vaccine for some of the poorest countries in the world where it is needed the most. Creative and innovative strategies to fund the worldwide distribution of an effective HIV vaccine, when it becomes available, are being aggressively discussed with potential funders such as the World Bank, the International Monetary Fund, and the Gates Foundation. The number of persons who will be candidates for a HIV vaccine will depend on whether the immunobiologic response is strictly preventive or therapeutic.
Additionally, efforts to control measles, which causes approximately 1 million deaths each year, and to expand rubella vaccination programs are also underway around the world. The use of existing vaccines in routine childhood vaccination programs worldwide must be expanded, and successful introduction of new vaccines must occur as they are developed. Such efforts regarding infectious diseases control and prevention can benefit both rich and poor countries by decreasing disease importations from developing countries. In the West, millions of cases of potentially preventable influenza, pneumococcal disease, and hepatitis B occur each year in adolescent and adult populations. New vaccines will be targeted at these age groups.
Despite the 3 million or so lives saved by DTP3 and measles vaccines every year and the high rates of immunizations reported in most countries,23 there are serious challenges in terms of disparities within and across countries. In particular, countries in South Asia and Africa face challenges that at times are referred to as the “fallacy of coverage.”25 Namely the challenges have to do with suboptimal age-appropriate immunizations, social and gender inequity in immunizations, poor access, women’s as well as both parents’ education, and low vaccine efficacy rates that in some areas were found to be as low as 41.5%. To deal with these and other challenges, in 2006 WHO and the United Nations Children’s Fund (UNICEF) launched a new initiative titled the Global Immunization Vision Strategy.22 Other challenges include strategies for hard-to-reach populations, evidence-based prioritization of global initiatives to introduce new vaccines, and strengthening and expansion of the global immunization and surveillance infrastructure.26
National treasuries and vaccine delivery systems must be capable of successfully implementing an increasingly complex vaccination schedule. As is true for other public health interventions, national and international efforts to promote vaccine use largely depend on public health infrastructure, economic development, and political stability. With the proper mind-set and establishment of priorities, even low-income countries can achieve remarkable rates of vaccination coverage for their populations.
An estimated 17.3 million deaths—or 30% of total global deaths in 2008—resulted from various forms of cardiovascular disease (CVD): ischemic or coronary heart disease, cerebrovascular disease or stroke, hypertension, heart failure, and rheumatic heart disease. Of these, 7.3 million deaths were due to ischemic heart disease, 6.2 million to cerebrovascular disease, and an additional 3.9 million to hypertensive and other heart conditions.27,28 At least 20 million people survive heart attacks and strokes every year, with a significant proportion of them requiring costly clinical care, which puts a huge burden on long-term care resources. CVD affects people in their midlife years, undermining the socioeconomic development not only of affected individuals but also of families and nations. Lower socioeconomic groups generally have a greater prevalence of risk factors, diseases, and mortality in developed countries. A similar pattern is emerging as the CVD epidemic matures in developing countries as well.
CVDs are no longer only a problem of the developed world. In 2005, some 80% of all CVD deaths worldwide took place in developing low- and middle-income countries, and these countries accounted for 86% of the global CVD disease burden. More than 60% of all coronary heart disease occurs in developing countries, partly as a result of increasing longevity, urbanization, and lifestyle changes. Furthermore, CVD is responsible for 10% of disability-adjusted life years (DALYs) lost in low- and middle-income countries and 18% in high-income countries. DALYs represent healthy years lost and indicate the total burden of a disease as opposed to simply the resulting death. The global burden of coronary heart disease is projected to rise from 46 million DALYs in 1990 to 82 million in 2020. The rise in the prevalence of CVD reflects a significant combination of unhealthy dietary habits, increased tobacco consumption worldwide, and reduced physical activity levels as a result of industrialization, urbanization, economic development, and food market globalization.7,28
More than half of the deaths and disability from heart disease and strokes each year can be reduced by a combination of simple cost-effective national efforts and individual actions to reduce major risk factors such as high blood pressure, diabetes mellitus, high cholesterol, obesity, and smoking. Obesity is one of the newest global epidemics, especially in developed and transitional countries. Because of obesity’s association with CVD and diabetes, obesity control and weight loss must be considered an important global strategy to improve the health and well-being of people all over the world.
The WHO, in collaboration with the CDC, is presently working to provide actionable information to develop and implement appropriate national and international policies related to the global epidemic of heart attack and stroke. As part of such efforts, the WHO has produced The Atlas of Heart Disease and Stroke,28 which addresses the problem of heart disease and stroke in a clear and accessible format for a wide audience. This highly valuable reference material has been designed for use by policymakers, national and international organizations, health professionals, and the general public. This picturesque atlas is in six parts: CVD, risk factors, the burden, action, the future and the past, and world tables.28
In the West, major milestones in the management of angina pectoris and heart attack, including expensive or invasive interventions such as diagnostic coronary angiography, thrombolytic therapy, statins, IIb/IIIa platelet receptor blocker drugs, percutaneous transluminal coronary angioplasty, coronary artery stenting, coronary artery bypass grafting, and ventricular assist devices, have resulted in impressive declines in mortality from these conditions in the past 2 decades. The technologic future holds even more promise for CVD treatment. However, these diagnostic and therapeutic services are largely inaccessible to the majority of populations living in Asia, Africa, and Latin America. No matter what advances are made in high-technology medicine, major global reductions in death and disability from CVD will only come from preventive measures involving modification of risk factors—not from cure. The most cost-effective methods of reducing risk are population-wide interventions combining effective economic, educational, and broad health promotion policies and programs emphasizing reduction in the dietary intake of fats, cessation of smoking, and salt restriction.
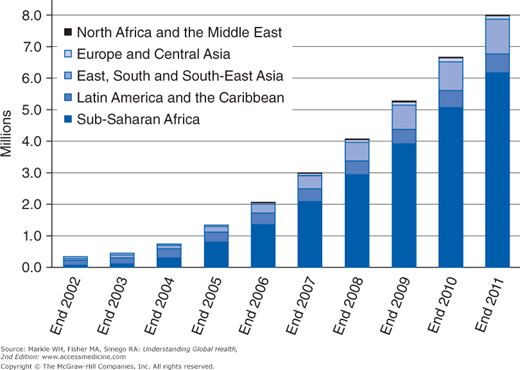
Much progress has been made since the early 1980s in improving our understanding of the etiology, epidemiology, natural history, and treatment of HIV/AIDS. Global efforts to combat the spread of AIDS have also become more organized and coordinated. In the last decade or so, more financial and pharmacologic resources have been made available to governmental and nongovernmental organizations internationally. For example, in 2004, only 700,000 people in low- and middle-income countries had access to antiretroviral treatment, but the number in 2011 had risen to 8 million (Figure 1-3). Since 2001, HIV incidence has fallen in 22 countries in sub-Saharan Africa and in 33 countries in the world. Also, the total number of AIDS-related deaths in the world fell from 2.2 million in 2005 to 1.8 million in 2010. In the developed world, the availability of antiretroviral treatment has led to a significant drop in morbidity, disability, and mortality resulting from AIDS. For example, the fixed-dose combination of two antiretroviral drugs, tenofovir and emtricitabine, is being used effectively to treat and prevent HIV infection. Combining the two agents into one tablet reduces the pill burden and increases compliance with antiretroviral therapy.
In the early days of this pandemic, a patient could not expect to live more than 6 months after being diagnosed with AIDS. Now most patients who have access to adequate treatment can expect to live for many years if not a full lifespan. Aside from effectively managing and treating the disease, the real goal is the development and widespread availability of a vaccine. Limited prophylactic success has been achieved with the use of topical microbicides among women. However, their widespread use poses many practical and cultural challenges.15-17
According to UNAIDS data, at the end of 2010 an estimated 34 million people in the world were living with HIV, which represents a 17% increase from 2001. This increase is largely due to improved access for AIDS patients to antiretroviral therapy.16,17 The UNAID 2011 World AIDS Day Report estimated that since 1997, 2.5 million deaths have been averted in low- and middle-income countries, and in 2010 alone, 700,000 AIDS-related deaths were averted. In 2010, there were 2.7 million new infections including 390,000 among children. The number of new infections was also down by 21% as compared with the peak in 1997. However, there were 7,000 new HIV infections every day in 2009 of which 97% were in low- and middle-income countries and 1,000 were in children under 15 years of age. Notably, between 2001 and 2010, AIDS-related deaths increased dramatically from 7,800 to 90,000 in Central Asia and Eastern Europe and from 24,000 to 56,000 in East Asia. Also, the number of AIDS-related deaths in the Middle East increased 60% in the same period from 22,000 to 35,000.7,15
Since 2004, the U.S. Global AIDS initiative, also known as the President’s Emergency Plan for AIDS Relief (PEPFAR), has made more than $30 billion available to combat the global HIV/AIDS epidemic. This program works in partnership with national governments and the private sector in more than 30 countries around the world, but primarily in Africa and the Caribbean. Despite many controversies about PEPFAR, by the end of 2008 the initiative is claimed to have supported, at least partly, antiretroviral treatment for more than 2 million people and averted 240,000 newborn infections and 1.1 million deaths worldwide.29,30
The HIV/AIDS epidemic has become a major obstacle in the fight against hunger and poverty in developing countries. Because most HIV-infected persons with AIDS are young adults who normally harvest crops, food production has dropped dramatically in countries with high HIV/AIDS prevalence rates. In half of the countries in sub-Saharan Africa, per capita economic growth is estimated to be falling by between 0.5% and 1.2% each year as a direct result of AIDS. Infected adults also leave behind children and elderly relatives who have little means to provide for themselves. In 2003, 12 million children were newly orphaned in sub-Saharan Africa, a number that rose to 14.8 million in 2010.31
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree