Drugs are used in combination to produce the appropriate balance of sedation, analgesia and muscle relaxation while minimising unwanted effects; at particular doses and concentrations, each contributes minor or major effects to achieve this balance. Excessive or inadequate doses of any one agent could disturb the balance.
General anaesthesia for surgical procedures involves several steps, although not all are essential for successful anaesthesia:
Premedication is given to adults to reduce anxiety and produce amnesia, usually with a benzodiazepine such as diazepam (Ch. 20). In addition, an antiemetic such as metoclopramide (Ch. 32) may be used.
Anaesthesia was originally induced and maintained solely by inhalation of a volatile agent, when several stages of general anaesthesia are observed during induction in adults (Table 17.2). The stage of excitation with struggling can be overcome by using a bolus of intravenous anaesthetic for rapid induction, followed by an inhalational anaesthetic for maintenance. For short surgical procedures in adults, both induction and maintenance can be achieved with an intravenous anaesthetic alone (total intravenous anaesthesia). In children, excitation is less of a problem, and anaesthesia is often both induced and maintained with an inhalational anaesthetic agent. Full general anaesthesia produces depression of spontaneous respiration and blood pressure, requiring artificial ventilation and perhaps circulatory support. Some short procedures do not need full general anaesthesia, and can be carried out under sedation by an anaesthetic with preserved respiratory and cardiovascular function. The adequacy of general anaesthesia is assessed by monitoring the heart rate, blood pressure and other physiological functions. For example, it can be inferred that the level of anaesthesia is inadequate and that pain is being experienced if the heart rate rises, or the person develops perspiration, tears, return of muscle tone, movement or change in pupil size.
Table 17.2
| Stage | Description | Effects produced |
| I | Analgesia | Analgesia without amnesia or loss of touch sensation; consciousness retained |
| II | Excitation | Excitation and delirium with struggling; respiration rapid and irregular; frequent eye movements with increased pupil diameter; amnesia |
| III | Surgical anaesthesia | Loss of consciousness; subdivided into four levels or planes of increasing depth Plane I: decrease in eye movements and some pupillary constriction Plane II: loss of corneal reflex Planes III and IV: increasing loss of pharyngeal reflex, and progressive decrease in thoracic breathing and general muscle tone |
| IV | Medullary depression | Loss of spontaneous respiration and progressive depression of cardiovascular reflexes, no eye movements; requires respiratory and circulatory support |
For abdominal and thoracic surgery, and for long operations, full skeletal muscle paralysis is produced by giving neuromuscular blocking drugs (Ch. 27), in which case endotracheal intubation and mechanical ventilation are essential. Analgesia can be provided by an intravenous opioid for systemic analgesia, or by a local anaesthetic (Ch. 18) to provide regional analgesia, such as into the epidural space (epidural analgesia) or around peripheral nerves.
At the end of an operation, resumption of consciousness (reversal of anaesthesia) occurs when intravenous anaesthetics are redistributed or metabolised, or when inhalational anaesthetics are redistributed or exhaled. Residual neuromuscular blockade by competitive blocking agents may need reversal with an anticholinesterase such as neostigmine (Ch. 27). Attentiveness, and therefore the ability to drive safely, may be impaired for up to 24 h after general anaesthesia.
Mechanisms of action of general anaesthetics
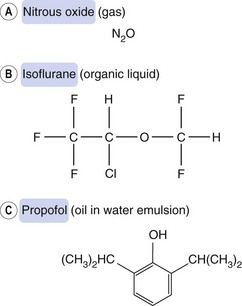
General anaesthesia can be produced by compounds of widely differing chemical structure: simple gases such as nitrous oxide, volatile liquids such as isoflurane and non-volatile solids such as propofol (Fig. 17.1). They act at several sites in the brain, but particularly the brainstem arousal centres, frontal cortex and thalamus to produce unconsciousness, and the spinal cord, pons and medulla to produce muscle relaxation.
General anaesthetics act at cell membranes, and the relationship between lipid solubility and potency led to the Meyer–Overton hypothesis that their incorporation into lipids altered the properties and function of neuronal cell membranes. However, this does not account for many of the properties of general anaesthetics, including the differing anaesthetic potencies of the stereoisomers of some anaesthetic agents which suggests stereospecific interaction with target receptors. The general relationship between lipid solubility and anaesthetic potency is probably more important for determining the pharmacokinetic properties of the drug than for explaining its mode of action.
Although it is not known precisely how general anaesthetics work, there is increasing evidence that implicates actions at ligand-gated ion channels (Table 17.3). Individual intravenous or inhalational anaesthetic agents have diverse abilities to inhibit or enhance the functions of a number of ion channels, thus explaining the differences in their capacities to produce unconsciousness, amnesia, analgesia and muscle relaxation. This may be achieved by direct interaction with the ion channel or by modulation of the receptors that control these channels. In particular, their actions are to inhibit the functions of excitatory receptors (such as those for acetylcholine [nicotinic] and for glutamate (N-methyl-D-aspartate [NMDA] receptors) and to enhance the functions of inhibitory receptors (such as those for γ-aminobutyric acid [GABAA] and possibly glycine), or to activate K+ channels that are widely expressed in inhibitory GABA interneurons.
Table 17.3
Possible sites of action of inhalation and intravenous general anaestheticsa
| Drug group | Properties of group | Receptor and channel targets |
| Etodimate, propofol, thiopental | Potent amnesics Potent sedatives Weak muscle relaxants | Enhance activity at GABAA receptors |
| Nitrous oxide, ketamine | Potent analgesics Weak sedatives Weak muscle relaxants | Inhibit glutamate NMDA receptors Inhibit ACh nicotinic receptors Open two-pore K+ channels |
| Sevoflurane, isoflurane, desflurane | Potent amnesics Potent sedatives Potent muscle relaxants | Enhance activity at GABAA receptors Enhance activity at glycine receptors Inhibit glutamate NMDA receptors Inhibit ACh nicotinic receptors Open two-pore K+ channels |
ACh, acetylcholine; GABA, γ-aminobutyric acid; NMDA, N-methyl-D-aspartate.
aInformation for this table is derived mainly from Solt and Forman (2007) and is based on data from in vitro studies and in vivo studies in transgenic animals.
Receptor binding sites for general anaesthetics have not been fully characterised, but are probably on proteins associated with the receptors and ion channels. General anaesthetics may compete with endogenous ligands or modulate the effect of these ligands at the receptor. As a result, they inhibit both local and long-range (such as thalamocortical) neural circuits.
The various stages of anaesthesia (Table 17.2) probably arise as a result of the different sizes of neurons affected by anaesthetics and their accessibility to the anaesthetic agent. A rapid action on small neurons in the dorsal horn of the spinal cord (nociceptive impulses; Ch. 19) and inhibitory cells in the brain (see effects of alcohol; Ch. 54) explain the early analgesic and excitation phases. By contrast, neurons of the medullary centres are less sensitive.
Drugs used in anaesthesia
General anaesthetics can be grouped according to their route of administration, which is either intravenous or inhalational.
Intravenous anaesthetics
Intravenous anaesthetics can be given by slow intravenous injection for rapid induction of anaesthesia and then replaced by inhalational anaesthetics for longer-term maintenance of anaesthesia. Both propofol and ketamine (but not etomidate or thiopental) can also be given by continuous infusion without inhalational anaesthesia for short operations (total intravenous anaesthesia) or for prolonged sedation. Ketamine is analgesic, unlike all other available intravenous anaesthetics, but it does not reliably suppress laryngeal reflexes, which can make endotracheal intubation more difficult. It is now rarely used, except for paediatric anaesthesia. Some properties of commonly used intravenous anaesthetics are shown in Table 17.4.
Pharmacokinetics
Thiopental is a thiobarbiturate that has a very rapid onset of action (within 30 s) owing to its high lipid solubility and ease of passage across the blood–brain barrier. The duration of action after a bolus dose is very short (about 2–5 min). Blood concentrations fall rapidly, initially because of distribution into tissues with greatest blood flow; distribution then occurs more slowly into the major muscle groups and into adipose tissue, which is lipid-rich but has poor blood flow (Fig. 17.2). With thiopental, total intravenous anaesthesia is not practicable, as during a lengthy procedure the brain and blood and slowly equilibrating tissues would reach equilibrium. Recovery from anaesthesia on cessation of anaesthetic administration would then depend on the elimination half-life (3–8 h for thiopental, related to hepatic metabolism) not the distribution half-life (about 3 min). Therefore, following induction of anaesthesia with thiopental, an inhalational agent is used for maintenance of anaesthesia.
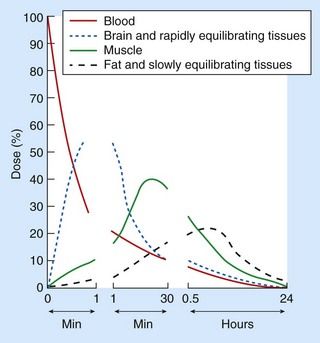
Fig. 17.2 The amounts of thiopental in blood, brain (and other rapidly equilibrating tissues), muscle, adipose tissue and other slowly equilibrating tissues after an intravenous infusion over 10 s.
Note: the time axis is not linear: the continued uptake into muscle between 1 and 30 min lowers the concentration in the blood and in all rapidly equilibrating tissues (including the brain); the terminal elimination slopes are parallel for all tissues; metabolism removes about 15% of the body load per hour.
Propofol has a slightly slower onset of action (about 30 s) compared with thiopental, but its duration of action is also limited by redistribution after a bolus dose. It can be given as an infusion for total intravenous anaesthesia (and for sedation in intensive care), but under these circumstances its duration of action is determined by a slower tissue distribution phase (half-life 0.5–1 h), whereas after prolonged use its duration of action is determined by hepatic clearance (half-life about 6 h). Propofol is particularly useful for day surgery, because of its rapid distribution and absence of hangover effects. It can also be used by intravenous infusion for up to 3 days for sedation in conscious adults requiring controlled ventilation in an intensive care unit.
Ketamine can be given by intramuscular injection or intravenously by bolus injection or infusion. When used for induction or for total intravenous anaesthesia the anaesthetic action is terminated largely by distribution (half-life about 15 min). With prolonged infusion it becomes dependent on hepatic metabolism (half-life 2–4 h).
Etomidate has a rapid onset of action after intravenous injection, and its action is terminated by rapid metabolism in plasma and the liver, so that the duration of action is about 6–10 min with minimal hangover. It is not used to maintain anaesthesia because prolonged infusion can suppress adrenocortical function.
Unwanted effects
 On the central nervous system (CNS): general depression of the CNS can produce respiratory and cardiovascular depression. Slow release of thiopental distributed into tissues may result in some sedation for up to 24 h after use. Hallucinations and vivid dreams are common during recovery from ketamine (emergence reactions), but are less frequent in children. They can be reduced by giving a benzodiazepine (Ch. 20).
On the central nervous system (CNS): general depression of the CNS can produce respiratory and cardiovascular depression. Slow release of thiopental distributed into tissues may result in some sedation for up to 24 h after use. Hallucinations and vivid dreams are common during recovery from ketamine (emergence reactions), but are less frequent in children. They can be reduced by giving a benzodiazepine (Ch. 20). On muscles: extraneous muscle movement is common with etomidate, and to a lesser degree with propofol. They can be reduced by a benzodiazepine or opioid analgesic given before induction. Ketamine increases muscle tone and can cause laryngospasm.
On muscles: extraneous muscle movement is common with etomidate, and to a lesser degree with propofol. They can be reduced by a benzodiazepine or opioid analgesic given before induction. Ketamine increases muscle tone and can cause laryngospasm. On the heart: thiopental, propofol and to a lesser extent etomidate depress the heart, producing bradycardia and reducing blood pressure. By contrast, ketamine more often produces tachycardia and an increase in blood pressure.
On the heart: thiopental, propofol and to a lesser extent etomidate depress the heart, producing bradycardia and reducing blood pressure. By contrast, ketamine more often produces tachycardia and an increase in blood pressure. Nausea and vomiting during recovery are experienced by up to 40% of people but rarely persist for more than 24 h. Propofol has an anti-emetic action.
Nausea and vomiting during recovery are experienced by up to 40% of people but rarely persist for more than 24 h. Propofol has an anti-emetic action. Convulsions have been reported after propofol. These can be delayed, indicating the need for special caution after day surgery.
Convulsions have been reported after propofol. These can be delayed, indicating the need for special caution after day surgery. Pain on injection with etomidate and propofol: this can be reduced by injecting into a large vein or by giving an opioid analgesic just before induction with etomidate, or giving intravenous lignocaine with propofol. Thiopental is an alkaline solution that is irritant if it extravasates outside the vein, causing tissue necrosis.
Pain on injection with etomidate and propofol: this can be reduced by injecting into a large vein or by giving an opioid analgesic just before induction with etomidate, or giving intravenous lignocaine with propofol. Thiopental is an alkaline solution that is irritant if it extravasates outside the vein, causing tissue necrosis.Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree