Gastroesophageal Reflux Disease
Alexandros D. Polydorides, MD, PhD
Key Facts
Terminology
Symptoms, lesions, or complications due to reflux
Etiology/Pathogenesis
LES defects, hiatal hernia, ↑ fluid volume, inefficient gastroesophageal clearance, lifestyle
Clinical Issues
Damaged mucosa in GERD: Secondary infections
Evaluate for CMV, HSV, Candida
Complications (50% of symptomatic patients)
Asthma, aspiration pneumonia, polyps/stenosis of larynx, peptic stricture, Barrett, adenocarcinoma
Atypical/severe symptoms: Exclude stricture, cancer
Macroscopic Features
Erythema, friability, hemorrhage, erosion, ulcer
Usually present distally and taper off proximally
Microscopic Pathology
Characteristic findings but none specific for GERD
Neutrophils, lymphocytes, eosinophils (> 6/biopsy)
Superficial erosion, deep ulcer (exudate, granulation)
Balloon cells: Swollen cytoplasm, pyknotic nuclei
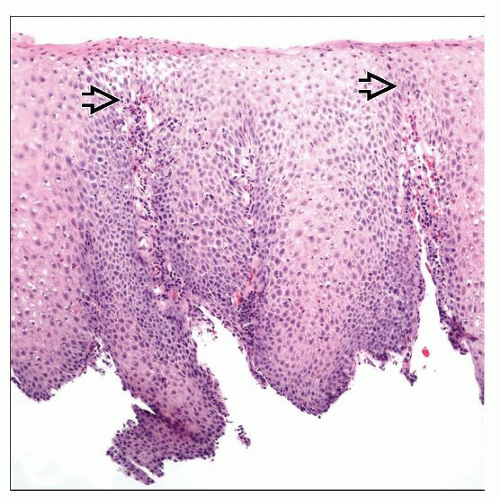
Hyperplasia of squamous epithelium
Subepithelial papillae, basal cell layer, acanthosis
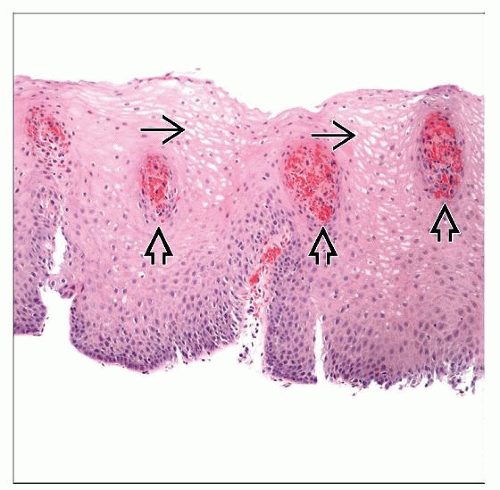
Mucosal capillary ectasia (“vascular lakes”)
Top Differential Diagnoses
Eosinophilic esophagitis
Pill, trauma, or drug-induced esophagitis
Diagnostic Checklist
Histologic changes may be patchy, endoscopy normal
Multiple biopsies recommended (distal esophagus)
Carditis common in GERD, distinguish from H. pylori
TERMINOLOGY
Abbreviations
Gastroesophageal reflux disease (GERD)
Definitions
Gastroesophageal reflux: Retrograde flow of gastric (or duodenal) contents into esophagus
GERD: Physical symptoms, endoscopic lesions, complications, or histopathologic alterations attributable to gastroesophageal reflux
Reflux esophagitis: Histologic changes (inflammation) in esophageal mucosa of GERD patients
ETIOLOGY/PATHOGENESIS
Infectious Agents
Current data: Industrialized nations (controversial)
Inverse relation between H. pylori infection rates and rising GERD incidence
H. pylori may exert protective effect from GERD
Multifactorial
Genetic, environmental factors thought to contribute
Risk Factors
Hiatal hernia, ↓ lower esophageal sphincter (LES) pressure, ↑ gastric fluid volume, inefficient clearance
Proposed Pathogenesis
Reflux is common, but damage does not usually occur
Offensive/defensive mechanism imbalance over time leads to damage
Offensive agents: Noxious elements (gastric contents)
Acid (HCl), pepsin (acid-activated protease)
Alkaline (bile) reflux compounds damage
Acid hypersecretion (Zollinger-Ellison syndrome)
Defensive mechanisms
Antireflux barrier: Limits refluxate frequency, volume
LES: ↓ pressure, incompetence, relaxation
Congenital esophageal or gastric abnormalities
Iatrogenic: Myotomy/resection, nasogastric tube
Luminal clearance: Limits refluxate/epithelium contact
Defective peristalsis, motility disorders (diabetes, alcoholic neuropathy, achalasia, scleroderma)
↑ gastric volume (saliva production), nonreducing hiatal hernia
Delayed gastric emptying: Gastroparesis, pyloric stenosis or dysfunction, stricture
Intraabdominal pressure: Obesity, ascites, pregnancy
Tissue resistance: Mucous, cell junctions, blood flow
Lifestyle: Smoking, alcohol, hot beverages, caffeine
Patient age, congenital defects (e.g., cystic fibrosis)
GERD: Inflammation, genesis of free radicals further damage LES, impair mucosal resistance
CLINICAL ISSUES
Epidemiology
Incidence
Prevalence: 3-36%
Industrialized nations: 10-20% have heartburn at least 1x a week, 4-10% daily
Age
All ages affected, even small children and infants
Ethnicity
Highest rate in North America, Europe (Caucasians, increasing frequency among Asians)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree