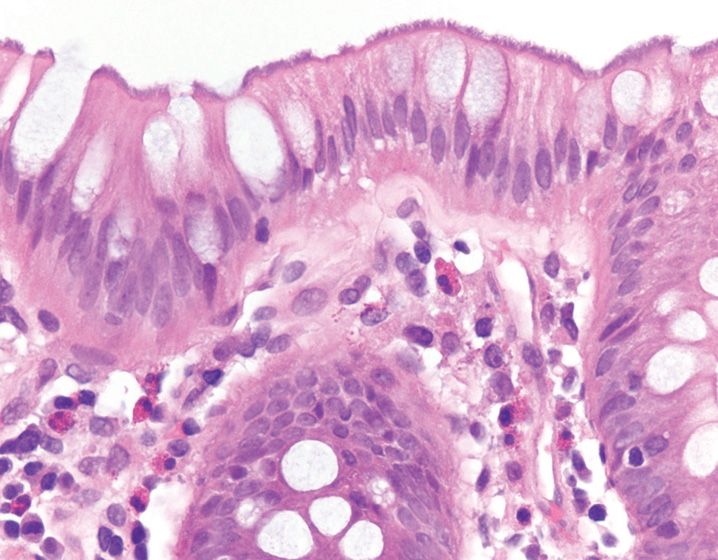
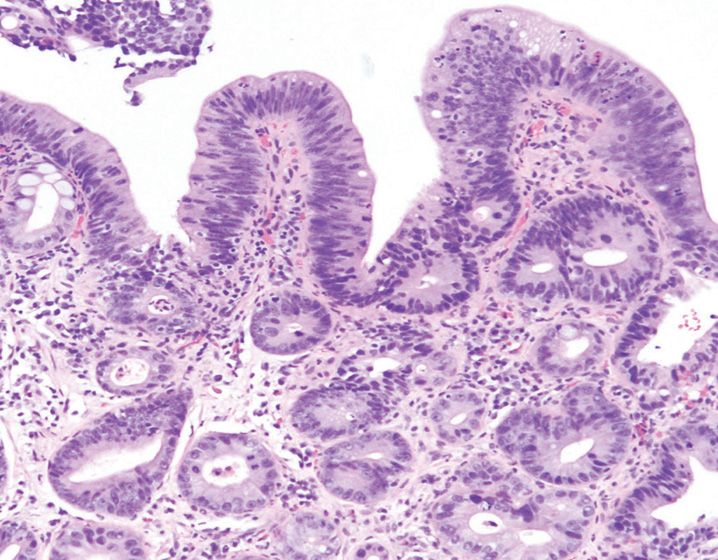
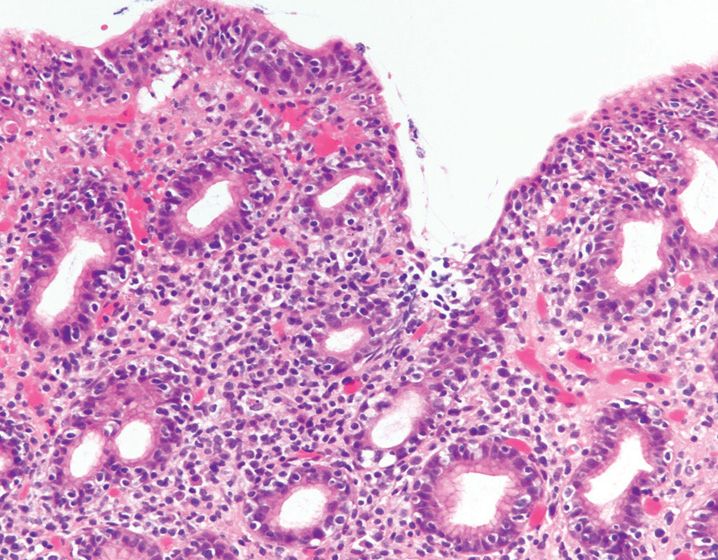
FIGURE 13-1
(A) Adenovirus infection
(B) Cytomegalovirus infection
(C) Herpes simplex infection
(D) Rotavirus infection
(E) Norwalk virus infection
16. Human papilloma virus infection is implicated in the pathogenesis of all of the following entities, except
(A) Anal squamous cell carcinoma
(B) Condyloma
(C) Esophageal squamous cell carcinoma
(D) Kaposi’s sarcoma
(E) Squamous papilloma
17. Which of the following infections is least likely to induce a granulomatous pattern of injury?
(A) Actinomyces israelii
(B) Clostridium difficile
(C) Mycobacterium tuberculosis
(D) Mycobacterium avium–intracellulare
(E) Yersinia pseudotuberculosis
18. All the following conditions are associated with pseudomembrane formation, except
(A) Campylobacter jejuni colitis
(B) Clostridium difficile colitis
(C) Collagenous colitis
(D) Enterohemorrhagic E. coli
(E) Ischemia
19. Which of the following infections is not associated with acute self-limited pattern of colitis?
(A) Aeromonas
(B) Campylobacter jejuni
(C) Enterohemorrhagic E. coli
(D) Salmonella
(E) Shigella
20. A colonic biopsy from a 70-year-old woman with history of cardiovascular disease shows a pseudo-membranous pattern of mucosal injury. Which of the following histologic features is considered to be specific for ischemic colitis?
(A) Ballooned crypts
(B) Cryptitis and crypt abscesses
(C) Degenerating goblet cells “pseudo signet-ring cells”
(D) Hyalinized lamina propria
(E) Mucosal necrosis
21. Which region of the gastrointestinal tract is most commonly affected by tuberculosis?
(A) Anal canal
(B) Colon
(C) Esophagus
(D) Ileocecal valve
(E) Stomach
22. All the following pathologic features favor a diagnosis of Crohn’s disease over intestinal tuberculosis, except
(A) Chronic mucosal injury in adjacent mucosa
(B) Circumferential ulcers
(C) Deep fistulas
(D) Mucosal cobblestoning
(E) Transmural lymphoid aggregates
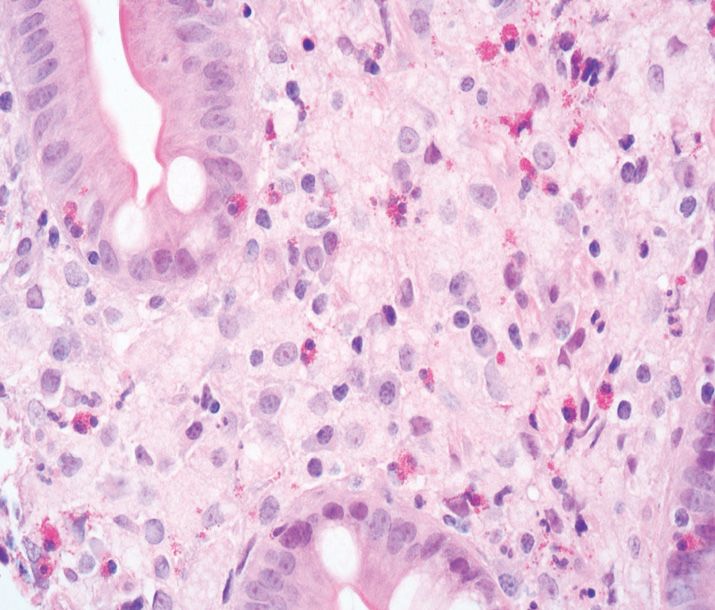
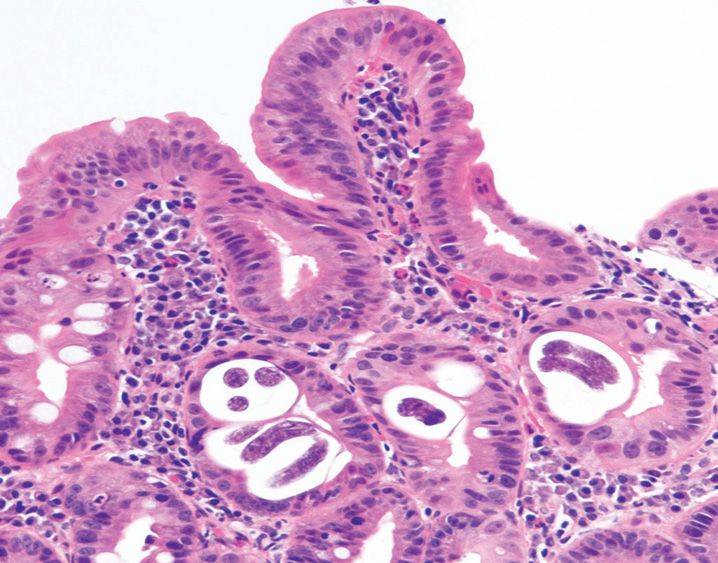
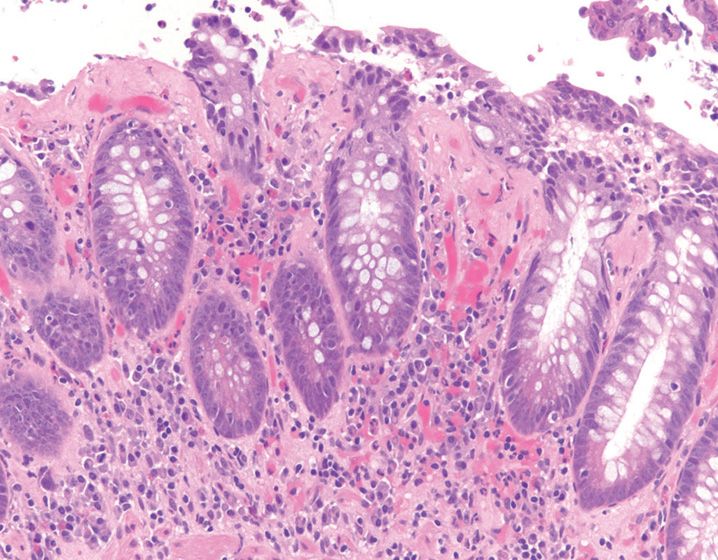
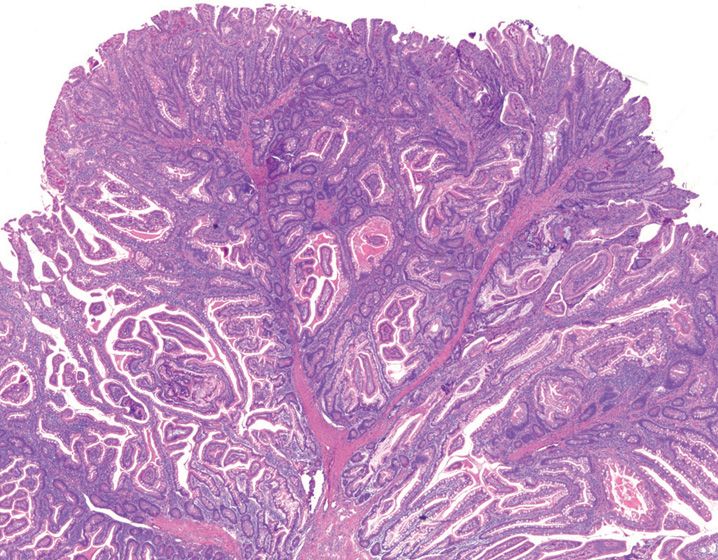
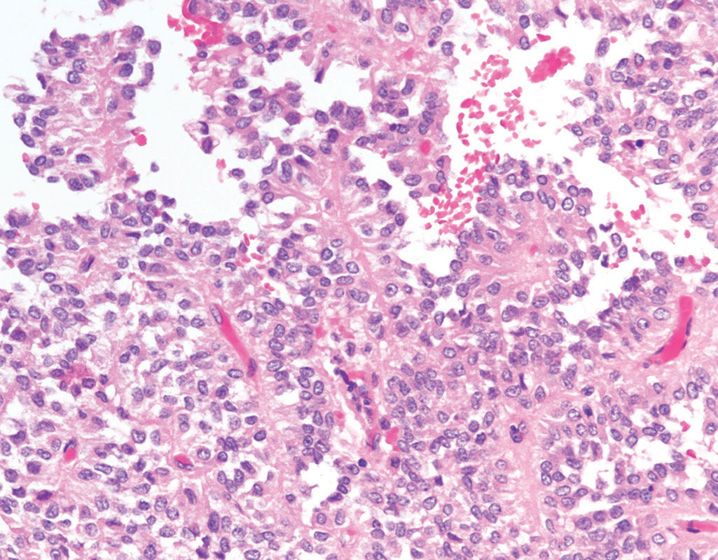
23. The special stain of choice for confirming the pathologic finding shown in this figure is (Figure 13-2)
(A) Brown–Hopps stain
(B) Giemsa stain
(C) Trichrome stain
(D) Von Kossa stain
(E) Warthin-Starry stain
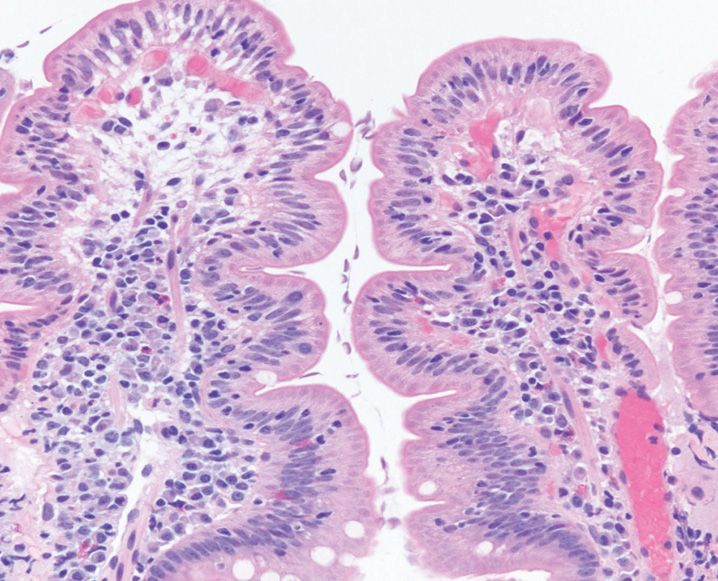
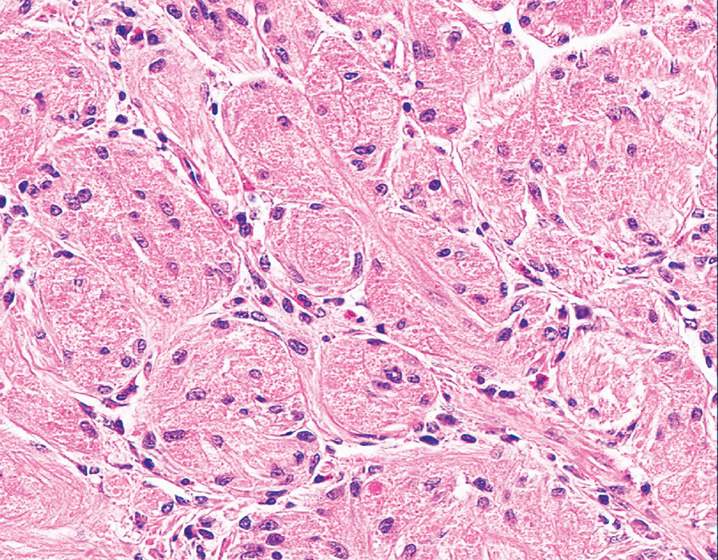
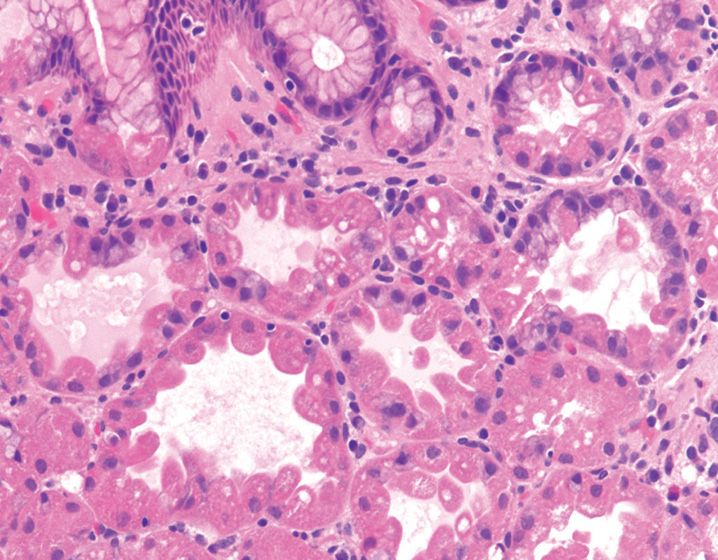
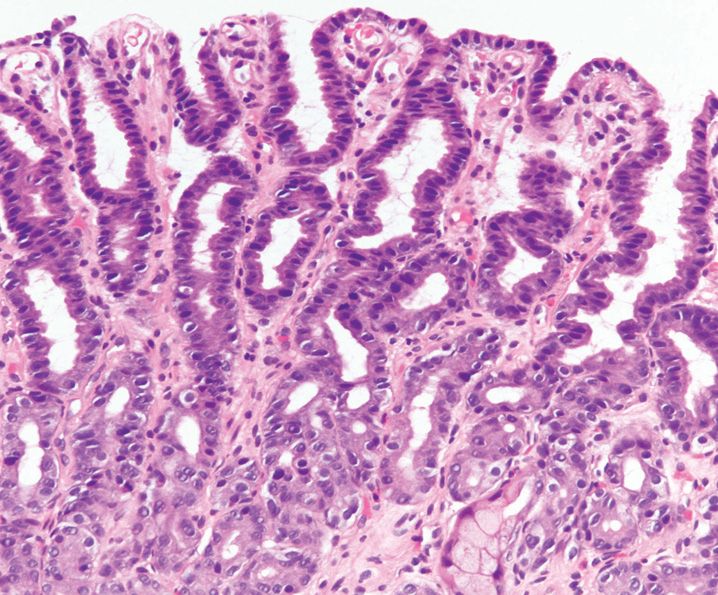
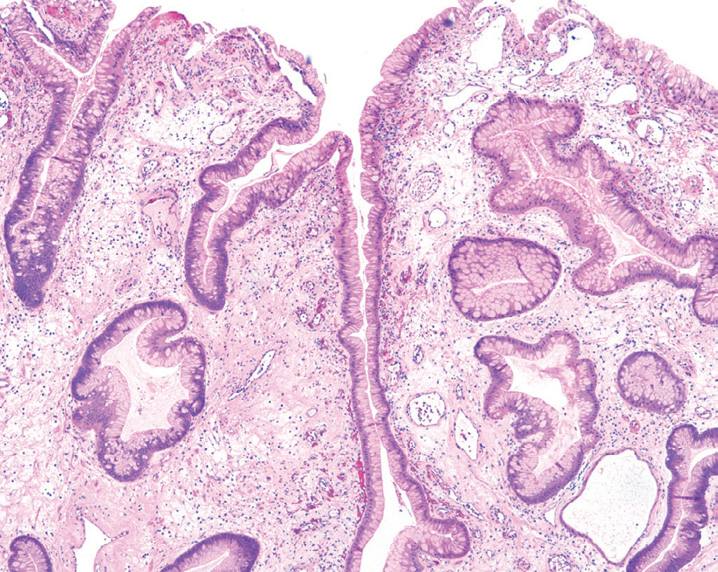
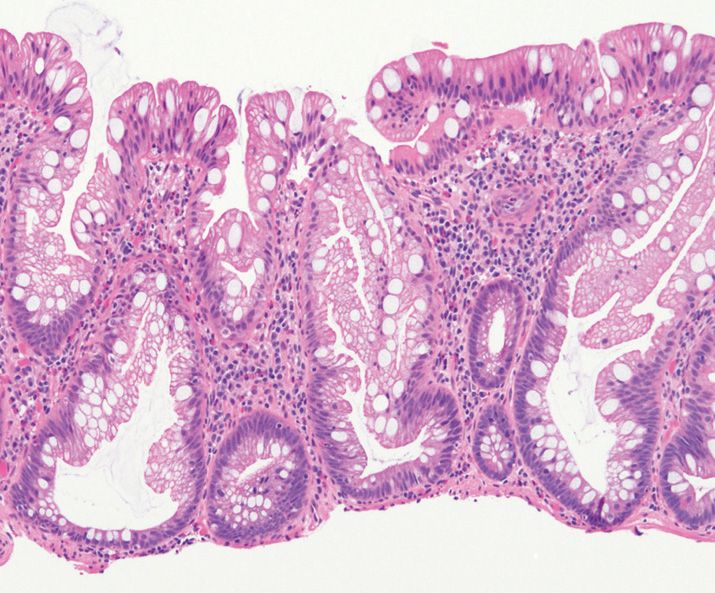
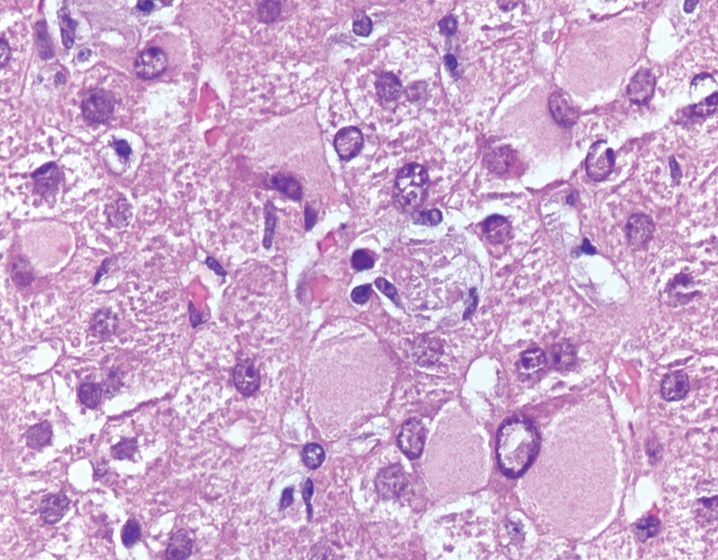
24. A 45-year-old man presents with malabsorption, arthritis, and lymphadenopathy. A duodenal biopsy obtained from this patient is shown in Figure 13-3. He does not have hepatosplenomegaly. A PAS with diastase stain is found to be positive and diagnostic of this condition. The most likely etiology for this patient’s symptoms is
(A) Crushed Brunner’s glands
(B) Gaucher’s disease
(C) Malakoplakia
(D) Mycobacterium avium–intracellulare infection
(E) Whipple’s disease
25. Which protozoal organism causes dysentery, flask-shaped cecal ulcers, and resembles macrophages on histologic examination?
(A) Entamoeba histolytica
(B) Cryptococcus neoformans
(C) Giardia lamblia
(D) Leishmania donovani
(E) Trypanosoma cruzi
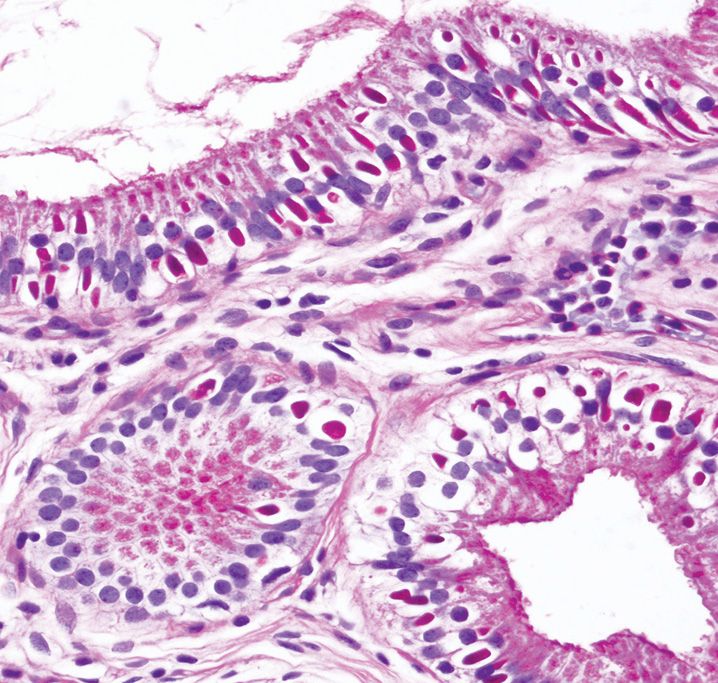
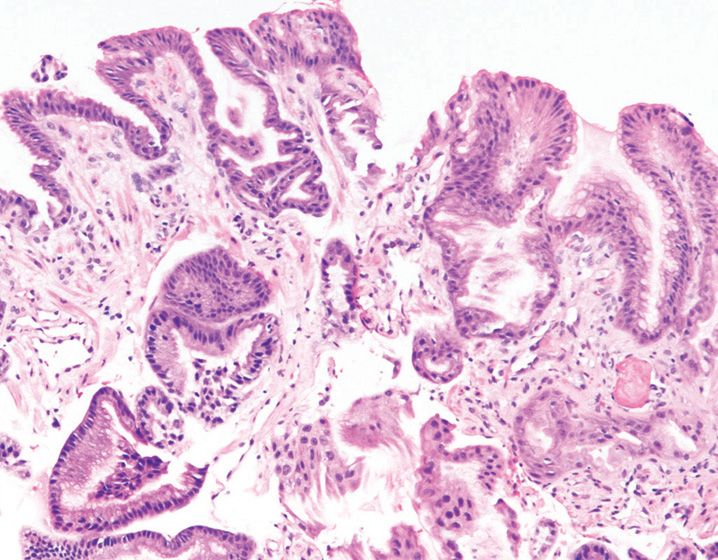
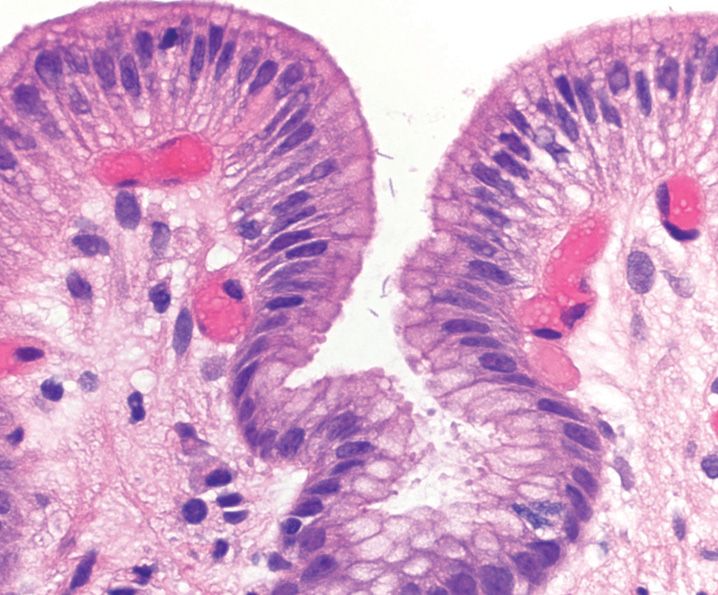
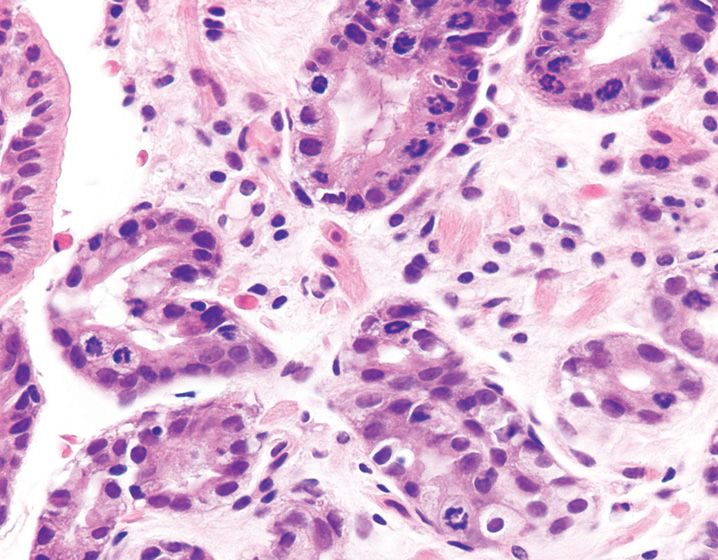
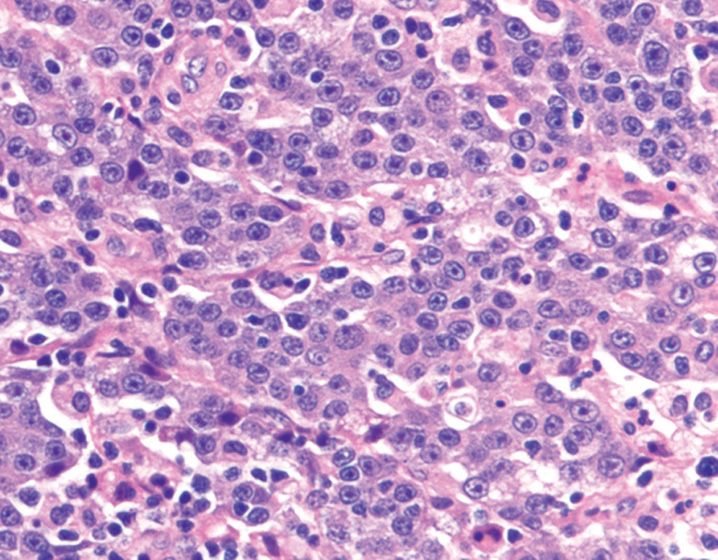
26. Which of the following features is not typically associated with the finding shown in this duodenal biopsy? (Figure 13-4)
(A) Foul-smelling watery diarrhea
(B) Minimal inflammation
(C) Normal endoscopy
(D) Tissue invasion
(E) Underlying immunodeficiency disorder
27. Which of the following flagellate organisms is implicated in the pathogenesis of megaesophagus and megacolon?
(A) Cryptosporidium parvum
(B) Giardia lamblia
(C) Leishmania donovani
(D) Toxoplasma gondii
(E) Trypanosoma cruzi
28. A 20-year-old woman with history of biliary dyskinesia undergoes cholecystectomy (see Figure 13-5). Which of the following infectious organisms is highlighted by the PAS stain?
(A) Cryptosporidium parvum
(B) Cyclospora cayetanensis
(C) Enterocytozoon bieneusi (microsporidia)
(D) Isospora belli
(E) Toxoplasma gondii
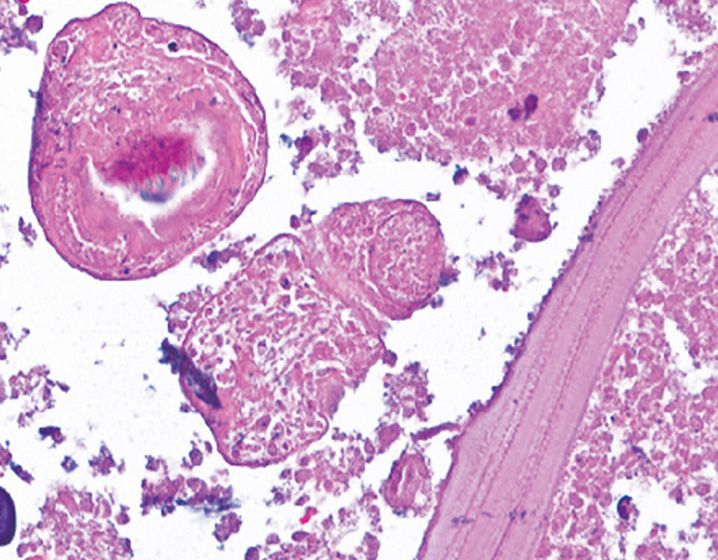
29. A duodenal biopsy from a patient with history of diarrhea is shown in Figure 13-6. Which of the following nematodes is responsible for the patient’s symptom and will most likely result in a stage of autoinfection?
(A) Ascaris lumbricoides
(B) Ancylostoma duodenale
(C) Enterobius vermicularis
(D) Strongyloides stercoralis
(E) Trichuris trichiura
30. A 30-year-old man presents with epigastric pain, nausea, and vomiting within 12 hours of consuming sushi. Endoscopic examination shows mucosal edema, hemorrhage, and slightly thickened gastric folds. Which of the following nematodes is most likely to be seen in the tissue sections from his stomach?
(A) Anisakis simplex
(B) Ascaris lumbricoides
(C) Enterobius vermicularis
(D) Strongyloides stercoralis
(E) Trichuris trichiura
31. Which primary immunodeficiency disorder results from mutation in the TNFRSF13B gene and is associated with celiac disease as its most common noninfectious GI complication?
(A) Common variable immunodeficiency
(B) Hyper-IgM syndrome
(C) Selective IgA deficiency
(D) Severe combined immunodeficiency
(E) X-linked agammaglobulinemia
32. Adult patients of common variable immunodeficiency are at risk for all of the following disorders, except
(A) B-cell non-Hodgkin lymphoma
(B) Colonic adenocarcinoma
(C) Gastric adenocarcinoma
(D) Small bowel adenocarcinoma
(E) Nodular lymphoid hyperplasia
33. Which chronic relapsing vasculitis is associated with oral aphthous ulcers, perianal disease, and ulcerative lesions of the GI tract that mimic Crohn’s disease?
(A) Behçet’s disease
(B) Churg-Strauss syndrome
(C) Microscopic polyangiitis
(D) Polyarteritis nodosa
(E) Wegener’s granulomatosis
34. Brown bowel syndrome is characterized by all the following clinicopathologic features, except
(A) Accumulation of lipofuscin within muscularis propria
(B) It is a congenital disorder
(C) It is commonly associated with Vitamin E deficiency
(D) It most commonly involves the small bowel
(E) The accumulated pigment is Periodic acid Schiff positive
35. In which part of the colon are muciphages most commonly found?
(A) Ascending colon
(B) Ileocecal valve
(C) Rectum
(D) Sigmoid colon
(E) Transverse colon
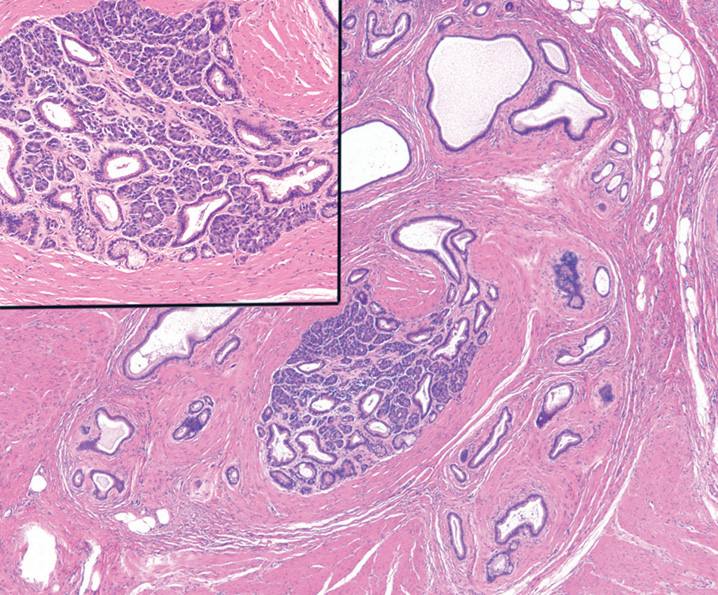
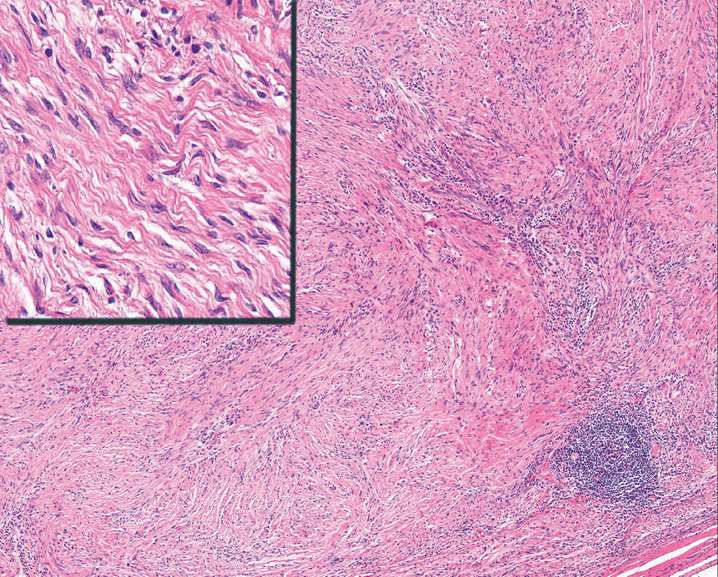
36. Figure 13-7 shows a submucosal tumor resected from a 40-year-old man. What is its most common location in the GI tract?
(A) Esophagus
(B) Colon
(C) Rectum
(D) Small bowel
(E) Stomach
37. Which of the following cells are increased in biopsies obtained from patients with irritable bowel syndrome and diarrhea?
(A) Eosinophils
(B) Lymphocytes
(C) Mast cells
(D) Neutrophils
(E) Plasma cells
38. Which of the following findings is not associated with achalasia?
(A) Cytoplasmic vacuolation of myocytes
(B) Inflammatory infiltrate composed of CD20-positive lymphocytes
(C) Lymphocytic ganglionitis
(D) Near total absence of myenteric ganglion cells
(E) Squamous epithelial hyperplasia and intraepithelial lymphocytosis
39. All the listed conditions have an association with Hirschsprung’s disease, except
(A) Down syndrome
(B) Multiple endocrine neoplasia
(C) Neurofibromatosis
(D) Neuroblastoma
(E) Turner syndrome
40. In a rectal suction biopsy, which of the following histologic findings supports a diagnosis of Hirschsprung’s disease?
(A) Lack of ganglion cells
(B) Lack of interstitial cells of Cajal
(C) Lack of neural plexuses
(D) Lymphocytic ganglionitis
(E) Submucosal fibrosis
41. Which of the following findings represents the most commonly encountered variation of the omphalomesenteric (vitelline) duct remnant?
(A) Meckel’s diverticulum
(B) Omphalomesenteric cyst
(C) Omphalomesenteric fistula
(D) Umbilical polyp
(E) Umbilical sinus
42. What is the most common type of heterotopic mucosa/epithelium found in a Meckel’s diverticulum?
(A) Biliary
(B) Colonic
(C) Duodenal
(D) Gastric
(E) Pancreatic
43. A 3-week-old boy with history of refractory diarrhea undergoes a duodenal biopsy that shows severe villous atrophy without crypt hyperplasia, increased apoptosis, or inflammation. There is no evidence of intraepithelial lymphocytosis. A PAS stain shows absence of a distinct brush border. What is the diagnostic test of choice?
(B) Serum anti-enterocyte antibody
(C) Serum gastrin
(D) Serum IgA
(E) Serum tissue transglutaminase
44. A 15-year-old boy with malabsorption is suspected to have autoimmune enteropathy. All the following findings are associated with this entity, except
(A) Anti-enterocyte antibodies
(B) Anti-goblet cell antibodies
(C) Increased crypt apoptosis
(D) Marked surface intraepithelial lymphocytosis
(E) Minimal response to gluten-free diet
45. An infant with very low birth weight is admitted with lethargy, abdominal distention, and absent bowel sounds. Imaging studies reveal changes consistent with pneumatosis. Which part of the bowel is most frequently involved by the condition described here?
(A) Descending colon
(B) Jejunum
(C) Ileocecal region
(D) Ileum
(E) Rectum
46. All the choices listed below are categorized as secondary causes of intestinal lymphangiectasia, except
(A) Constrictive pericarditis
(B) Lymphangioma
(C) Mesenteric tuberculosis
(D) Milroy disease
(E) Neuroblastoma
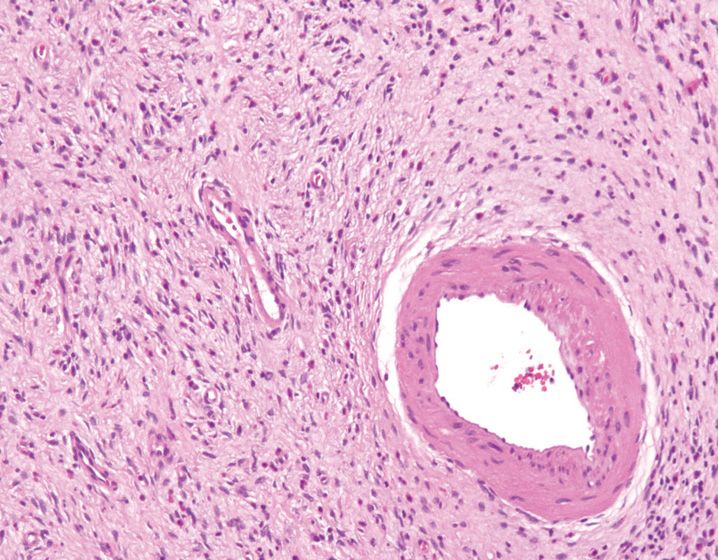
47. Which of the following choices describes a bleeding ulcer that is caused when an ulcer erodes into a single, unusually large submucosal mural arteriole?
(A) Cameron’s ulcer
(B) Chemical injury-induced ulcer
(C) Dieulafoy’s lesion
(D) Stress ulcer
(E) Variceal ulcer
48. A patient with cirrhosis undergoes endoscopic evaluation for gastrointestinal bleeding. The stomach shows a mosaic mucosal pattern and the biopsy reveals numerous ectatic capillaries and venules within the lamina propria, without evidence of vascular thrombi. What is the most likely cause of the gastrointestinal bleeding?
(A) Chronic gastritis
(B) Gastric antral vascular ectasia
(C) Ischemia
(D) Peptic ulcer disease
(E) Portal hypertensive gastropathy
49. A gastric biopsy from a 45-year-old man with iron deficiency anemia and an endoscopic appearance of linear mucosal hyperemia is shown in Figure 13-8. What is the most likely cause of patient’s anemia?
(A) Chronic gastritis
(B) Gastric antral vascular ectasia
(C) Hereditary hemorrhagic telangiectasia
(D) Portal hypertensive gastropathy
(E) Reactive gastropathy
50. What is the most common cause of lower gastrointestinal tract bleeding?
(A) Angiodysplasia
(B) Arteriovenous malformation
(C) Diverticular disease
(D) Hemorrhoids
(E) Ulcerative colitis
51. All of the features listed below are associated with angiodysplasia, except
(A) It is a developmental disorder
(B) It primarily affects elderly patients
(C) It is often located in the right colon
(D) It is characterized by dilated submucosal blood vessels
(E) It is a common source of bleeding in patients with renal failure
52. Which of the following drugs/medications causes “diaphragm disease”?
(A) Iron pills
(B) Laxatives
(C) Non-steroidal anti-inflammatory drugs
(D) Oral contraceptives
(E) Proton pump inhibitors
53. Which of the following etiologies would be categorized as an arterial cause of gastrointestinal ischemia?
(A) Buerger’s disease
(B) Behçet’s disease
(C) Chronic radiation injury
(D) Idiopathic myointimal hyperplasia of mesenteric veins
(E) Portal hypertension
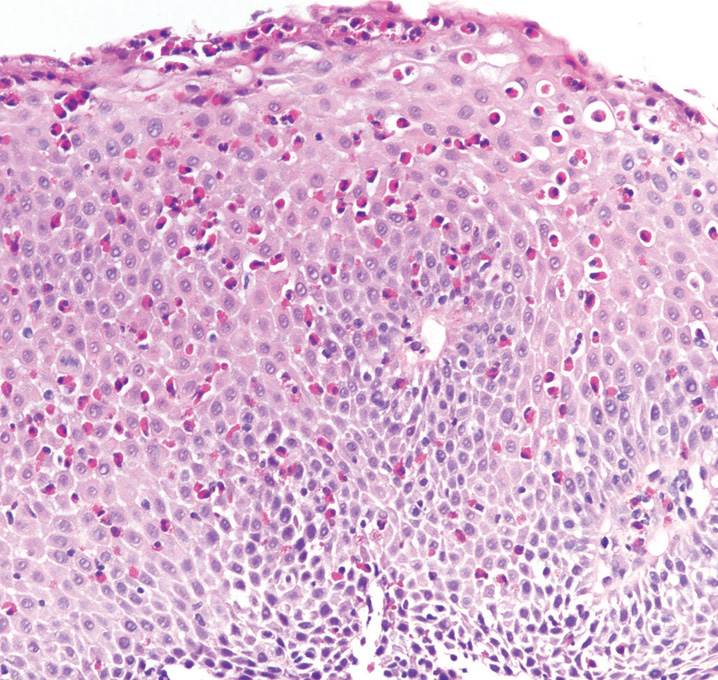
54. Which of the listed histologic features favors squamous dysplasia over reactive squamous hyperplasia?
(A) Irregular papillae
(B) Lack of atypical mitosis
(C) Maintenance of nuclear polarity
(D) Non-overlapping nuclei
(E) Regular nuclear membranes
55. A mid-esophageal biopsy from a 30-year-old man with history of dysphagia is shown in Figure 13-9. What is the characteristic endoscopic finding associated with this entity?
(A) Erosions
(B) Mass
(C) Rings and furrows
(D) Salmon-colored mucosa
(E) Ulcer
56. In evaluating biopsy from a patient suspected to have Barrett’s esophagus, which of the following histologic findings favors the presence of pseudo-goblet cells over true goblet cells?
(A) Alcian-blue reactivity at pH 2.5
(B) Blue cytoplasm
(C) Continuous distribution
(D) Eccentric, compressed nuclei
(E) Rounded shape of the cell
57. The esophageal biopsy shown in Figure 13-10 was obtained from a patient with chronic reflux and ulcerated salmon-colored mucosa on endoscopy. What is the best diagnosis?
(A) Barrett’s esophagus, negative for dysplasia
(B) Barrett’s esophagus, indefinite for dysplasia
(C) Barrett’s esophagus with high-grade dysplasia
(D) Barrett’s esophagus with low-grade dysplasia
(E) Intramucosal adenocarcinoma
58. Which of the following drugs/chemicals is associated with changes shown in this biopsy? (Figure 13-11)
(A) Alcohol
(B) Colchicine
(C) Iron
(D) Non-steroidal anti-inflammatory drugs
(E) Proton pump inhibitor
59. Which of the following etiologies is least likely to cause acute hemorrhagic gastritis?
(A) Alcohol
(B) Allergy
(C) Burns
(D) Non-steroidal anti-inflammatory drugs
(E) Stress
60. The campylobacter organism-like (CLO) test detects which of the following enzymes produced by Helicobacter pylori?
(A) Ammonia
(B) cag A toxin
(C) Phospholipase
(D) Urease
(E) vac A toxin
61. In the setting of Helicobacter pylori gastritis, the presence of which of the following histologic findings suggests therapy failure and antibiotic resistance?
(A) Granulomas
(B) Intestinal metaplasia
(C) Lymphocytes
(D) Neutrophils
(E) Plasma cells
62. Which of the following histologic findings in a gastric biopsy is considered to be specific for Helicobacter pylori infection?
(A) Intraepithelial lymphocytes
(B) Intestinal metaplasia
(C) Lymphoid follicle formation
(D) Neutrophils
(E) Superficial lamina propria inflammation
63. In the setting of Helicobacter pylori gastritis, all of the listed findings are highly suspicious for the presence of extranodal marginal zone B-cell lymphoma, except
(A) Active gastritis with intestinal metaplasia
(B) Endoscopic evidence of a mass/nodule
(C) Expansile inflammatory infiltrate of uniform-appearing cells
(D) Lymphoepithelial lesions with glandular disruption
(E) Monocytoid appearance of lymphocytes
64. Which specific pattern of Helicobacter pylori gastritis is associated with a high risk for development of intestinal-type dysplasia and gastric adenocarcinoma?
(A) Antral-predominant nonatrophic Helicobacter pylori gastritis
(B) Antrum-restricted atrophic Helicobacter pylori gastritis
(C) Corpus-predominant Helicobacter pylori gastritis
(D) Multifocal atrophic Helicobacter pylori gastritis
(E) Non-atrophic pangastritis
65. A gastric antral biopsy obtained from a 72-year-old woman shows superficial lymphoplasmacytic inflammatory infiltrate with focal active gastritis and intestinal metaplasia. All the following are possible explanations for the inability to demonstrate Helicobacter pylori, except
(A) Low bacterial load
(B) Presence of intestinal metaplasia
(C) Proton pump inhibitor use
(D) Recent antibiotic use
(E) Use of immunohistochemical stain for H. pylori
66. A 10-year-old boy with history of nausea and vomiting undergoes a gastric biopsy, which is depicted in Figure 13-12. He loves to play with his pets that include dogs, cats, and parakeets. All the following statements are true regarding this organism, except
(A) It causes severe gastritis
(B) It has a patchy pattern of mucosal involvement
(C) It has 5–7 spirals
(D) It is difficult to culture
(E) It measures 5–9 microns in length
67. A gastric ulcer is more likely to be benign when the following features are present, except
(A) Located close to the incisura angularis
(B) Located on the lesser curvature of the antrum
(C) Ranges in size from 0.5 to 2.0 cm in diameter
(D) Shows heaped up mucosal borders with irregular rugal folds
(E) Shows sharply demarcated boundaries
68. A 70-year-old woman presents with long-standing anemia and early satiety. A biopsy from the gastric body is shown in Figure 13-13. The gastric antrum was completely normal. No Helicobacter pylori organisms were identified. Which of the following serologic abnormalities is least likely to be present in this patient?
(A) Achlorhydria
(B) Hypochlorhydria
(C) Hypergastrinemia
(D) Hypogastrinemia
(E) Low serum pepsinogen I level
69. Enterochromaffin cell-like hyperplasia is least likely to be associated with which of the following conditions?
(A) Autoimmune gastritis
(B) Multifocal atrophic Helicobacter pylori gastritis
(C) Multiple endocrine neoplasia
(D) Non-steroidal anti-inflammatory drug-related gastritis
(E) Zollinger-Ellison syndrome
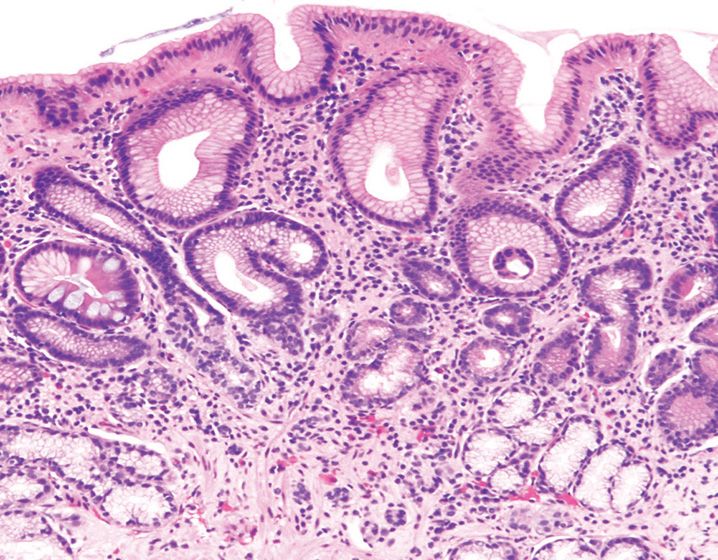
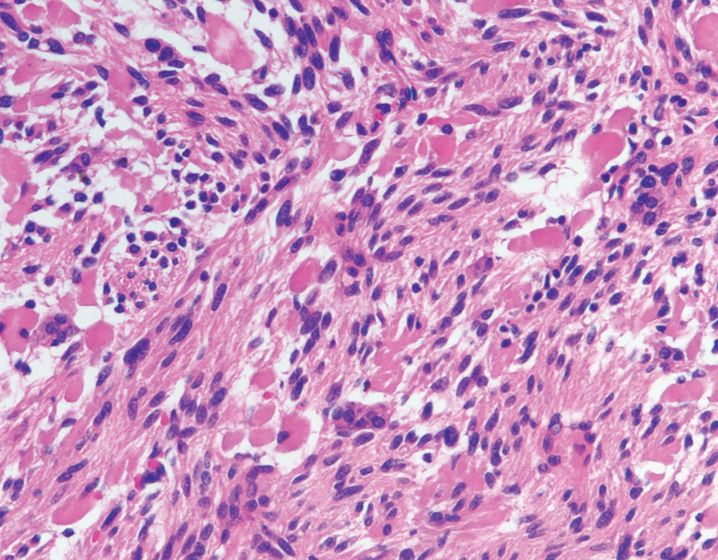
70. The pattern of mucosal injury depicted in Figure 13-14 is least likely to be associated with which of the following conditions?
(A) Celiac disease
(B) Extranodal marginal zone B-cell lymphoma
(C) Helicobacter pylori gastritis
(D) Ménétrier’s disease
(E) Non-steroidal anti-inflammatory drug-related gastritis
71. A gastric biopsy from a 70-year-old man with osteoarthritis and chronic non-steroidal anti-inflammatory drug use is shown in Figure 13-15. All the following pathologic features are helpful in diagnosing this pattern of injury, except
(A) Crowded glands with angulated profiles
(B) Foveolar hyperplasia
(C) Mucin depletion
(D) Nuclear hyperchromasia
(E) Smooth muscle proliferation within lamina propria
72. Toxic level of which of the following drugs is associated with this biopsy finding? (Figure 13-16)
(A) Alcohol
(B) Colchicine
(C) 5-FU
(D) Non-steroidal anti-inflammatory drugs
(E) Proton pump inhibitors
73. All the following pathologic findings favor chemo-radiation atypia over a neoplastic process, except
(A) Angulated and crowded glandular architecture
(B) Cytoplasmic vacuolation
(C) Large, irregular nuclei with smudged chromatin pattern and low N:C ratio
(D) Presence of surface epithelial maturation
(E) Stromal atypia
74. Which of these features is not helpful in distinguishing esophageal columnar metaplasia from gastric carditis?
(A) Active inflammation
(B) Hybrid glands
(C) Multilayered epithelium
(D) Presence of esophageal glands and ducts
(E) Squamous mucosa overlying intestinalized glands
75. In a patient suspected to have gluten-sensitive enteropathy, which of the listed endoscopic and pathologic findings would argue against this diagnosis?
(A) Expansion of the lamina propria by plasma cells and lymphocytes
(B) Increased CD20-positive lymphocytes within the surface epithelium
(C) Involvement of proximal jejunum
(D) Scalloped appearance of the duodenal mucosa
(E) Villous blunting
76. In a duodenal biopsy, which of the following entities is not associated with the findings of villous blunting and intraepithelial lymphocytosis?
(A) Autoimmune enteropathy
(B) Helicobacter pylori gastritis
(C) Primary intestinal lymphangiectasia
(D) Protein intolerance
(E) Tropical sprue
77. Which of the following segments of gastrointestinal tract is most commonly involved by eosinophilic gastroenteritis?
(A) Colon
(B) Duodenum
(C) Esophagus
(D) Ileum
(E) Stomach
78. A small bowel resection specimen from a patient suspected to have Crohn’s disease would show all the following features, except
(A) Circumferential ulcers
(B) Cobblestone appearance of the mucosa
(C) Fat wrapping
(D) Fistula formation
(E) Strictures
79. Which of the following histologic findings would be very unusual for a diagnosis of Crohn’s disease?
(A) Epithelioid granulomas
(B) Fissuring ulcers
(C) Lymphocytic phlebitis
(D) Transmural lymphoid aggregates
(E) Neural hypertrophy and thickening of the muscularis mucosae
80. A 24-year-old man with history of peripheral edema and steatorrhea undergoes small bowel resection for symptoms of obstruction. Based on Figure 13-17, what is the most likely diagnosis?
(A) Adenocarcinoma
(B) Cavernous lymphangioma
(C) Crohn’s disease
(D) Diaphragm disease
(E) Intestinal tuberculosis
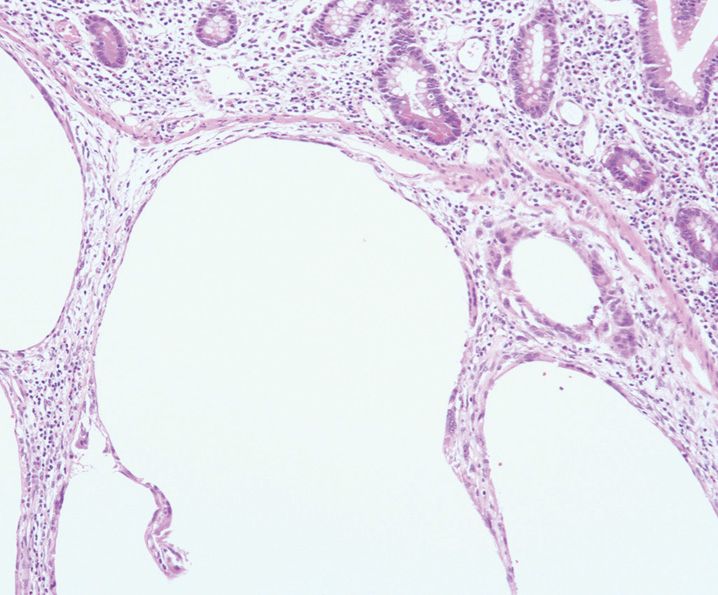
81. The pathologic finding depicted in Figure 13-18 occurs in the setting of all the following underlying intestinal diseases, except
(A) Adenocarcinoma
(B) Diverticular disease
(C) Infectious colitis
(D) Idiopathic inflammatory bowel disease
(E) Neonatal necrotizing enterocolitis
82. Which of the following histologic findings is the most reliable marker of chronic mucosal injury/chronic colitis?
(A) Crypt abscess formation
(B) Crypt architectural distortion
(C) Cryptitis
(D) Granulomas
(E) Superficial-predominant lymphoplasmacytic infiltrate
83. Which of the following pathologic features is not typical for untreated ulcerative colitis?
(A) Backwash ileitis
(B) Chronic active colitis
(C) Crypt rupture-associated granulomas
(D) Patchy and segmental involvement
(E) Rectal involvement
84. In patients with ulcerative colitis, which of the following risk factors is considered to be the strongest risk factor for development of dysplasia/carcinoma?
(A) Alcohol use
(B) Extent and severity of disease
(C) Family history of sporadic colon cancer
(D) Primary sclerosing cholangitis
(E) Smoking
85. Per 2010 American Gastroenterological Association (AGA) guidelines, the duration of disease after which patients with ulcerative colitis need to be enrolled in an endoscopic surveillance program is
(A) 1 year
(B) 2 years
(C) 5 years
(D) 8 years
(E) 10 years
86. A 70-year-old woman with refractory diarrhea undergoes colonoscopic examination that shows no mucosal abnormalities. A biopsy from left colon is shown in Figure 13-19. All the following features are diagnostic of this entity, except
(A) Basal lymphoplasmacytosis
(B) Increased intraepithelial lymphocytes
(C) Normal to slightly distorted crypt architecture
(D) Pseudomembrane formation and linear mucosal breaks
(E) Thickening of subepithelial collagen table
87. Which of the following pathologic findings favors a diagnosis of diverticular disease-associated colitis over idiopathic inflammatory bowel disease?
(A) Bearclaw-like ulcers
(B) Fistula formation
(C) Segmental disease with fat wrapping
(D) Rectal sparing
(E) Transmural lymphoid aggregates
88. A patient with a history of bone marrow transplant (8 months ago) undergoes colonoscopy for evaluation of diarrhea. A biopsy obtained from the sigmoid colon shows increased numbers of eosinophils within the lamina propria and prominent crypt apoptotic activity. The patient has been compliant with his medications. What is the most likely cause of his symptoms?
(A) Antibiotics
(B) Chemotherapy
(C) Graft-versus-host disease
(D) Mycophenolate mofetil-associated colitis
(E) Non-steroidal anti-inflammatory drugs
89. All the following histologic features are pathognomonic of mucosal prolapse syndrome/solitary rectal ulcer syndrome, except
(A) Always associated with an ulcer
(B) History of excessive straining
(C) Mass lesions may mimic carcinoma
(D) More common in females
(E) Usually located in the rectum
90. Which of the following pathologic findings favors a diagnosis of adenocarcinoma over colitis cystica profunda?
(A) Discrete rim of lamina propria around the glands
(B) Evidence of previous injury such as radiation vasculopathy, hemosiderin-laden macrophages
(C) Irregular and infiltrative glandular contours lined by dysplastic epithelium
(D) Mucin-filled cysts
(E) Polypoid configuration
91. Fibrous obliteration of the appendiceal lumen results from replacement of the entire lumen and underlying crypts by spindle cells. Which immunohistochemical marker is often expressed by this spindle cell proliferation?
(A) Caldesmon
(B) Cytokeratin
(C) Desmin
(D) S-100 protein
(E) Synaptophysin
92. What is the most common parasitic infection of vermiform appendix?
(A) Ancylostoma duodenale
(B) Ascaris lumbricoides
(C) Enterobius vermicularis
(D) Strongyloides stercoralis
(E) Trichuris trichiura
93. An appendectomy specimen from a patient with history of rupture 4 weeks ago, and subsequent antibiotic therapy, is most likely to show which of the following histologic findings?
(A) Cryptitis
(B) Eosinophilic inflammatory infiltrate
(C) Granulomatous inflammation
(D) Lymphoid hyperplasia
(E) Periappendicitis
94. Histologic evaluation of one of several nodular esophageal lesions shows prominent intracytoplasmic glycogen. Based on this finding, which of the following syndromes should be suspected?
(A) Cowden syndrome
(B) Familial adenomatous polyposis
(C) Gardner syndrome
(D) Neurofibromatosis
(E) Turcot syndrome
95. The gastric polyp shown here (Figure 13-20) is least likely to be associated with which of the following conditions?
(A) Autoimmune gastritis
(B) Familial adenomatous polyposis
(C) Helicobacter pylori gastritis
(D) Non-steroidal anti-inflammatory drug-induced gastritis
(E) Post-Billroth II gastrectomy
96. Which of the following causes of enlarged gastric folds is associated with protein-losing enteropathy, foveolar hyperplasia, and excessive secretion of transforming growth factor-alpha?
(A) Chronic gastritis
(B) Lymphoma
(C) Ménétrier’s disease
(D) Signet ring cell carcinoma
(E) Zollinger-Ellison syndrome
97. Which of the following clinicopathologic features is not associated with fundic gland polyps arising in the setting of familial adenomatous polyposis?
(A) APC gene mutation
(B) Equal male:female ratio
(C) Less than 1% risk of developing dysplasia
(D) Often associated with multiple polyps
(E) Younger age at presentation
98. What is the best diagnosis for the submucosal gastric lesion depicted in Figure 13-21?
(A) Carcinoid tumor
(B) Gastritis cystica profunda
(C) Lymphangioma
(D) Pancreatic heterotopia
(E) Well-differentiated adenocarcinoma
99. A 65-year-old woman undergoes resection of a gastric polyp shown in Figure 13-22. Which of the following features is not typical of this entity?
(A) Antrum is the most common location for this lesion
(B) A subset of these lesions may show KIT mutation
(C) The lesional cells express CD34 and vimentin
(D) They are often submucosal in location
(E) They may occasionally arise in the small bowel
100. Gastric mucosal calcinosis most commonly occurs in which of the following disease settings?
(A) Acute myeloid leukemia
(B) End-stage renal disease
(C) Helicobacter pylori gastritis
(D) Liver failure
(E) Proton pump inhibitor use
101. In gastric mucosal hemosiderosis, what is the pattern of iron deposition observed in patients with systemic iron overload or hemochromatosis?
(A) Luminal
(B) Predominantly extracellular
(C) Predominantly glandular, diffuse
(D) Predominantly stromal, patchy
(E) Vascular
102. Hamartomatous polyps of the small intestine are most commonly associated with which of the following syndrome/condition?
(A) Cowden syndrome
(B) Cronkhite-Canada syndrome
(C) Inflammatory diseases such as Crohn’s disease
(D) Juvenile polyposis syndrome
(E) Peutz-Jeghers syndrome
103. A 14-year-old boy presents with small bowel obstruction and undergoes resection of an obstructing polypoid mass shown in Figure 13-23. He has numerous polyps within the small bowel. Which genetic mutation is associated with this condition?
(A) APC
(B) BMBR1A
(C) PTEN
(D) SMAD4
(E) STK11
104. Type-1 neurofibromatosis is associated with all of the following gastrointestinal neoplasms, except
(A) Ampullary adenocarcinoma
(B) Gangliocytic paraganglioma
(C) Gastrointestinal stromal tumor
(D) Inflammatory fibroid polyp
(E) Somatostatinoma
105. Which type of lymphoma most commonly presents as lymphomatous polyposis within the GI tract?
(A) Diffuse large B-cell lymphoma
(B) Follicular lymphoma
(C) Hodgkin lymphoma
(D) Mantle cell lymphoma
(E) Marginal zone lymphoma
106. Based on histologic features alone, which of the following findings favors a primary small bowel adenocarcinoma over metastatic adenocarcinoma involving the small bowel?
(A) Extensive angiolymphatic space invasion
(B) Extensive mural disease with minimal mucosal involvement
(C) Presence of a precursor lesion
(D) Signet ring cell morphology and a diffuse growth pattern
(E) Tumor multifocality
107. All the following statements regarding inflammatory polyps are true, except
(A) The stroma may harbor bizarre atypical cells that resemble a sarcomatous proliferation
(B) They are composed of mixture of inflamed lamina propria and dilated glandular elements
(C) They are exclusively associated with idiopathic inflammatory bowel disease (pseudopolyps)
(D) They may be histologically indistinguishable from juvenile polyps
(E) They usually do not have a tendency toward neoplastic progression
108. A 20-year-old man presents with multiple colonic hamartomatous polyps and is confirmed to have a mutation in the PTEN gene. He also has facial trichilemmomas. Besides hamartomatous polyps, which of the following colonic lesions is common in these patients?
(A) Adenomyoma
(B) Carcinoid
(C) Ganglioneuroma
(D) Inflammatory fibroid polyp
(E) Leiomyoma
109. A patient with multiple colonic polyps is clinically suspected to have Cronkhite-Canada syndrome. Which of the following features is least likely to be associated with this syndrome?
(A) Autosomal-dominant inheritance pattern
(B) Death resulting from malnutrition and bleeding
(C) Ectodermal abnormalities such as alopecia and nail dystrophy
(D) Esophageal sparing
(E) Presence of polyps that resemble juvenile polyps
110. During a routine colonoscopy, a 53-year-old man is found to have this 1.5 cm sessile polyp in the ascending colon (see Figure 13-24). Which of the following molecular alterations is most commonly associated with this lesion?
(A) APC mutation
(B) BRAF mutation
(C) KRAS mutation
(D) MSH2 mutation
(E) SMAD4 mutation
111. Resection of an esophageal cyst shows a unilocular cyst lined by ciliated columnar epithelium, with evidence of cartilage, smooth muscle, and mucous glands within the cyst wall. The cyst does not communicate with the esophageal lumen. What is the best designation for this cyst?
(A) Bronchogenic cyst
(B) Diverticulum
(C) Dorsal enteric cyst
(D) Duplication cyst
(E) Intramural cyst
112. Of the choices listed below, which is the most common type of heterotopic tissue found in the esophagus?
(A) Gastric
(B) Pancreatic
(C) Parathyroid
(D) Sebaceous
(E) Thyroid
113. Verrucous carcinoma of the esophagus is usually associated with all of the following features, except
(A) Accompanied by minimal cytologic atypia
(B) Locally aggressive neoplasm
(C) More common in males than females
(D) Often presents as a very large lesion
(E) Often present with distant metastasis
114. Which of the following features is not associated with CDH1 mutated gastric adenocarcinoma?
(A) Adjacent gastric mucosa is non-atrophic
(B) Age of presentation is 3rd–4th decade
(C) Gene penetrance varies from 70% to 80%
(D) Increased risk of lobular breast carcinoma
(E) Intestinal-type morphology
115. Which of the tumors listed below is the most common extracolonic malignancy arising in the setting of familial adenomatous polyposis?
(A) Anal squamous cell carcinoma
(B) Barrett’s adenocarcinoma
(C) Esophageal squamous cell carcinoma
(D) Gastric adenocarcinoma arising in fundic gland polyp
(E) Periampullary adenocarcinoma
116. All the following conditions are considered to be a significant risk factor for development of small intestinal adenocarcinoma, except
(A) Celiac disease
(B) Crohn’s disease
(C) Cronkhite-Canada syndrome
(D) Familial adenomatous polyposis
(E) Hereditary nonpolyposis colon cancer syndrome
117. What percentage of colon cancers arises as a result of chromosomal instability?
(A) 2%
(B) 15%
(C) 30%
(D) 50%
(E) 85%
118. Which of the following histologic types of colorectal cancer is more common in patients with longstanding ulcerative colitis?
(A) Adenosquamous carcinoma
(B) Medullary carcinoma
(C) Mucinous carcinoma
(D) Signet ring cell carcinoma
(E) Small cell carcinoma
119. All the listed pathologic features are associated with this colonic adenocarcinoma (see Figure 13-25) resected from a 40-year-old man, except
(A) Crohn’s-like lymphoid response
(B) Exophytic/polypoid configuration
(C) Located in the descending colon
(D) Mucinous differentiation in other areas
(E) Tumor heterogeneity
120. All the following statements regarding KRAS mutation analysis of colorectal neoplasms are true, except
(A) Codon 12 and 13 mutations are the most common activating mutations
(B) Presence of a KRAS mutation indicates response to cetuximab
(C) Sanger sequencing, pyrosequencing, and melt curve analysis are common techniques of analysis
(D) The test is performed on stage IV colorectal cancers
(E) The test may be performed on biopsy samples as well as cytology specimens
121. An appendectomy specimen from a 42-year-old man reveals a carcinoid tumor. Which of the following pathologic features is not considered to be an indication for right hemicolectomy?
(A) Extensive angiolymphatic space invasion
(B) Mesoappendiceal involvement
(C) Regional lymph node metastasis
(D) Size of 1.0 cm
(E) Rupture with presence of extraappendiceal tumor
122. What percentage of gastrointestinal tumors is known to harbor KIT mutations?
(A) 5%
(B) 10%
(C) 25%
(D) 50%
(E) 85%
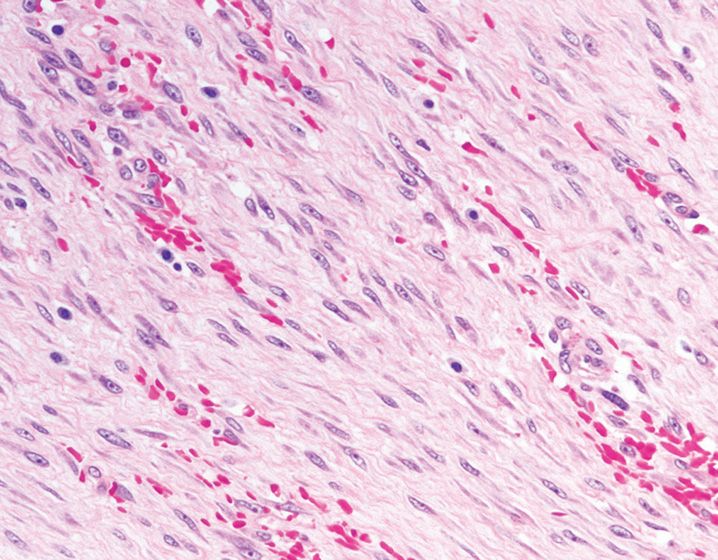
123. The submucosal tumor shown in Figure 13-26 is diffusely positive for DOG1. The tumor most likely originates from which part of the GI tract?
(A) Esophagus
(B) Ileum
(C) Omentum
(D) Rectum
(E) Stomach
124. The gastric tumor shown in this figure (Figure 13-27) was resected from a 52-year-old man. What is the most likely diagnosis?
(A) Fibromatosis
(B) Gastrointestinal stromal tumor
(C) Inflammatory fibroid polyp
(D) Leiomyoma
(E) Schwannoma
125. A mesenteric nodule resected from a 40-year-old woman is shown in Figure 13-28. The lesion was immunoreactive for β-catenin. Which of the following clinicopathologic features is not associated with this entity?
(A) Commonly associated with Turcot syndrome
(B) Composed of bland spindle/stellate cells with scattered dilated, thin-walled vessels
(C) Patients are usually asymptomatic
(D) They commonly arise in the mesentery and pelvis
(E) They typically infiltrate into adjacent soft tissue and bowel wall
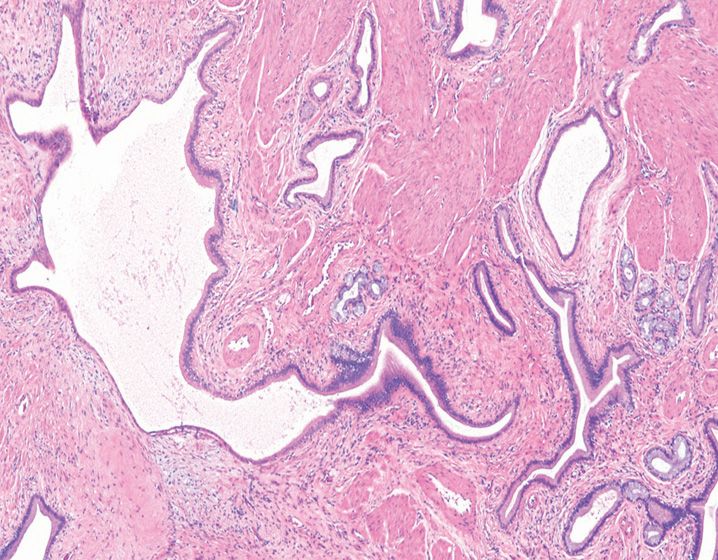
126. During a Whipple procedure for a pancreatic head mass, the surgeon notices this 2.0 cm lesion in the fundus of the gallbladder (see Figure 13-29). The surgeon is very worried about this lesion and requests a frozen section. What is your diagnosis?
(A) Adenomyoma
(B) Chronic cholecystitis
(C) Gallbladder adenocarcinoma
(D) Hyperplastic Luschka’s ducts
(E) Metastatic pancreatic adenocarcinoma
127. All the following histologic features on a pancreatic resection margin sample favor a diagnosis of adenocarcinoma, except
(A) Incomplete glandular lumens
(B) Irregular and angulated growth pattern
(C) Nuclear size variation of 2:1
(D) Presence of atypical glands adjacent to muscular arteries and fat
(E) Presence of perineural invasion
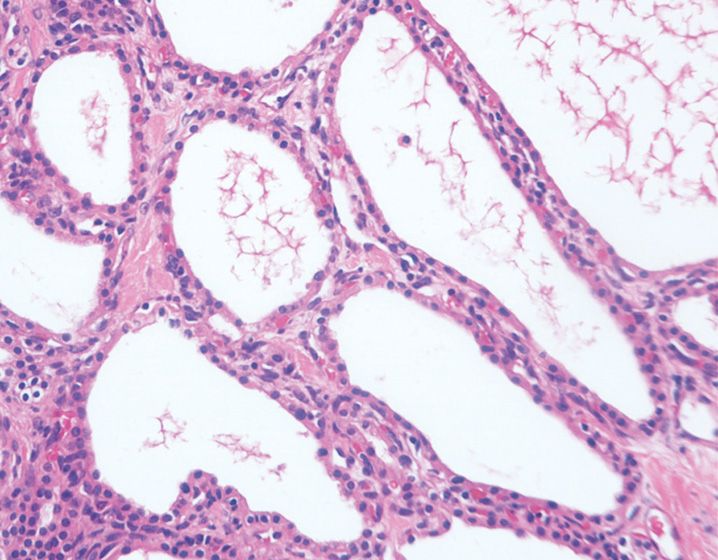
128. A 65-year-old woman undergoes resection of this pancreatic mass (Figure 13-30). What is the best diagnosis?
(A) Intraductal papillary mucinous neoplasm
(B) Lymphoepithelial cyst
(C) Microcystic serous cystadenoma
(D) Mucinous cystic neoplasm
(E) Pancreatic adenocarcinoma with cystic degeneration
129. An incidental histologic lesion characterized by tall columnar mucinous cells with well-polarized nuclei, slight nuclear stratification, and papillary formation, is encountered in a Whipple resection specimen. What is the best classification for this lesion?
(A) Pancreatic intraepithelial neoplasia IA
(B) Pancreatic intraepithelial neoplasia IB
(C) Pancreatic intraepithelial neoplasia II
(D) Pancreatic intraepithelial neoplasia III
(E) Intraductal papillary mucinous neoplasm
130. A 50-year-old woman undergoes resection of a cystic lesion located in the tail of pancreas. Microscopically, the cyst wall is lined by mucinous epithelium and shows variable amount of ovarian-type subepithelial stroma. What is the best diagnosis for this cystic lesion?
(A) Cystic neuroendocrine tumor
(B) Cystic pancreatic adenocarcinoma
(C) Intraductal papillary mucinous neoplasm
(D) Microcystic serous cystadenoma
(E) Mucinous cystic neoplasm
131. Based on (Figure 13-31), what would be this patient’s demographic profile and gross appearance of this lesion?
(A) A 2-year-old boy with pancreatic body mass
(B) A 30-year-old woman with a well-circumscribed hemorrhagic and cystic lesion in the body of pancreas
(C) A 50-year-old man with tan-white lesion in the body of pancreas
(D) A 62-year-old woman with a cystic pancreatic tail mass
(E) A 75-year-old man with a solid pancreatic head mass
132. A liver biopsy from a 20-year-old man shows extensive parenchymal necrosis involving approximately 80% of the parenchyma. Which of the following is the least likely etiology for this histologic finding?
(A) Acute viral hepatitis E infection
(B) Autoimmune hepatitis
(C) Drug toxicity
(D) Primary biliary cirrhosis
(E) Wilson’s disease
133. Based on the findings shown in Figure 13-32, what is the most likely etiology for this histologic change?
(A) Cytomegalovirus infection
(B) Epstein-Barr virus infection
(C) Hepatitis B infection
(D) Hepatitis E infection
(E) Yellow fever
134. Which histologic finding distinguishes chronic hepatitis due to primary biliary cirrhosis from chronic viral hepatitis C-induced disease?
(A) Ductopenia
(B) Lobular activity
(C) Lobular granulomas
(D) Portal interface activity
(E) Steatosis
135. A 10-year-old boy presents with recent onset fever and increased serum aminotransferases. Which of the following histologic findings would support the clinical impression of Epstein-Barr virus hepatitis?
(A) Apoptotic hepatocytes
(B) Cholestasis
(C) Granulomas
(D) Sinusoidal lymphocytosis
(E) Steatosis
136. A 40-year-old man presents with recent onset abdominal pain, fever, and hepatomegaly. Imaging studies reveal a multiloculated cyst with rounded densities. A histologic section from this lesion is shown in Figure 13-33. Which parasitic organism causes this condition?
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree