5 Gastrointestinal disease
Symptoms
Dyspepsia and indigestion
Treatment
Treatment is with antacid therapy (Table 5.1).
| Class of drug | Drug | Dose |
|---|---|---|
| H2-receptor antagonists | Cimetidine | 400 mg twice daily |
| Famotidine | 40 mg daily | |
| Nizatidine | 300 mg daily | |
| Ranitidine | 300 mg daily | |
| Proton pump inhibitors | Esomeprazole | 20 mg daily |
| Lansoprazole | 30 mg daily | |
| Omeprazole | 20 mg daily | |
| Pantoprazole | 40 mg daily | |
| Rabeprazole | 20 mg daily | |
| Antacids | Aluminium hydroxide | 10–20 mL 3 times daily |
| Magnesium carbonate | 10 mL 3 times daily | |
| Magnesium trisilicate | 10–20 mL 3 times daily | |
| Aluminium and magnesium complexes | 10 mL between meals and at bedtime | |
| Others | Alginates and antacids | 2 tablets twice daily |
| Chelates and complexes, e.g. tripotassium, dicitratobismuthate, sucralfate | 2 tablets twice daily |
Nausea and vomiting
Treatment
Many patients require no therapy. Food is usually withheld and fluids only are allowed. With more persistent vomiting, IV fluids, e.g. 0.9% saline (p. 369), are given for dehydration and correction of electrolyte abnormalities. A naso-gastric tube is inserted if there is bowel obstruction.
Diarrhoea
Acute diarrhoea
• Treatment
All produce constipation if given frequently.
• Specific therapy
Diarrhoea in patients with HIV infection
Chronic diarrhoea is a common symptom in patients with HIV infection (p. 96). Cryptosporidium is the commonest pathogen isolated. Other infective causes include cytomegalovirus, Mycobacterium avium and Giardia intestinalis. Stool culture with examination for ova, cysts and parasites should be performed, together with flexible sigmoidoscopy/colonoscopy and biopsy.
Chronic diarrhoea
Chronic diarrhoea refers to diarrhoea of more than 4 weeks’ duration. It can be due to a variety of causes (usually non-infective) including inflammation (inflammatory bowel disease), drugs (metformin, statins), functional factors, malabsorption or cancer (change in bowel habit), the treatments for which are described elsewhere.
• Clinical features
Constipation
Treatment
• Laxatives (Box 5.2)
Gastro-oesophageal reflux disease
Reflux is extremely common in the general population, causing mild indigestion and heartburn.
Investigations
Under the age of 45 years, all patients should be treated initially without investigations, unless there are alarm symptoms (Box 5.1).
Treatment
• Medical treatment (Table 5.1)
Non-erosive reflux disease (NERD)
These cases include patients with reflux symptoms. They often do not respond to a PPI. Patients are usually female and often the symptoms are functional (p. 167).
Complications
Other oesophageal disorders
Achalasia
Treatment
Diffuse oesophageal spasm
This disorder causes chest pain and dysphagia, is diagnosed by oesophageal manometry and is characterized by simultaneous non-peristaltic oesophageal contractions occurring after 20% or more swallows. Barium swallow may show a corkscrew appearance. Nutcracker oesophagus is a variant of diffuse oesophageal spasm characterized by very high-amplitude peristalsis (> 200 mmHg).
Chemical oesophagitis
Peptic ulcer disease
Helicobacter pylori
• Non-invasive:
Aspirin and other NSAIDs
Prophylactic therapy
This is necessary for all high-risk patients, i.e. those over 65 years, those with a peptic ulcer history, particularly with complications, and patients on therapy with corticosteroids or anticoagulants. An alternative is to give a COX-2 NSAID, which causes less mucosal damage (p. 298), but long-term cardiovascular risk is a problem.
Complications of peptic ulcer
These include haemorrhage (p. 151).
Gastrointestinal haemorrhage
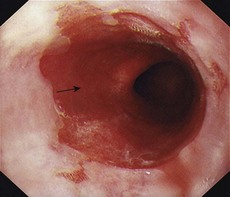
Acute upper gastrointestinal bleeding
Haematemesis is the vomiting of blood from a lesion proximal to the distal duodenum. Melaena is the passage of black tarry stools; the black colour is due to altered blood — 50 mL or more is required to produce this. Melaena can occur with bleeding from any lesion in areas proximal to and including the caecum.
Immediate management (Box 5.3)
Box 5.3 Management of acute gastrointestinal bleeding (see also Fig. 20.4)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree