Gastrointestinal Physiology
GENERAL FEATURES
In general, the gastrointestinal (GI) tract includes what structures?
The entire gut tube from mouth to the anus, as well as the accessory organs of digestion (liver, gallbladder, and pancreas)
What is the primary function of the GI (alimentary) tract?
Nutrient absorption
Gut motility refers to what?
The movement of food (in various stages of digestion) through the GI tract
What is the innermost surface of the gut tube?
The mucosa (composed of the first four items in the next question)
Please identify the labeled components of cellular anatomy in the following cross-section of the GI tract.
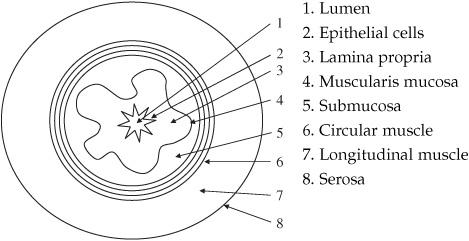
Figure 6.1 Structural features of the GI tract.
What is the main muscle type in the GI canal?
Visceral smooth muscle (VSM)
Where in the GI tract do we have skeletal muscle?
In the oropharynx and esophagus (absent by the distal third of the esophagus) where we have voluntary control over swallowing and chewing, and the external anal sphincter which we gain control of during infancy
What is unique about the muscle in the GI tract?
The smooth muscle cells are interconnected by gap junctions and function together as a single unit, much like cardiac muscle. Thus, an action potential generated in one muscle cell can easily spread to adjacent cells, allowing the cells to peristalse
Describe the roles of the following anatomical regions of the GI tract:
Oropharynx
Chewing breaks food into smaller pieces which provides more surface area for digestion, also houses some glands which begin secreting hydrolyzing enzymes
Esophagus
Propels food from oropharynx to stomach
Stomach
Grinds and mixes food with stomach acids to provide a suitable slurry to enter the small intestine
Small intestine
The workhorse of nutrient absorption; entry into small intestine is coordinated with the secretion of the various exocrine enzymes from the liver and the pancreas (more to come)
Large intestine
Water and electrolyte reabsorption along with storage of fecal waste
How long does transit through the following GI segments take?
Esophagus
Seconds
Stomach
2 to 5 hours, conventionally we talk about the stomach being 50% empty after 3 hours.
Small intestine
Also 2 to 5 hours
Large intestine
Approximately 30 to 50 hours
What is the collective term for the immune defense of the gut?
Gut-associated lymphoid tissues (GALT); this term encompasses a number of different lymphatic tissues throughout the gut tube
List some of the major component lymphatic tissues in the GI tract.
Tonsils, Peyer patches, lymphoid aggregate in the appendix
GASTROINTESTINAL CONTROL—NERVOUS
Name the two main nervous systems of the gut.
- Enteric or intrinsic system
- Autonomic or extrinsic system
What are the components of the extrinsic system? (Not including the control of the oropharynx)
Parasympathetic nervous system (PNS) and sympathetic nervous system (SNS)
Name the main function of the SNS in the GI tract.
Excitation
Which nerves carry PNS fibers and what structures/organs do they innervate?
Vagus: esophagus, stomach, pancreas, small intestine, and first portion of the large intestine
Pelvic splanchnic nerves: second portion of large intestine, rectum, and anus
Name the main function of the SNS with respect to the GI tract.
Inhibitory
Which GI nerves carry SNS fibers?
Spinal nerves
Is the action of SNS exclusively inhibitory?
No
Where are the exceptions?
Lower esophageal sphincter, pyloric, and internal anal sphincter
Why does sympathectomy not affect alimentary motility?
Reuptake of norepinephrine (NE) by sympathetic nerve endings is so rapid that only a great rise in NE concentration during a sympathetic discharge can have a significant effect on normal GI motility
Overexcitation of the extrinsic nervous system can produce what common syndrome?
Irritable bowel syndrome (IBS)
What afferent information is carried by the extrinsic system?
All conscious sensations from the gut: fullness, pain, nausea, etc.
What are the two anatomical components of the intrinsic system?
Myenteric or Auerbach plexus
Submucosal or Meissner plexus
What are the functions of the intrinsic system?
Acts as mediator of information between the extrinsic nervous system and the alimentary tract
Commands most functions of the GI tube especially motility and secretion
Can execute neural function of the gut without extrinsic innervations
Where is the myenteric plexus located?
It lies between the longitudinal and circular muscle layers
What is the main function of the myenteric plexus?
Controls and coordinates motility
Where is the submucosal plexus located?
It lies in the submucosa (hence the name), between the muscularis mucosa and circular muscle layer
What is the main function of the submucosal plexus?
Controls secretion and absorption as well as local blood flow
GASTROINTESTINAL CONTROL—HORMONAL
What is the main stimuli for hormone release?
Food lying adjacent to GI mucosa
What is the main function of GI hormones?
Regulate the digestive process by influencing secretion, motility, and blood flow
What are hormones? (see Chapter 7 for more details)
Chemical signals that fall into many categories, which help relay signals across varying distances
Define neurocrine.
Process in which one nerve fiber releases messenger that acts across a short distance upon a target cell (nerve fiber, muscle cell, or gland cell)
Define paracrine.
Released messenger acts upon adjacent cells
Define endocrine.
Stimulus acting upon a receptor causes the cell to release a messenger into the bloodstream that then acts on a distant target cell
Action potential causes release of messenger that enters the bloodstream and acts upon a distant target cell
Name the main gastric hormones.
Gastrin
Cholecystokinin (CCK)
Secretin
Gastric inhibitory peptide (GIP)
Name the cells that secrete gastrin.
G cells in the antral mucosa of stomach
Of the above types of hormonal systems, which is used by gastrin to exert its effect?
Endocrine (and to a lesser degree neuroendocrine)
What are the three forms of gastrin?
- Big gastrin (34 amino acids)
- Little gastrin (17 amino acids)
- Mini gastrin (14 amino acids)
Which form of gastrin is most abundant and potent?
Little gastrin
Which form has the longest half-life?
Big gastrin (42 minutes)
Which amino acids confer physiological activity?
Last four amino acids at the carboxy terminal (i.e., little gastrin: AA 14 to 17)
What are the major stimuli for gastrin’s secretion?
- Amino acids; notably L-amino acids like phenylalanine, tryptophan, cysteine, tyrosine
- Vagal stimulation
- Stomach distention
What are the functions of gastrin?
- Primary: Increases hydrochloric acid (HCl) secretion (via parietal cells)
- Stimulates growth of gastric mucosa
- Increases gastric motility
- Increases LES contraction (preventing reflux)
- Decreases ileocecal sphincter contraction (dubbed the gastrocolic reflex; this allows defecation)
- Increases pepsinogen secretion
What are some other stimuli for gastrin’s secretion?
Epinephrine
Calcium
Acetylcholine (ACh)
What are the inhibitors of gastrin secretion.
pH < 2 (feedback inhibition) Somatostatin
Secretin
Calcitonin
GIP
Glucagon
Vasoactive inhibitory peptide (VIP)
Which other GI hormone is chemically “related” to gastrin?
CCK, which shares five amino acids on the carboxy terminal, the extra amino acid of CCK offers receptor specificity, but cross activation is possible
While the two enzymes share five amino acids, how do they differ in their shared function?
Potency
What cells secrete CCK?
I cells of the duodenum and jejunum
Which hormonal system is used by CCK to exert its effects?
Endocrine
What are the major stimuli for CCK’s secretion?
Protein and fat digestion products in the small intestine
What product of fat digestion does not stimulate CCK secretion?
Triglycerides
Why don’t triglycerides stimulate the release of CCK?
They cannot cross the intestinal membranes
Which form is most abundant and potent?
CCK 8 (octapeptide)
On which amino acid sequence is the physiological activity located?
On the octapeptide on the carboxy terminal
What are the functions of CCK?
Increase gallbladder and pancreatic contraction
Decrease contraction of the sphincter of Oddi, allowing pancreatic secretion
Slow gastric emptying
Increase pepsinogen secretion
Decrease LES contraction
Stimulate growth of the exocrine pancreas
Work synergistically with secretin to increase bicarbonate secretion in the small intestine
What syndrome occurs when non-β-cell tumors of the pancreas secrete gastrin (e.g., gastrinoma)?
Zollinger-Ellison syndrome
Name the cells that secrete secretin.
S cells of the duodenum
What is the primary stimulus for secretin secretion?
H+ in the duodenum
What is another stimuli for secretin release?
Protein and fat digestion products in the small intestine
What system of cellular communication is used by secretin to exert its actions?
Endocrine and paracrine
What are the functions of secretin?
- Stimulates bicarbonate secretion from pancreatic and biliary duct cells
- Decreases HCl secretion
- Enhances activity of CCK on pancreatic secretion and gallbladder contraction
- Decreases gastric and intestinal motility
- Increases pepsinogen
Which hormones are part of the secretin-glucagon family?
Secretin
Glucagon
Vasoactive intestinal peptide (VIP), sometimes called vasoactive inhibitory peptide
Gastric inhibitory peptide (GIP)
What cells secrete GIP?
K cells of the jejunum and duodenum
What are the major stimuli for GIP’s release?
Products of carbohydrate and fat breakdown in the small intestine
What system is primarily used by GIP to exert its actions?
Endocrine
What are the functions of GIP?
Stimulates insulin release and inhibits H+ secretion
What are the GI paracrine hormones?
Somatostatin, serotonin, and histamine
Name the cells that secrete somatostatin.
Multiple cells in the GI tract
What is the stimulus for somatostatin release?
Presence of H+ in the lumen
What inhibits the secretion of somatostatin?
Vagal stimulation
What is the function of somatostatin?
Think: “stasis”
- Inhibits release of all GI hormones
- Inhibits gastric H+ secretion
- Inhibits gallbladder and pancreatic contraction
Name the cells that secrete histamine.
Enterochromaffin-like (ECL) cells within the gastric mucosa
What is the function of histamine in the GI tract?
Increases gastric H+ secretion (both directly and by potentiation of the effects of gastrin and vagal stimulation)
Why does that relationship make sense? (think about mast cell activation → increased acid secretion)
Histamine functions, in general as an immune cytokine, in the gut it has a similar function- acidification of the gastric lumen makes the environment far more hostile to arriving pathogens
What cells secrete serotonin?
Enterochromaffin (EC) cells in the gut wall
What is their primary stimulus for secretion?
Distension of the gut lumen
What does serotonin do in the gut?
It is primarily excitatory and leads to increased gut motility
What are the GI neurocrine hormones?
VIP
Gastrin-releasing peptide (GRP) (bombesin)
Enkephalins
What other GI hormone is VIP homologous to?
Secretin
Name the cells that normally secrete VIP.
Neuronal cells in the mucosa and smooth muscle of the GI tract
What tumor type can also secrete VIP?
Pancreatic islet cell tumors
What are the functions of VIP?
Relaxes GI smooth muscle (including LES)
Stimulates pancreas to secrete HCO3−
Inhibits gastric H+ secretion
Name the cells that secrete GRP.
Vagal nerves that innervate G cells
What is the function of GRP?
Stimulates gastrin release
What are the types of enkephalins?
Met-enkephalin and Leu-enkephalin
Name the cells that secrete enkephalins.
Neurons in the mucosa and smooth muscle of the GI tract
What are the functions of enkephalins?
- Contract GI smooth muscle (especially lower esophageal, pyloric, and ileocecal sphincters)
- Inhibit secretion of fluid and electrolytes by the intestines
What hormone is secreted into the bloodstream to increase appetite?
Ghrelin
What is ghrelin’s stimulus for secretion?
Hypoglycemia
What cells secrete ghrelin?
X cells in the body of the stomach
GASTROINTESTINAL CONTROL—MOTILITY
Name the types of electrical waves found in the alimentary tract.
Slow waves and spike potentials
What are slow waves?
Fluctuating changes in the resting membrane potential
What are slow waves not?
Action potentials
Where are slow waves generated?
Cells of Cajal (pacemaker of the alimentary tract)
Why are slow waves important?
Determine the rhythmicity of the GI tract’s contractions by controlling the pattern of spike potentials
Where in the tract are the waves the slowest?
Stomach at 3 waves/min
Where in the tract are the waves the fastest?
Duodenum at 12 waves/min
What are spike potentials?
Action potentials of the alimentary tract
How are spike potentials generated?
They occur when the resting gut pacemaker membranes depolarize
Name three factors that cause increased depolarization of gut pacemaker cells.
- Muscle stretch
- ACh
- PNS
Which channels are involved in the generation of the action potential?
Ca2+-Na+ channels, just like anywhere else in the body
How does a spike potential cause contraction?
Like other muscle cells, Ca2+ enters the smooth muscle cell interior
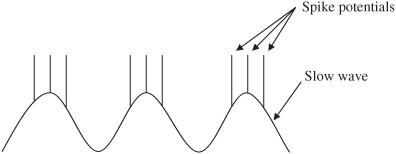
Figure 6.2 Electrical signaling in the GI tract.
Define motility.
Mechanical activity of the GI tract that is divided into mixing (segmentation) and propelling (peristalsis)
Describe segmentation.
Contraction around the bolus sends intestinal contents (chyme) backward and forward. The area then relaxes and the material moves back into the segment, mixing the contents.
Describe peristalsis.
Contraction behind the bolus is coupled with relaxation in front of it, which propels the bolus distally
What factors promote inhibition of peristalsis?
Ileogastric reflex and CCK
Name the functions of small intestinal motility.
Allows for mixing of food bolus with digestive enzymes
Exposes food molecules to absorptive mucosa
Propels nonabsorbed material to the colon
Which aspect of motility is most important in the small intestine?
Segmentation: allows for increased surface area for digestion and absorption of chyme
What is the frequency of slow waves in the following segments of the small intestine?
Duodenum
12 waves/min
Proximal jejunum
12 waves/min
Terminal ileum
8 to 9 waves/min
What other factor is important for segmental contraction?
Excitation by the myenteric plexus
What is the average velocity of peristalsis waves in the small intestine?
0.5 to 2.0 cm/s
What factors stimulate increased peristalsis activity?
Gastroileal reflex (neural regulation)
Gastrin
CCK
Serotonin
Insulin
What factors inhibit peristalsis activity?
Secretin and glucagon
Name the two types of motility found in the colon.
- Haustral segmental movement
- Mass movement
What are haustra?
Invaginations of the circular and longitudinal muscles of the large intestine which provide some compartmentalization
What are mass movements?
Modified peristalsis that is characterized by uniform contraction and movement of colonic contents down the descending colon
How often do mass movements occur per day?
1 to 3 times/day
Name some factors that stimulate mass movement.
Gastrocolic reflex
Duodenocolic reflex
Irritation of the colon
PNS stimulation
Over distention of a colonic segment
Where is the vomiting center located?
Medulla
What stimuli does the vomiting center respond to?
Gag
Gastric distention
Vestibular stimulation
Where are the chemoreceptors that can induce vomiting?
Fourth ventricle
What stimuli do the chemoreceptors respond to?
Emetic substances
Vestibular stimulation
Radiation
What is vomiting?
Reverse peristalsis that propels GI contents in the stomach towards the oropharynx and out through the upper esophageal sphincter
What occurs if the peristalsis is not strong enough to overcome the pressure in the upper esophageal sphincter (UES)?
Retching
Where does the reverse peristalsis begin?
Small intestine
MOUTH AND ESOPHAGUS
Course reduction in food particle size is accomplished by what process?
Mastication
During this process what fluid is introduced to the food bolus?
Saliva
What are the principal glands of salivation?
- Submandibular (70%)
- Parotid (25%)
- Sublingual (5%)
Name the functions of saliva.
Dissolves and alkalinizes ingested food particles
Protects the oral cavity
Moistens the mouth (lubrication)
Begins hydrolysis of complex starches
Name and describe the two types of salivary secretions.
- Serous secretions: contain enzymes for starch digestion
- Mucous secretions: contain mucin for lubrication and protection
What is the enzyme found in salivary secretions responsible for carbohydrate digestion?
Salivary amylase
In what ways does saliva help protect the oropharynx?
- Salivary piece: IgA—binding protein which activates secreted IgA
- Lactoferrin secretion: chelates iron to make it unavailable for bacteria
- Lysozyme: attacks bacterial cell walls
- Acquired pellicle: a thin layer of glycoproteins that adheres to teeth to help protect them
Name the type of secretions for the principal glands:
Parotid
Serous
Submandibular
Serous and mucous
Sublingual
Serous and mucous
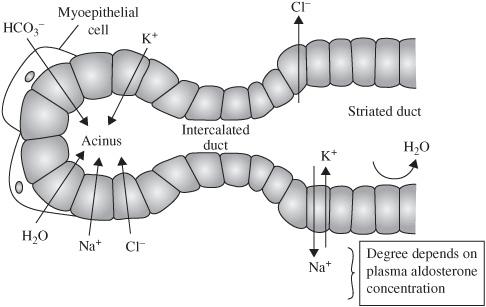
Describe the glandular process of saliva secretion:
Initial saliva from gland (isotonic to plasma)
↓
Ducts secrete K+ and HCO3−
Na+ reabsorption occurs in the salivary ducts in proportion to the time spent there, usually leading to hypotonic saliva
In periods of fasting, when salivary flow is low, how does the composition of saliva change?
The saliva remains in the duct longer and more sodium and chloride are reabsorbed without water, so it becomes hypotonic.
And when salivary flow is rapid?
Quick transit times through the duct leads to secretions that more closely resembles acinar (plasma) composition
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree