KEY TERMS
Congenital defects are a major cause of death and disability in infants and children. Some 3 percent to 4 percent of newborns have a major abnormality apparent at birth. Other problems show up later; up to 7.5 percent of children are diagnosed with a congenital defect in their first five years.1 Such abnormalities may be inherited in the child’s genes, or they may be caused by birth injury or by the mother’s exposure to an infectious agent or toxic substance during pregnancy. Genes also play a role in many diseases of later life.
Because the birth of healthy children has been a high priority traditionally for public health, education and prenatal care for pregnant women have been encouraged. As more has been learned about how certain infectious agents, drugs, and chemicals can cause birth defects, greater public health efforts have been directed toward preventing women’s exposure to these substances. Until the past few decades, little could be done to prevent genetic abnormalities. Now, however, technological developments have opened up vast possibilities in the detection of defective genes. These discoveries have had many clear benefits, but they have also raised many difficult ethical questions.
Environmental Teratogens
Birth defects may be caused by a variety of environmental agents, called teratogens, which include some bacteria and viruses, various drugs and chemicals, and radiation. Many teratogens are also carcinogens, capable of causing cancer. In some cases, the teratogenic effect, like the carcinogenic effect, is known to be the result of mutation in the DNA. However, much less is known about the disruptions of fetal development that lead to birth defects than is known about carcinogenesis.
Infectious diseases known to damage the fetus include syphilis, rubella (German measles), and toxoplasmosis. Congenital syphilis, caused by bacteria passed from a mother to her fetus through the placenta, was a devastating disease of newborns before penicillin was discovered. The disease damaged the infants’ nerves, bones, and skin and often resulted in blindness and mental retardation. Beginning in the 1930s, many states required blood tests for syphilis—the Wasserman test—for all couples about to be married in an effort to identify and treat infected people before they could transmit the disease to a child.2 Most states have discontinued that requirement.
Rubella, ordinarily a mild disease of childhood, causes profound deafness in children whose mothers were infected by the virus while pregnant. Routine vaccination of children against rubella accomplishes the longer-term purpose of immunizing childbearing women, and the incidence of congenital deafness has been dramatically reduced. Toxoplasmosis, a parasitic disease that may go unnoticed in adults, can cause major neurological damage in the fetus. Since cats are a reservoir for the parasite and the route of transmission is most commonly through cat feces, toxoplasmosis is best prevented by education—warning pregnant women about the risks of contracting the disease through gardening and contact with litter boxes.
A pregnant woman’s exposure to teratogenic drugs and environmental chemicals can have very obvious results because the effects become apparent within nine months, dramatically altering a young life. One memorable tragedy occurred in the 1950s at Minamata, Japan, where a plastics factory contaminated the bay with high levels of mercury. A highly toxic form of the mercury accumulated in the fish, the staple of the community’s diet. While adults were relatively unaffected, many children were born with severe neurological deformities, including profound brain damage.3 The tragedy of Minamata, captured by the famous photographs of W. Eugene Smith and Aileen M. Smith, accessible on the Internet, alerted the world to the dangers of environmental pollution.4 Laws controlling air and water pollution and disposal of toxic wastes have been effective in preventing such disasters in the United States, but they continue to occur in other parts of the world, including the former Soviet Union.
Another famous teratogenic event was the epidemic of limb deformities that occurred in Europe and Australia in the early 1960s that was caused by the sedative thalidomide. Women who took the drug to relieve morning sickness gave birth to babies whose arms and legs were drastically shortened into flipper-like appendages.3 The United States escaped the epidemic because one skeptical Food and Drug Administration (FDA) official, Dr. Frances Kelsey, was suspicious of the drug and resisted great pressure from the manufacturer before the dangers became apparent. In 1998, in a controversial decision, thalidomide was approved by the FDA as an effective treatment for leprosy and some forms of cancer. However, it can be used only under very strict regulations that require women taking it to undergo monthly pregnancy tests and to use two forms of birth control.5
One of the FDA’s most important missions is to protect American citizens against such tragic side effects of drugs by prohibiting them entirely if their value is not judged to be worth the associated risks or by mandating clear communications about risks when there are also clear benefits. The antibiotic tetracycline, the anti-epilepsy drug Dilantin, the hormone diethylstilbestrol, and the acne medication Accutane are among the common prescription drugs that have been found by painful experience to cause birth defects. Pregnant women are now advised to refrain from taking any medication that is not absolutely necessary.
Alcohol was recognized to be a teratogen only in the 1970s. Although most cases of fetal alcohol syndrome have been identified in children of heavy drinkers, no level of alcohol has been judged safe for the fetus, and pregnant women are advised not to drink at all. Tobacco smoke increases the risk of premature birth and low birth weight, as well as sudden infant death syndrome. Cocaine and heroin use by pregnant women causes addiction in the fetus, bringing about painful withdrawal symptoms in the newborn and sometimes leaving permanent neurological damage.
Genetic Diseases
Essentially all the information required for the development of a new human being is contained in the genetic material located in the 46 chromosomes, half of which come from the mother’s egg and half of which come from the father’s sperm. Mistakes are common in the reproductive process. The most visible are chromosomal abnormalities, which can be seen under a microscope. Such defects cause a variety of malformations in the developing fetus, many of which are incompatible with survival. More than half of pregnancies in healthy women end in spontaneous abortion, and chromosomal abnormalities are obvious in many of these aborted fetuses.1 When the affected fetus does survive, the disability is usually profound, almost always including mental retardation and often leading to early death. Down syndrome, caused by an extra copy of chromosome 21, is the best-known disorder of this type, largely because its effects are less lethal than those of other chromosomal defects, and most affected infants survive.
The majority of genetic diseases are caused by defects that are not visible under a microscope. Those that are best known and understood are caused by a defect in a single gene inherited more or less according to classical Mendelian genetics (see FIGURE 12-1). In the first part of the figure, the pattern of inheritance of a dominant gene is shown. The father carries the gene for Huntington’s disease on one of a pair of chromosomes. The mother carries two normal genes. Half of the children will inherit the disease from the father. In the second part of the figure, the pattern of inheritance of a recessive gene is shown. Both parents carry one recessive gene, but neither parent has symptoms, and the parents may be unaware that they are carriers. One-quarter of the children will inherit two recessive genes and will have the disease. One-half the children will be carriers.
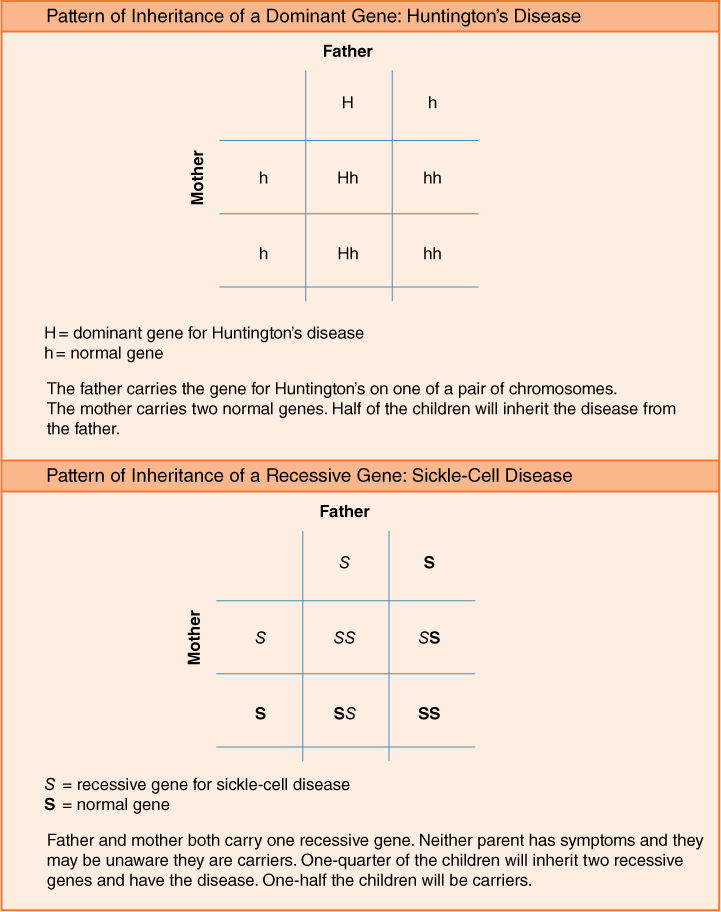
FIGURE 12-1 Mendelian Genetics
In sum, of the two copies of each gene that an individual inherits, one from each parent, the gene for a disease may be dominant or recessive. When the presence of a single copy is sufficient to cause the disease—an autosomal dominant disorder—the affected person will transmit that gene on average to half of his or her children. (Autosomal genes are on a non-sex chromosome.) Examples of autosomal dominant disorders are Huntington’s disease, a midlife deterioration of the brain whose best-known victim was the folk singer Woody Guthrie; achondroplasia, a type of dwarfism made famous by the French painter Toulouse-Lautrec; and Marfan syndrome, characterized by extreme height and cardiovascular abnormalities, which occasionally makes the news after the sudden death of an unsuspecting basketball player.1
Autosomal recessive disorders do not become obvious unless the individual inherits two copies of the gene. The disease may appear unexpectedly in a child of two parents who were unaware that they each carried one copy of the gene. The best-known autosomal recessive disorders tend to predominate in certain ethnic groups: Tay-Sachs disease in Jews of Eastern European descent, sickle-cell disease in Africans and African Americans, cystic fibrosis in people of northern European ancestry, and thalassemia in populations of Mediterranean or Asian descent.1
X-linked disorders, such as hemophilia and Duchenne’s muscular dystrophy, are caused by a defective gene on the female sex chromosome, called the X chromosome. These diseases occur predominantly in males. Since females have two X chromosomes, inheritance of the defective gene has minimal impact on them because of the second, normal gene’s presence. Males, who inherit an X chromosome from the mother and a Y chromosome from the father, can inherit the disease only from the mother.
While the patterns of inheritance are well established for many genetic diseases, new mutations may sometimes occur, affecting a child whose family has no history of the disease. Many autosomal dominant conditions cause such severe handicaps that the affected individuals are unable or unlikely to reproduce; for these conditions, the majority of cases arise from mutations. With recessive and X-linked genetic defects, birth of an affected infant into a family that lacks a history of the condition may or may not indicate that a new mutation has occurred. A recessive gene would not be apparent unless someone who carried it married another carrier. X-linked genes might not appear for several generations in small families or those in which most of the children happened to be girls.
Some genetic conditions vary in their impact depending on environmental factors. For example, anencephaly—the absence of a brain—and the related spinal-cord defect, spina bifida, appear to be the result of a combination of genetic and environmental factors. The incidence of these disorders has been found to vary by geographical area, a hint that further research will provide evidence that environmental factors are involved. One important finding is that if a woman takes dietary supplements of folic acid before conception and during early pregnancy, her infant’s risk of these devastating conditions is substantially reduced.
Genetic makeup also influences people’s susceptibility to most of the common diseases of adulthood; most of these diseases involve complex interactions between genes and the environment. Genes for cholesterol and other blood lipids affect an individual’s risk of cardiovascular disease. High blood pressure has a genetic component. A variety of genes affect people’s risk for various forms of cancer, including breast cancer and colorectal cancer. Susceptibility to diabetes is strongly influenced by genes. Knowing individuals’ family health history can help determine whether they need more intensive screening for these diseases.
Mental disorders including schizophrenia, manic depression, and Alzheimer’s disease are also believed to be affected by genetics, although the evidence is fragmentary. While it is well known that people with high cholesterol can lower their risk of heart disease or diabetes by exercising, eating a healthier diet and, if necessary, taking appropriate medications, current knowledge offers little guidance about how to counteract a family history of Alzheimer’s disease or other mental disorders. One can only hope that, with advances in biomedical research, prevention will someday be possible.
Genetic and Newborn Screening Programs
Short of performing surgery on the genetic material, the public health mandate of preventing death and disability from many genetic diseases can be fulfilled only by predicting and preventing the birth of affected children. The process involves various methods of prenatal diagnosis and, when an affected fetus is identified, termination of the pregnancy. One of the most common genetic abnormalities, Down syndrome, is caused by an extra copy of chromosome 21. Affected individuals have a distinctive appearance and are likely to have heart defects and mild to moderate mental retardation. The risk of bearing an infant with the syndrome is well known to increase with the mother’s age and, in the past, women age 35 and older were advised to undergo prenatal testing by amniocentesis, using a needle to sample fetal cells from the uterus. With the option of abortion available, this practice reduced the number of Down syndrome births by about 25 percent.1 However, even though younger women have a lower risk, the number of infants born to them is much higher overall, and they bear most of the affected infants. The American College of Obstetricians and Gynecologists now recommends that all pregnant women be screened.6 In the United States, about 90 percent of women who are found to be carrying an infant with Down syndrome choose to have an abortion.7
There is a more significant role for public health in the prevention of disorders that are caused by recessive genes. When the gene is known, members of populations that have a high incidence of a disease, such as Jews of Eastern European descent, can be screened for carrier status, allowing young people to make informed decisions about marriage and child bearing. In the 1970s, after the gene for Tay-Sachs disease was identified, a major voluntary program offered screening to Jewish people. The response was enthusiastic because the horror of the disease was well known: Apparently healthy infants begin to deteriorate soon after birth, developing paralysis, dementia, and blindness, and die by age 3 or 4. Couples who are both Tay-Sachs carriers can choose to undergo prenatal testing by amniocentesis, allowing for termination of an affected pregnancy.8
However, religious Jews are opposed to abortion. An alternative approach is offered by an organization called Dor Yeshorim, established in the 1980s by a rabbi who had lost four children to Tay-Sachs. The organization offers Jewish high school students in the United States, Israel, and other countries blood tests to determine if they are carriers. To maintain anonymity, and to avoid the stigma of being labeled a carrier, each student is given an identification number and a telephone number that couples can call to learn whether they are genetically “compatible.” In ultra-orthodox communities that practice arranged marriage, a confidential registry was established that allows matchmakers to avoid arranging marriages between carriers of Tay-Sachs and several other debilitating or lethal genetic diseases.9 As a result of the availability of screening, the incidence of Tay-Sachs has been reduced by more than 90 percent in the United States and Canada.8
Another public health approach to preventing the death and disability caused by genetic diseases is provided by newborn screening for metabolic disorders that can be treated if diagnosed soon after birth. An estimated 5000 of the 4.1 million infants born in the United States each year have a potentially severe or lethal condition for which screening and treatment could prevent many or all of the complications.10 The first such condition to be recognized was phenylketonuria (PKU), which was identified as the cause of mental retardation in a significant number of institutionalized adults. Biomedical scientists found that the problem was a genetic inability to metabolize the amino acid phenylalanine, which therefore accumulates in the blood with toxic effects on the brain. They recognized that if affected infants could be identified early they could be put on a special diet low in phenylalanine, and the damage would be prevented.
Dr. Robert Guthrie, a pediatrician from Buffalo, New York, who is considered the “father of newborn screening,” developed a simple, inexpensive test that could diagnose PKU from a drop of a baby’s blood placed on a piece of filter paper. Routine newborn screening for PKU began in the 1960s and is now mandated in all states and most developed countries. Before each baby is discharged from the hospital, the blood sample is obtained by a prick of the baby’s heel. Filter paper specimens bearing the dried blood spots are sent to state public health laboratories for testing.11
A number of other inborn metabolic errors can be identified from testing the same dried drop of blood, and tests for these conditions are mandated by various states depending on the characteristics of their populations. In addition to PKU, all states screen for congenital hypothyroidism, a deficiency of thyroid hormone leading to mental retardation and dwarfism that can be easily treated with regular doses of the hormone. All states now screen for sickle-cell disease, prevalent in African American populations, a program that raised ethical issues when first implemented, as discussed below. The newborn blood samples are used in some states to identify infants who may have been exposed to the human immunodeficiency virus (HIV) prenatally.
Laboratory tests used for newborn screening have become increasingly sophisticated. A method called tandem mass spectrometry searches for more than 20 metabolic disorders in one process, using the dried blood-spot specimen.12 However, the technical ability to detect these disorders has confronted states with dilemmas of how extensively to implement screening for them. Resources are needed to follow up on an abnormal test result, including further testing to confirm the presence of a disease and counseling of parents and pediatricians about a condition that may be extremely rare. There are concerns about who is responsible for treating a disease that has been identified through screening. For example, the special diet required for infants with PKU may be considered a food rather than a drug and thus not be covered by a family’s health insurance. For some conditions, no treatment exists. States differ not only on which conditions they screen for, but also on whether parental consent is required before screening, whether a fee is charged, and the extent of services provided for follow-up.13
The information gained from a genetic test or the screening of a newborn is not always so unambiguous as a fatal diagnosis of Tay-Sachs disease or a clear need for a special diet, as in PKU. With many conditions, uncertainties in the test results as well as in the prognosis complicate decision making. For example, cystic fibrosis (CF), which causes abnormal secretions of the lungs, pancreas, and sweat glands, is the second most common potentially lethal genetic diseases in the United States.14 About 1 in 25 Caucasian Americans, the group at highest risk, carries the recessive gene, which has been identified. The screening test, which measures an enzyme in the blood, yields many false positives. Scientists learned that the accuracy of the diagnosis could be improved by following up the enzyme test with a test on the DNA. As scientists studied the gene, however, they found hundreds of different mutations that could cause CF, and there seemed to be little correlation between the mutation and the symptoms. While many patients with CF die young of breathing problems associated with thick mucus in the lungs, some individuals identified by genetic tests have much milder symptoms. Although there were questions about whether to include CF in newborn screening programs, a major clinical trial found that early identification of affected infants helped to prevent some of the nutritional deficits and deterioration of lung function suffered by children who were identified only when they developed symptoms at an older age.14 All states now screen for CF.15
The identification of the CF gene allows prospective parents to be tested for carrier status, as in Tay-Sachs disease. However, in the case of CF, test results are not as clear. Each of the many possible mutations must be tested for individually, and it is not feasible for laboratories to test for all of them. Currently, the accepted approach for white Americans is to test for the 23 most common mutations. Most carrier couples can be identified this way, but there is still a small risk that couples with a normal test result could bear a child with CF. The frequencies of mutations are lower in other ethnic groups, but identification of carriers is less reliable.16 Scientists are learning more about the relationship between certain mutations and different symptoms, although there is significant variability among affected individuals in the severity of symptoms.
In addition to the conditions that can be identified using the blood spot, the Centers for Disease Control and Prevention (CDC) recommends screening for hearing loss using computerized equipment now available in many hospitals. Profound and permanent congenital hearing loss is estimated to occur in approximately one in 1000 births. About half of these cases are thought to be due to genetic mutations, and about half are due to environmental factors, including prenatal drug exposures and infections such as rubella.17
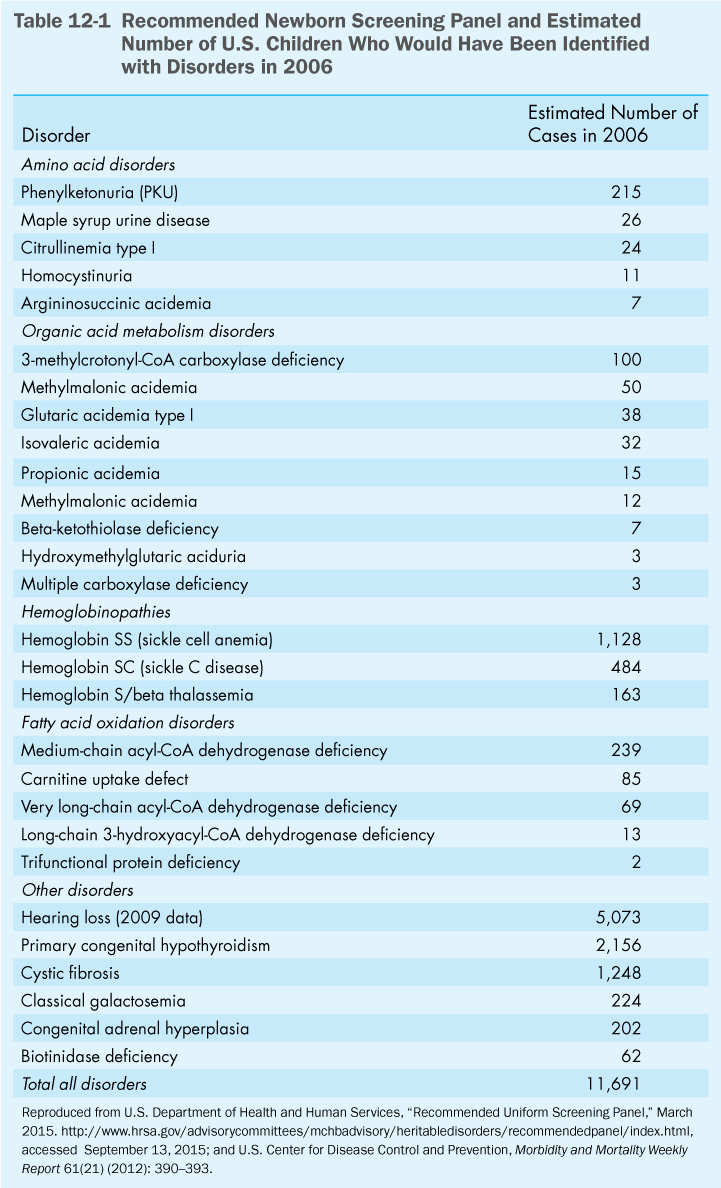
Because of the variation from state to state in the number of disorders included in newborn screening programs, a federal advisory committee in 2006 recommended a panel of 29 disorders that all states should include in their newborn screening programs.15 As of 2009, all the states had implemented the full screening panel.18 An additional three conditions have been added since then: severe combined immunodeficiency in 2009, critical congenital heart disease in 2010, and Pompe disease in 2013.19 A list of the conditions for which the CDC recommends screening is shown in Table 12-1.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


