Genitourinary Tract Trauma
Jack W. McAninch
Viraj A. Master
Introduction
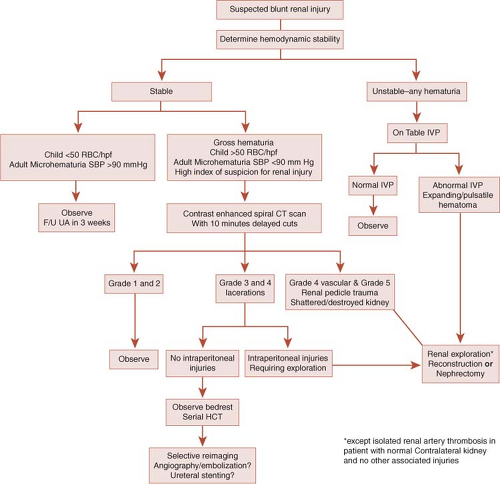
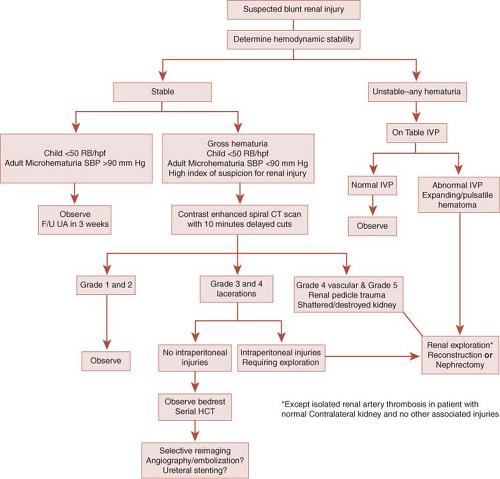
The genitourinary system, encompassing the kidney, ureter, bladder, urethra, and external genitalia are commonly injured in both blunt and penetrating trauma. Approximately 10% of all traumatically injured patients seen in the emergency department involve the genitourinary system, with the renal injuries occurring 1% to 5% of the time, and these injuries may be hard to identify. Early, thorough assessment allows for accurate staging, which then guides treatment and is essential in preventing serious complications. The intervening time period since the publication of the last edition of this volume has seen an additional systematic data review of urethral trauma of a large international scope, and using engineering approaches to diverse urologic problems such as predicting urethral injury during different pelvic fracture patterns and examination of renal injuries from direction of motor vehicle collisions. In this chapter, an evidence-based approach to diagnosis and management continues to be used. A detailed analysis of all genitourinary trauma articles published worldwide between 1966 and 2002 was conducted by an invited panel of surgeons (and chaired by J.W. McAninch) with subspecialty interests in traumatic and reconstructive urology, which was convened by the World Health Organization at the 2003 Stockholm Société Internationale d’Urologie meeting. Each paper from the primary literature was analyzed according to their numerical level of evidence classification, from randomized prospective clinical trials to case reports. Consensus papers were written on trauma to each genitourinary organ, which are suggested, additional readings, with an updated monograph from 2009 on urethral trauma. Evidence-supported diagnostic algorithms for adult blunt injury and pediatric blunt injury are seen in Figures 1 and 2, respectively, while additional algorithms for injuries to specific areas of the genitourinary tract are presented later in the chapter.
Renal Trauma
The kidney is the most commonly injured genitourinary organ due to external trauma, found in approximately 1% to 5% of abdominal trauma cases. Advances in staging techniques resulting from increased use of CT scanning, as well as increased awareness, based on outcomes research of the kidney’s capacity for healing, have permitted the vast majority of these injuries to be successfully managed nonoperatively by the surgical consultant. Nonetheless, certain severely injured kidneys are best managed by exploration and reconstruction, with nephrectomy reserved for life-threatening hemorrhage or kidneys that have been injured beyond repair. Ultimately, the objective of managing these patients is to prevent significant hemorrhage and retain enough functioning nephron mass to avoid end-stage kidney failure. A secondary goal is to avoid complications specifically attributable to the traumatized kidney.
Staging of Renal Injuries
Approximately 90% of renal injuries result from blunt trauma—usually falls from great heights, motor vehicle accidents, and violent assaults. Most of these injuries are minor, and rarely require surgical exploration. At San Francisco General Hospital (SFGH), only 2% of all bluntly injured kidneys have required exploration or repair. Pediatric kidneys as well as congenitally abnormal kidneys (cystic kidneys, hydronephrotic kidneys) are more susceptible to major injury, secondary to blunt mechanisms. Although only 10% of renal injuries result from penetrating trauma, up to 55% of these injuries will require exploration or repair. This is usually due to a more severe renal injury, associated intra-abdominal injuries, incomplete preoperative radiographic staging, or a combination of these factors.
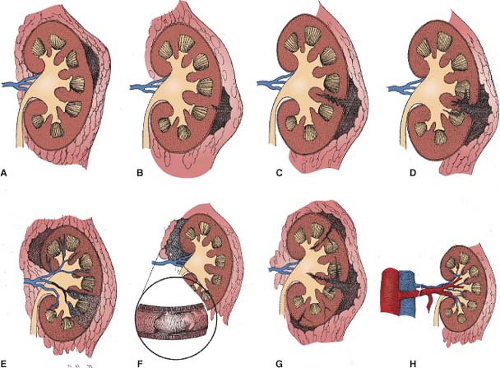
The American Association for the Surgery of Trauma (AAST) has created a renal organ injury scale which correlates with patient outcomes, and permits appropriate and selective management to be undertaken (Table 1). The renal injury classification is one of the few classification schemes which has been prospectively validated and found to correlate directly with need for surgical intervention. Moreover, recently, in 2010, it has been demonstrated that the AAST renal injury score predicts the degree of renal dysfunction. Grade 1 injuries include subcapsular hematomas and renal contusions (Fig. 3). Grade 2 injuries involve small lacerations into the renal cortex. Grade 3 injuries extend through the corticomedullary junction. Grade 4 injuries consist of either injury into the collecting system, or renal vascular injuries such as main renal artery or vein injury with contained hemorrhage, or segmental vessel injury. Grade 5 injuries include kidneys with pedicle avulsion off the great vessels, as well as completely shattered kidneys.
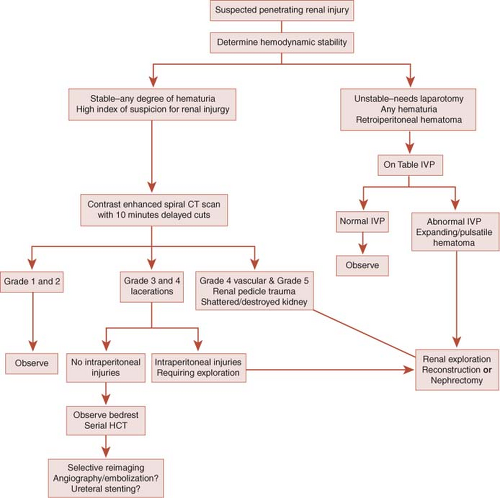
Clinical staging begins with history and physical examination, including determining whether the patient has been in shock as well as assessing for presence of hematuria. Based upon these criteria, a subset of patients likely to have significant renal injury may be identified. This subset may then undergo radiographic staging in order to completely stage the injury and determine whether operative management is indicated (Figs. 4 and 5).
History should focus on the mechanism of trauma (blunt [Fig. 4] or penetrating [Fig. 5]), as well as presence of significant deceleration—which should raise suspicion for significant renal injury. In penetrating trauma, knowledge of type of bullet (high vs. low velocity) or knife used in the assault may assist in prediction of degree of renal injury. On physical examination, the presence of shock (defined as systolic blood pressure <90 mm Hg) should be recorded. The lowest recorded systolic blood pressure is critical in determining the need for radiographic imaging in adult blunt renal trauma. Clearly, a patient in shock who cannot be resuscitated may require urgent laparotomy, thus bypassing radiographic staging of suspected renal injury and will require intraoperative staging. The abdomen, flank, and back should be carefully examined. Flank tenderness or ecchymosis as well as lower rib fractures may indicate underlying renal injury. In penetrating trauma, entry and exit wounds may be a helpful indicator that the kidney has been injured.
Hematuria is the most common sign of penetrating and blunt renal trauma. Importantly, however, the presence of hematuria and degree of hematuria does not correlate consistently with degree of renal injury. This is particularly true in penetrating injuries, where a significant percentage of patients with significant renal injuries may have no hematuria. It is imperative that the first voided or catheterized specimen should be analyzed, because hematuria may clear
rapidly. Either dipstick or microscopic analysis may be performed.
rapidly. Either dipstick or microscopic analysis may be performed.
Radiographic Staging
Using the clinical information outlined above, the indications for radiographic imaging may be tailored to detecting patients with a significant chance of having a major renal laceration (AAST Grade 3–5). Based upon experience at SFGH, we recommend imaging the following categories of patients, although it must be emphasized that clinical judgment continues to be paramount:
0Penetrating trauma: abdomen, flank, or back injury with any degree of hematuria, particularly when the course of the missile appears to involve the kidney or ureter.
Blunt trauma with either gross (visible) hematuria or shock (defined as any recorded systolic blood pressure below 90 mm Hg). Patients having sustained blunt trauma with microhematuria only can safely avoid renal imaging.
Blunt trauma in the setting of significant deceleration injury, for example, falls from heights or motor vehicle accidents. This mechanism of injury has been associated with a higher incidence of ureteropelvic junction (UPJ) disruption as well as renovascular trauma.
Pediatric penetrating injury or blunt trauma with microhematuria greater than 20 RBC/HPF. There is increasing evidence that the adult imaging criteria outlined above will identify the majority of significant renal lacerations in children, but this remains controversial. The surgeon should continue to maintain a
low threshold for renal imaging in the pediatric population.
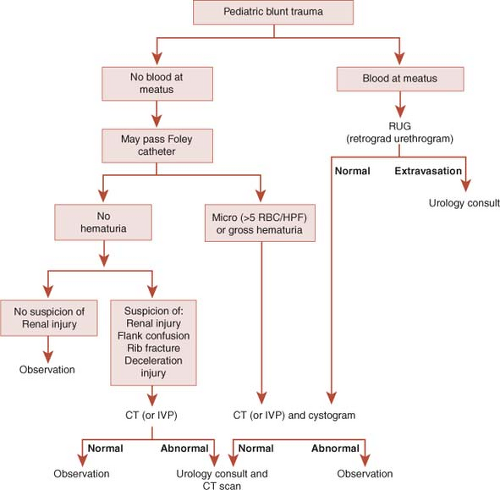 Fig. 2. Algorithm for staging blunt trauma in pediatric patients. CT, computed tomography; HPF, high-power field; IVP, intravenous pyelogram; RBC, red blood cell. |
Table 1 American Association for the Surgery of Trauma Organ Injury Severity Scale for Renal Trauma | |||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||
Contrast-enhanced computed tomography (CT) scanning has replaced Intravenous Pyelography (IVP) as the imaging modality of choice in renal trauma patients, but it must be emphasized that modern scanners are so rapid, a “delayed” CT 10 minutes after the initial CT is critical to detect renal pelvic or ureteral injuries down to the bladder. If this second scan is not possible, a plain abdominal radiograph (KUB) at this time may add complementary information to the CT scan. CT is noninvasive, and offers rapid and accurate detection of renal injuries, as well as associated injuries to other organs. CT defines depth and extent of lacerations, a functioning contralateral kidney, the presence of associated hematoma and contrast extravasation, which suggests injury through the collecting system, as well as any devitalized
renal parenchyma. Consideration must be given to each of these factors when deciding upon a treatment plan.
renal parenchyma. Consideration must be given to each of these factors when deciding upon a treatment plan.
While CT may accurately demonstrate parenchymal lacerations, it has limited use in staging renovascular injuries. A renal vein laceration may be suspected by the finding of hematoma, medial to the renal hilum. Adjunctive radiographic imaging techniques include renal ultrasound, nuclear scintigraphy, magnetic resonance imaging (MRI), and retrograde pyelography. None of these are recommended as first-line studies in the acute setting.
Indications for Surgical Exploration
A vast majority of renal injuries are contusions or minor lacerations, and may thus be managed nonoperatively if adequately staged. Appropriate radiographic staging has also permitted selective nonoperative management of major lacerations in both blunt and penetrating trauma (Figs. 4 and 5). In a recent series of grade 4 lacerations at SFGH, almost one-quarter were successfully managed nonoperatively. Penetrating injuries more commonly require laparotomy because of associated injuries or hemodynamic instability. In our experience, however, 55% of stab wounds and 24% of gunshot wounds were successfully managed expectantly through the use of careful selection and complete clinical and radiographic staging. In a series of gunshot wounds to 206 renal units, the renal salvage rate was 85%. But, if expectant management is selected in the setting of a major renal laceration, close monitoring with serial hematocrit measurements and liberal use of repeat imaging, especially at 36 to 48 hours is indicated.
The only absolute indication for surgical exploration in renal trauma is persistent, life-threatening hemorrhage believed to be from renal injury, renal pedicle avulsion, and expanding, pulsatile, or uncontained retroperitoneal hematoma. These patients often present in severe shock, and it is thus rare for these patients to have undergone radiographic staging prior to emergency laparotomy. In the setting of renal pedicle avulsion or a severely shattered kidney, reconstruction may be impossible, and nephrectomy may be lifesaving.
Relative indications for renal exploration include incomplete staging, devitalized
renal parenchyma, vascular injury, and urinary extravasation. In a hemodynamically unstable patient, radiographic assessment is not possible prior to laparotomy and there may be an unexpected retroperitoneal hematoma found at the time of laparotomy in the trauma patient. At this time, if the patients’ clinical condition permits, a single abdominal plain film taken 10 minutes after the bolus administration of 2 cc/kg of intravenous contrast, delivered as a bolus, in a normotensive patient, is quite helpful. This is known as a “one-shot” IVP. This film is most helpful for confirming the presence of a normally functioning contralateral kidney and may possibly help to diagnose the injury in the affected renal unit. In addition, all patients with penetrating trauma and incomplete preoperative staging and a retroperitoneal hematoma require exploration. Although the one-shot IVP may be indeterminate, a recent study found that it successfully obviated renal exploration in 32% of patients in whom it was required. Furthermore, this approach has not been found to increase the rate of unnecessary nephrectomy. The initial laparotomy is the optimal time for any required renal reconstruction, but must be emphasized that the entire clinical picture is to be taken into account, minding damage control principles, and should be expedient. Delayed exploration has resulted in nephrectomy rates as high as 50%.
renal parenchyma, vascular injury, and urinary extravasation. In a hemodynamically unstable patient, radiographic assessment is not possible prior to laparotomy and there may be an unexpected retroperitoneal hematoma found at the time of laparotomy in the trauma patient. At this time, if the patients’ clinical condition permits, a single abdominal plain film taken 10 minutes after the bolus administration of 2 cc/kg of intravenous contrast, delivered as a bolus, in a normotensive patient, is quite helpful. This is known as a “one-shot” IVP. This film is most helpful for confirming the presence of a normally functioning contralateral kidney and may possibly help to diagnose the injury in the affected renal unit. In addition, all patients with penetrating trauma and incomplete preoperative staging and a retroperitoneal hematoma require exploration. Although the one-shot IVP may be indeterminate, a recent study found that it successfully obviated renal exploration in 32% of patients in whom it was required. Furthermore, this approach has not been found to increase the rate of unnecessary nephrectomy. The initial laparotomy is the optimal time for any required renal reconstruction, but must be emphasized that the entire clinical picture is to be taken into account, minding damage control principles, and should be expedient. Delayed exploration has resulted in nephrectomy rates as high as 50%.
Parenchymal Injury
Significant amounts of devitalized renal parenchyma are often best managed by early surgical debridement. Expectant management of patients with devitalized fragments and associated intra-abdominal injury may
lead to a higher rate of abscess and infected urinoma formation, as well as delayed bleeding. Immediate exploration in this setting reduced the posttrauma complication rate from 82% to 23%. This result suggests that major renal lacerations with devitalized fragments and associated intra-abdominal injuries should be immediately repaired, particularly if a laparotomy is already planned by the trauma surgeon. In addition, patients with a major devitalized fragment associated with urinary extravasation and a significant hematoma are ultimately best treated by early exploration and reconstruction, even without concomitant intraperitoneal injury. However, the nonoperative approach in this situation may be more prudent for the surgeon who rarely undertakes renal exploration in the trauma setting, as the chance of unnecessary nephrectomy is increased.
lead to a higher rate of abscess and infected urinoma formation, as well as delayed bleeding. Immediate exploration in this setting reduced the posttrauma complication rate from 82% to 23%. This result suggests that major renal lacerations with devitalized fragments and associated intra-abdominal injuries should be immediately repaired, particularly if a laparotomy is already planned by the trauma surgeon. In addition, patients with a major devitalized fragment associated with urinary extravasation and a significant hematoma are ultimately best treated by early exploration and reconstruction, even without concomitant intraperitoneal injury. However, the nonoperative approach in this situation may be more prudent for the surgeon who rarely undertakes renal exploration in the trauma setting, as the chance of unnecessary nephrectomy is increased.
Urinary extravasation signifies collecting system violation secondary to a major renal laceration, but does not specifically mandate surgical repair. The collecting system may be violated at a fornix, a minor or major calyx, or even through the renal pelvis and UPJ. While the majority of lacerations into fornices and minor calyces will seal spontaneously, larger degrees of extravasation may leak for a prolonged period and are less likely to resolve spontaneously. Serial CT scans are mandatory in the management of these patients. The first scan should be obtained at approximately 36 to 48 hours post-injury in order to rule out the development of significant new complications. Intervention is indicated in the setting of sepsis, ongoing leakage, or significant urinoma formation. In these cases, placement of an indwelling ureteral stent or even a nephrostomy tube may speed resolution of extravasation. Lacerations of the renal pelvis usually do not resolve spontaneously, and should be surgically repaired. Similarly, UPJ avulsion mandates
surgical repair. These unusual injuries are more commonly found in the setting of deceleration injury or in children, but may also take place in adults with an undiagnosed congenital anomaly such as UPJ obstruction. CT findings which suggest UPJ avulsion include nonvisualization of the ipsilateral ureter and medial extravasation of contrast material. When a kidney injured by a gunshot wound shows continued extravasation at the time of the first repeat CT scan, the surgeon should also maintain a low threshold for repair. These injuries are often associated with significant devitalized parenchyma secondary to blast effect, especially when a high velocity missile has been used, and are unlikely to heal spontaneously.
surgical repair. These unusual injuries are more commonly found in the setting of deceleration injury or in children, but may also take place in adults with an undiagnosed congenital anomaly such as UPJ obstruction. CT findings which suggest UPJ avulsion include nonvisualization of the ipsilateral ureter and medial extravasation of contrast material. When a kidney injured by a gunshot wound shows continued extravasation at the time of the first repeat CT scan, the surgeon should also maintain a low threshold for repair. These injuries are often associated with significant devitalized parenchyma secondary to blast effect, especially when a high velocity missile has been used, and are unlikely to heal spontaneously.
Vascular Injury
Major injury to the main renal artery or vein usually requires operative management. These patients have higher rates of complications, renal loss, and mortality when compared to those with nonvascular renal injuries. CT findings consistent with main renal artery injury include lack of renal enhancement or abrupt cut-off of an enhancing artery. Segmental arterial injuries typically appear as wedge-shaped infarcts with the apex facing the renal hilum. Injuries to the main renal vein typically appear as central or large hematomas which may displace the kidney anteriorly. Vascular injuries typically occur secondary to deceleration trauma causing the disruption of the inelastic intimal layer with subsequent irreversible parenchymal ischemia and infarction.
Despite the ongoing advances in trauma care, successful renal salvage after major renovascular injury only occurs in 25% to 35% of cases, at best. Time to reperfusion is the major factor in determining the ultimate outcome. Renal function is significantly impaired following 3 hours of total and 6 hours of partial ischemia. Despite technically successful repair, late hypertension occurs in <50% of renal arterial injuries managed nonoperatively, compared to 57% which were revascularized. Renal arterial repair should be reserved for solitary kidneys, bilaterally injured kidneys, and in the rare situation of detection within 6 hours of injury. Endovascular stenting may have a limited role, as maintaining patency requires anticoagulation, which is rarely possible in the traumatically injured patient. If detection of renal artery thrombosis is delayed and laparotomy is otherwise indicated, nephrectomy should be performed at that time. Otherwise, the kidney may be allowed to atrophy, with delayed nephrectomy performed if hypertension develops.
Renal Exploration and Reconstruction
Proximal Vascular Control
Primary goals for exploration/reconstruction include control of renal hemorrhage, preservation of maximal parenchyma, and reduction of potential complications attributable to the injured kidney. Historically, renal exploration in the trauma setting usually resulted in total nephrectomy. Using a refined approach to proximal vascular control and a meticulous approach to reconstruction, it is possible to salvage the vast majority of injured kidneys requiring surgical exploration.
The reason behind unplanned nephrectomy in the trauma setting is uncontrolled hemorrhage. We therefore routinely obtain proximal vascular control prior to opening the retroperitoneal hematoma. While temporary vascular occlusion is rarely necessary (<17% of renal explorations at SFGH), there is no accurate method of determining which kidneys will require this maneuver during the subsequent reconstruction. Those who have presented series suggesting pedicle control can be safely obtained if necessary following release of the perinephric hematoma that have reported nephrectomy rates approximately three times higher than those with early vascular control.
The traumatized kidney should be explored through a midline transperitoneal incision extending from the xiphoid process to the pubic symphysis. Except in cases of renal pedicle avulsion, all associated intra-abdominal injuries (spleen, liver, pancreas, small and large intestine) should be addressed before renal exploration—thus allowing Gerota’s fascia to maintain its natural tamponade effect on the hematoma.
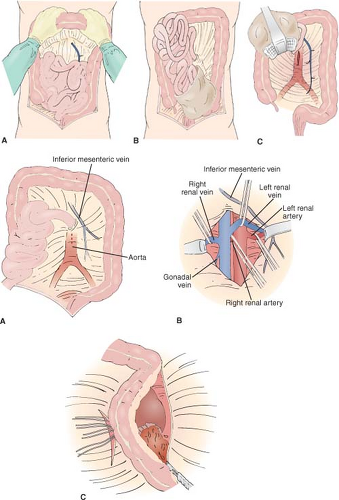
The approach to the injured kidney begins with proximal vascular control. A Bookwalter self-retaining retractor should be used if available. The transverse colon is wrapped in moist laparotomy sponges and placed on the chest (Fig. 6A). The small intestine is placed in a bowel bag and retracted superiorly and to the right. This exposes the root of the mesentery and the ligament of Treitz and the underlying great vessels. The retroperitoneal incision is made over the aorta superior to the inferior mesenteric artery, and extending up to the ligament of Treitz (Fig. 6B). If a large retroperitoneal hematoma obviates easy palpation of the aorta at the level of the ligament of Treitz, the incision may be made medial to the inferior mesenteric vein. This vein is an important guide, running a few centimeters left of the aorta. It is easily identifiable, even in the presence of a large hematoma. Dissection should be carried superiorly along the anterior wall of the aorta until the left renal vein is identified crossing anterior to it. This vessel is encircled but not occluded with a vessel loop, allowing for retraction. The encircled left renal vein serves as a guide to the remaining renal vessels, each of which then encircled in vessel loops. These vessels are all left unoccluded unless heavy bleeding is encountered during the renal dissection. In our experience, most bleeding is successfully controlled with manual compression alone. Temporary renal vascular occlusion should be kept below 30 minutes in order to minimize warm ischemic damage. After vascular control has been successfully achieved, the injured kidney may
be exposed by mobilizing the ipsilateral colon along the white line of Toldt and reflecting it medially. Gerota’s fascia is then incised along the lateral aspect of the kidney in order to completely expose the kidney. Care should be taken to maintain the integrity of the renal capsule as the kidney is mobilized in order to decrease hemorrhage and preserve the capsule for later closure.
be exposed by mobilizing the ipsilateral colon along the white line of Toldt and reflecting it medially. Gerota’s fascia is then incised along the lateral aspect of the kidney in order to completely expose the kidney. Care should be taken to maintain the integrity of the renal capsule as the kidney is mobilized in order to decrease hemorrhage and preserve the capsule for later closure.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree