Chapter 9 Gastrointestinal Tract
The Mouth
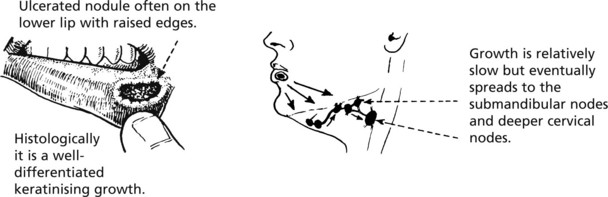
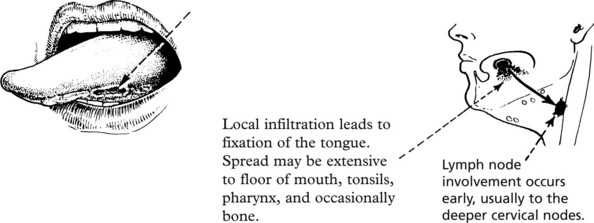
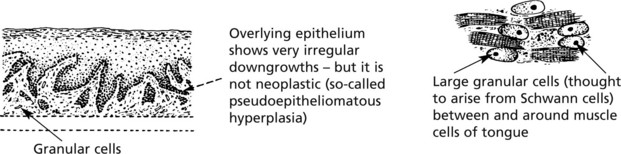
Oral Cancer
Oral cancer accounts for 2% of cancers in the United Kingdom. There is wide geographical variation – commoner in S. East Asia. Males are at least twice as commonly affected as women – it is a disease of the elderly.
Mouth
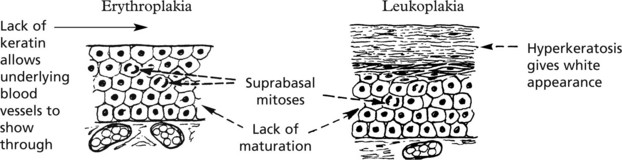
Erythroplakia and Leukoplakia
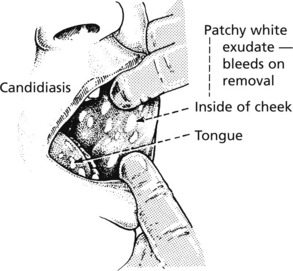
These terms describe velvety red patches and white patches in the oral mucosa. These are important because they may represent dysplasia of the squamous epithelium and may lead to squamous cancer.
Not all examples of leukoplakia are premalignant and may also be due to:
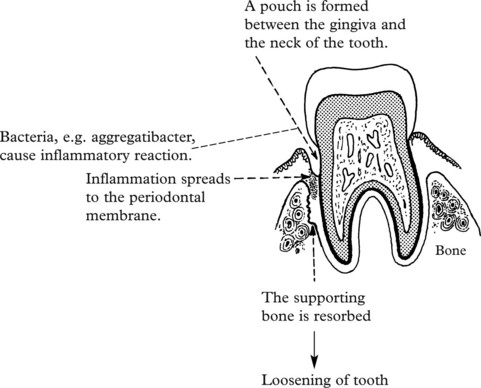
Dental Caries and Periodontal Disease
These two very common processes are primarily of importance to dentists but an understanding is also valuable for doctors.
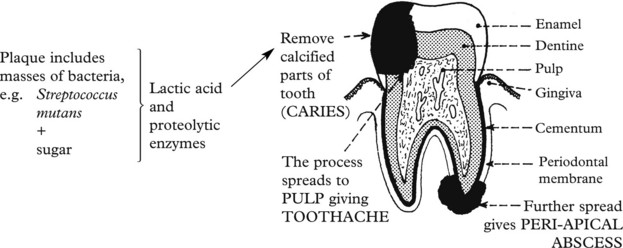
Dental Caries
This is the commonest disease of teeth.
Poor oral hygiene + high sugar intake lead to formation of plaque.
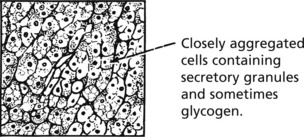
Diseases of the Salivary Glands
Inflammation
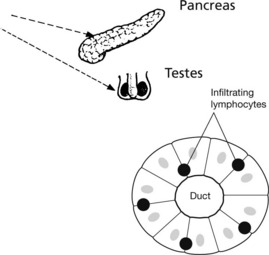
The commonest acute inflammation is due to the mumps virus, which produces acute swelling, particularly of the parotid glands, with oedema and mononuclear infiltration of the interstitial tissue.
The testes and pancreas may also be inflamed and atrophy may follow.
Salivary Glands – Benign Tumours
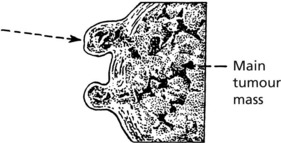
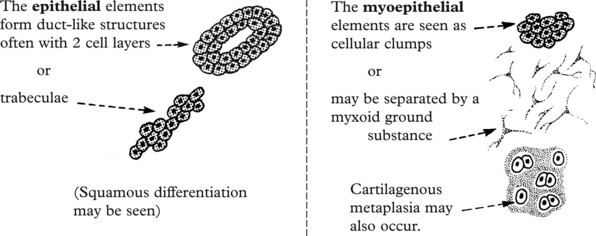
Pleomorphic Adenoma
This is the commonest tumour of the salivary glands and most often occurs in the parotid. The term ‘pleomorphic’ applies not to the nuclei of the cells but to the different types of tissue found. These are derived from the epithelial and myoepithelial cells.
Salivary Glands – Carcinomas
Almost all malignant tumours of the salivary glands are adenocarcinomas. They affect major and minor glands and arise de novo or from pre-existing pleomorphic adenoma. The prognosis is variable.
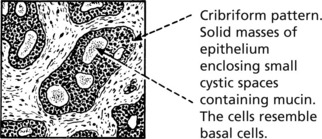
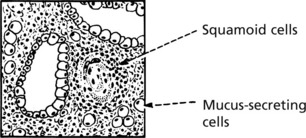
Three unusual subtypes are worth noting.
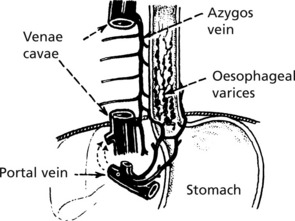
Oesophagus
The oesophagus is a muscular tube 25 cm long lined by stratified squamous epithelium which is resistant to damage by heat, cold and mechanical trauma.
Inflammation
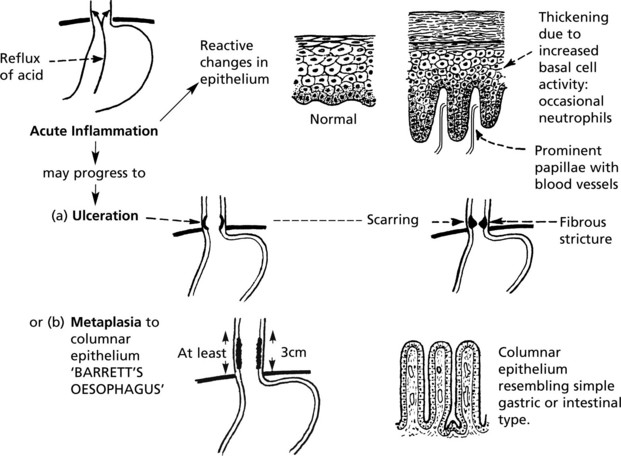
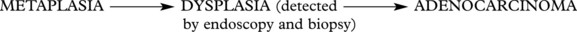
Reflux Oesophagitis
This is an important premalignant lesion with a 30–40 fold increased risk of cancer.
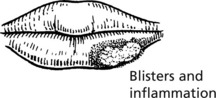
Other Forms of Oesophagitis
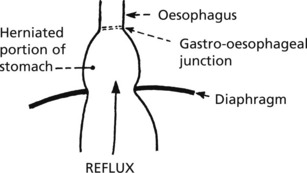
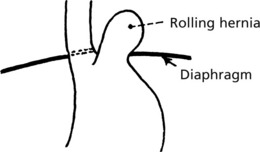
Hiatus Hernia
In hiatus hernia part of the stomach herniates into the thorax. This is common, particularly in the elderly, though often asymptomatic. Two forms are seen:
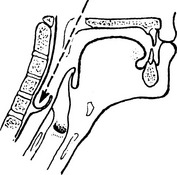
Diverticula
These are relatively rare and are of 2 varieties.
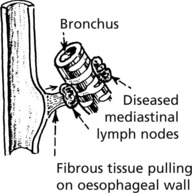
Rarely, there may be a congenital diverticulum at the level of the bifurcation of the trachea.
Obstruction usually leads to dysphagia – difficulty in swallowing. The causes include:
Strictures of the oesophageal wall due to:
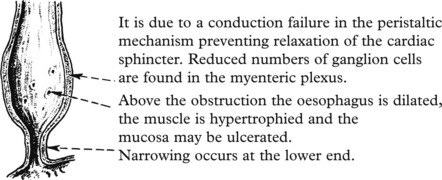
Achalasia of the oesophagus develops in young adults and may cause severe obstruction.
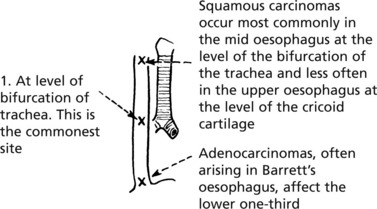
Oesophagus – Tumours
Benign tumours of the oesophagus are rare. They are almost always of connective tissue origin (usually leiomyomas) and form polyps within the lumen, causing obstruction.
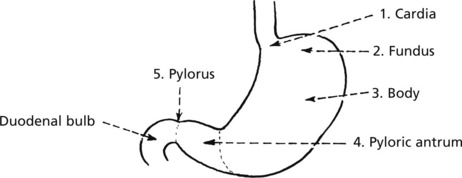
Stomach
The stomach is divided into five anatomical regions:
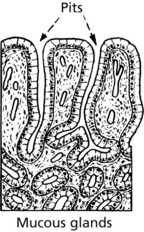
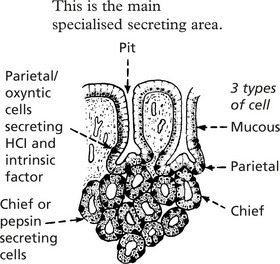
Three forms of mucosa are seen:
Gastritis
Acute Inflammation
Mild acute gastritis is an acute inflammation with neutrophil reaction in the superficial layers of the mucosa. Pain and sickness have a multitude of causes varying from hot fluids, alcohol and aspirin which act as direct irritants, to infections such as childhood fevers, viral infections and bacterial food poisoning.
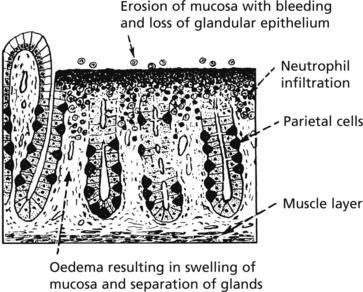
Haemorrhagic Erosions
Note that the changes are superficial so that restoration to normal can occur very quickly occur.
Chronic Gastritis
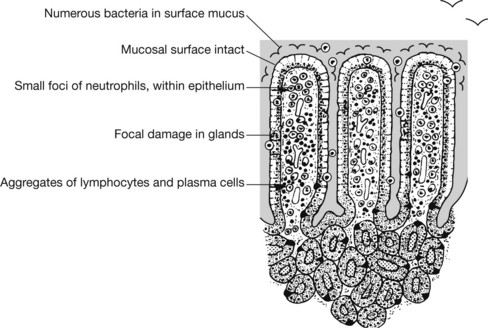
There are 3 main causes of chronic gastritis:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree