(1)
Department of Pathology, Medical College of Wisconsin, Milwaukee, Wisconsin, USA
Keywords
TeratomaMature teratomaImmature teratomaSeminomaYolk sac tumorChoriocarcinomaEmbryonal carcinomaGerm cell tumor with additional malignant componentGerm cell tumors are rare mediastinal lesions that are thought to originate from aberrant migration of germ cells to the thymus during embryogenesis. These tumors account for approximately 10–15 % of all mediastinal tumors and cysts. All types of germ cell tumors arising at other body sites (i.e., gonads, retroperitoneum, pituitary) have been described in the mediastinum. Teratomas, the most common type of germ cell tumor of the mediastinum, occur mostly in children or young adults. The vast majority of germ cell tumors originating from the mediastinum arise in the anterior compartment. Mediastinal germ cell tumors show a striking predilection for men. Most present with symptoms related to compression of surrounding structures. Malignant germ cell tumors of the mediastinum can secrete fetal oncoproteins, including alpha-fetoprotein (AFP) and human chorionic gonadotropin (HCG). Elevation of these proteins can be assessed easily by serology, aiding in the preoperative diagnosis. An important clinical association has been observed in patients with Klinefelter’s syndrome, who show an increased predisposition for the development of germ cell malignancy and hematologic abnormalities. An increased incidence of hematologic disorders such as acute leukemias, malignant histiocytosis, or systemic mastocytosis has also been observed in patients with mediastinal germ cell tumors.
The classification of germ cell tumors of the mediastinum has been controversial and has undergone various changes over the years. In general, most authors have applied classification schemes similar to those used for the gonadal counterparts of these tumors. The most recent classification (Moran and Suster, Primary germ cell tumors, 1997) divides these lesions into teratomatous and nonteratomatous lesions:
Teratomatous lesions
Mature teratoma
Immature teratoma
Teratoma with additional malignant component
Type I: teratoma + malignant germ cell tumor
Type II: teratoma + non-germ cell carcinomatous elements
Type III: teratoma + sarcomatous elements
Type IV: teratoma + any combination of the above
Nonteratomatous lesions
Seminoma
Yolk sac tumor
Choriocarcinoma
Embryonal carcinoma
Lesions showing combinations of any of the above
6.1 Teratomatous Lesions
Teratomatous lesions (Figs. 6.1, 6.2, 6.3, 6.4, 6.5, 6.6, 6.7, 6.8, 6.9, 6.10, 6.11, 6.12, 6.13, 6.14, 6.15, 6.16, 6.17, 6.18, 6.19, 6.20, 6.21, 6.22, 6.23, 6.24, 6.25, and 6.26) are mixed tumors composed of elements derived from all three germ cell layers, although tumors comprising elements from only one germ cell layer (“monodermal teratomas”) have also been accepted as teratomas. Most teratomas are composed of mature tissues and designated as mature teratoma. Tumors containing immature neural or mesenchymal elements have been designated as immature teratomas and are associated with a more aggressive clinical behavior. Both mature and immature teratomas can harbor an additional neoplastic, malignant component. In the past, such tumors were designated as “malignant teratoma” or “teratocarcinoma.” Such designations have been abandoned because they were, for the most part, either imprecise or misleading and did not denote the specific type of additional malignant component comprising the lesion. Such tumors are now designated “teratoma with malignant component”:
Type I: Teratoma with additional nonteratomatous germ cell tumor component (e.g., seminoma, yolk sac tumor, choriocarcinoma, embryonal carcinoma)
Type II: Teratoma with additional non-germ cell tumor carcinomatous (somatic) component (e.g., adenocarcinoma or squamous cell carcinoma)
Type III: Teratoma with additional sarcomatous component (e.g., rhabdomyosarcoma, leiomyosarcoma, chondrosarcoma, liposarcoma, angiosarcoma)
Type IV: Teratoma with additional malignant components that may be a combination of any of the above
Teratomas occur more often in children and young adults and present with symptoms due to compression of adjacent structures, although a significant number of patients may be asymptomatic, with tumors discovered incidentally on chest imaging studies. The most common elements encountered in mature teratomas are ectodermal derivatives such as skin and brain tissue, followed by endodermal derivatives such as gastrointestinal and respiratory mucosa, fat, bone, and cartilage. On imaging studies, the lesions are often cystic and may contain fluid levels; calcifications, metaplastic bone, and teeth often can be identified and may be helpful in the preoperative diagnosis.



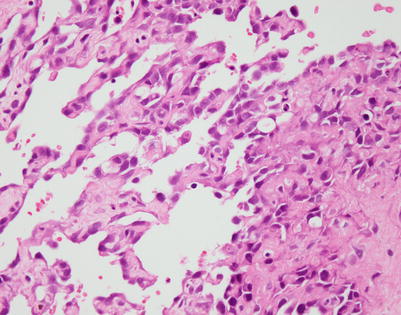

Fig. 6.1
Mature teratomas are grossly well circumscribed and encapsulated with a smooth and shiny outer surface. On cut surface, they can display a variegation of tissues based on the number of mature elements they contain
Fig. 6.2
Another example of mature teratoma of the mediastinum shows a well-circumscribed mass with a multicystic cut surface. The cysts were filled with clear mucinous or serosanguinous fluid
Fig. 6.3
Histologic appearance of a mature teratoma shows mature glial tissue (right) adjacent to a small, dilated glandular structure filled with keratinous debris
Fig. 6.4
Another example of a mature teratoma of the mediastinum, showing mature glial tissue containing an island of keratinizing, squamous epithelium in the center
Fig. 6.5
A frequent finding in mature teratoma of the mediastinum is the presence of exocrine and endocrine pancreatic tissue. In some instances, these elements may lead to symptomatic inflammation akin to acute pancreatitis

Fig. 6.6
Gross example of a monodermal teratoma of the mediastinum (“dermoid cyst”) showing a dilated cystic cavity containing dense grumous (sebaceous) material and hair
Fig. 6.7
Histologic appearance of a monodermal teratoma of the mediastinum showing a lining composed of well-developed epidermis with hair follicles and extrusion of keratinous debris and sebaceous material into the lumen
Fig. 6.8
Occasionally monodermal teratomas in the mediastinum will show only fibrosis and inflammation with scattered granulomas and fat necrosis. The granulomas are a reaction to extruded hair, which elicits a giant cell, foreign body-type reaction
Fig. 6.9
Immature teratomas of the mediastinum, containing immature elements that may arise from any of the three germ cell layers, are most common in children and young adults. The immature component most often encountered is the neuroepithelium, characterized by immature glandular structures surrounded by a spindle-cell to round cell stromal background
Fig. 6.10
Higher magnification of immature neural elements in immature teratoma shows neural tubules (arrows) surrounded by cellular, immature neural stroma. The greater the proportion of immature neural elements, the more aggressive the behavior of the lesion
Fig. 6.11
Another example of immature teratoma shows mature cartilage admixed with immature neural elements
Fig. 6.12
Higher magnification from an immature teratoma of the mediastinum shows detail of an immature neural tubule lined by primitive neuroepithelium

Fig. 6.13
Teratomas with additional malignant components (formerly known as “malignant teratoma” or “teratocarcinoma”) are rare lesions that can contain a variety of malignant elements in addition to the teratomatous elements. Grossly, they show a variegated cut surface with hemorrhage, necrosis, and foci of cystic degeneration. This example contains mature teratoma in addition to yolk sac tumor and seminoma
Fig. 6.14
Mediastinal teratoma with additional malignant component, type I, shows mature teratomatous elements admixed with foci of seminoma. The top part of the image shows a benign squamous pearl; below it are clusters and islands of round seminoma cells
Fig. 6.15
Mediastinal immature teratoma with additional malignant component, type I, shows immature neural elements (top right) and a diffuse seminomatous component (bottom left)
Fig. 6.16
Mediastinal teratoma with additional malignant component, type II, shows residual benign, mucin-secreting glands admixed with a poorly differentiated squamous cell carcinoma component with sarcomatoid transformation (spindling of the cells, bottom). The spindle tumor cells were also positive for low-molecular-weight cytokeratins
Fig. 6.17
Higher magnification from squamous cell carcinomatous component in teratoma with additional malignant component, type II, showing focus of incomplete keratinization
Fig. 6.18
Mediastinal teratoma with additional malignant components, type III, showing mature teratoma containing foci of angiosarcoma (arrow)
Fig. 6.19
Higher magnification from mediastinal teratoma with additional malignant component, type III, showing irregular, anastomosing vascular channels lined by atypical endothelial cells
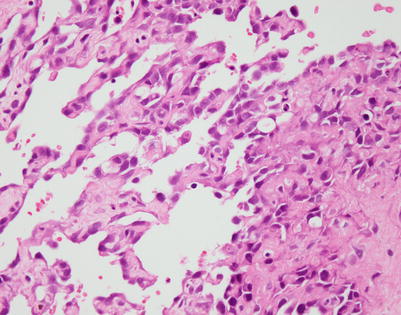
Fig. 6.20
At a higher power, the field in Fig. 6.19 shows large cells with hyperchromatic nuclei lining anastomosing vascular channels, characteristic of angiosarcoma. The tumor cells stained strongly with vascular-associated markers, including CD31, CD34, and FLI-1
Fig. 6.21
Mediastinal teratoma with additional malignant component, type III, showing a dilated glandular structure lined by columnar epithelium (right) and a well-circumscribed nodule (left) composed of an atypical, small round cell population corresponding to embryonal rhabdomyosarcoma
Fig. 6.22
Higher magnification from rhabdomyosarcomatous component in mediastinal teratoma with additional malignant component. There is a dense population of atypical, small, round blue cells harboring scattered larger cells with abundant pink cytoplasm
Fig. 6.23
At a higher power, the field in Fig. 6.22 shows a few scattered rhabdomyoblasts characterized by an abundant rim of intensely eosinophilic cytoplasm. The tumor cells stained strongly with desmin and showed nuclear positivity for Myo-D1
Fig. 6.24
Mediastinal teratoma with additional malignant component, type III, showing a focus of osteochondrosarcomatous differentiation. The two well-circumscribed nodules on the right show foci of chondrosarcoma; the nodules are surrounded by a highly atypical, sarcomatous spindle-cell proliferation
Fig. 6.25
At higher magnification, the third nodule in Fig. 6.24 shows an osteoid formation surrounded by atypical spindle-cell proliferation indicative of osteosarcomatous differentiation
Fig. 6.26
Mediastinal teratoma with additional malignant component, type IV, shows a tumor displaying a combination of yolk sac tumor (glandular structure, right) surrounded by highly atypical spindle-cell proliferation corresponding to rhabdomyosarcomatous elements. Other sections showed more conventional mature teratomatous elements and foci of seminoma
6.2 Nonteratomatous Lesions
Nonteratomatous lesions comprise tumors resembling their gonadal counterparts, including seminoma, yolk sac tumor, choriocarcinoma, embryonal carcinoma, and mixed nonteratomatous germ cell tumors containing combinations of these types (Figs. 6.27, 6.28, 6.29, 6.30, 6.31, 6.32, 6.33, 6.34, 6.35, 6.36, 6.37, 6.38, 6.39, 6.40, 6.41, 6.42, 6.43, 6.44, 6.45, 6.46, 6.47, 6.48, 6.49, 6.50, 6.51, 6.52, 6.53, 6.54, 6.55, 6.56, 6.57, 6.58, 6.59, 6.60, 6.61, 6.62, 6.63, 6.64, 6.65, 6.66, 6.67, 6.68, 6.69, 6.70, 6.71, 6.72, 6.73, 6.74, 6.75, 6.76, 6.77, 6.78, 6.79, 6.80, 6.81, 6.82, 6.83, 6.84, 6.85, 6.86, 6.87, 6.88, 6.89, 6.90, 6.91, 6.92, 6.93, 6.94, 6.95, 6.96, 6.97, and 6.98). Nonteratomatous tumors are more common in young adults and occur almost exclusively in males; only a few case reports of these tumors in women have been described.