Objectives
- Understand the role of the gallbladder in concentrating bile and coordinating its secretion with ingestion of a meal
- Describe the molecular mechanisms whereby bile is concentrated during storage
- Discuss the mechanism and significance of gallbladder secretion
- Understand how bile remains isoosmolar during concentration
- Explain how contraction of the gallbladder is regulated
- Describe the molecular mechanisms whereby bile is concentrated during storage
- Explain why the gallbladder is vulnerable to the formation of cholesterol gallstones
- Describe the physiologic consequences of surgical removal of the gallbladder
- Understand the role of the sphincter of Oddi in regulating bile outflow into the intestine
Basic Principles of Gallbladder Function
 The gallbladder serves to store and concentrate bile coming from the liver in the period between meals. Gallbladder function therefore permits coordination of the secretion of a bolus of concentrated bile with the entry of dietary lipids into the small intestine. It is important to be aware, however, that the gallbladder is not essential to normal digestion and absorption of a meal. In the absence of a functioning gallbladder, the bile acid pool continues to cycle through the enterohepatic circulation and the majority of the bile acid pool is stored in the small intestine.
The gallbladder serves to store and concentrate bile coming from the liver in the period between meals. Gallbladder function therefore permits coordination of the secretion of a bolus of concentrated bile with the entry of dietary lipids into the small intestine. It is important to be aware, however, that the gallbladder is not essential to normal digestion and absorption of a meal. In the absence of a functioning gallbladder, the bile acid pool continues to cycle through the enterohepatic circulation and the majority of the bile acid pool is stored in the small intestine.
Functional Anatomy of the Gallbladder
The gallbladder is a muscular sac located just below the liver and lying adjacent to the liver’s surface. Its capacity is approximately 50 mL in adult humans. It is linked to the biliary system via the cystic duct, a bidirectional conduit for bile flow. During periods of fasting, bile secreted by the liver is diverted into the gallbladder on the basis of pressure relationships in the biliary system, as will be discussed in more detail later. On the other hand, when the gallbladder receives neurohumoral cues that fats are present in the small intestine, it contracts and bile flows out of the gallbladder and into the intestine via the cystic and common bile ducts.
The gallbladder has two functional layers. The innermost of these, facing the bile, is a columnar epithelium that participates actively in bile concentration. The tight junctions that link adjacent epithelial cells are among the most well-developed anywhere in the body, making the epithelium highly resistant to the passive flux of solutes. This “tight” epithelium prevents the passive loss of bile acid molecules and thus is essential to the ability of the gallbladder to concentrate the bile. It is likely also important in limiting the potentially deleterious effects of amphipathic bile acids. To this end, the epithelium also contains abundant goblet cells that secrete mucus, which is also believed to protect the epithelium from injury.
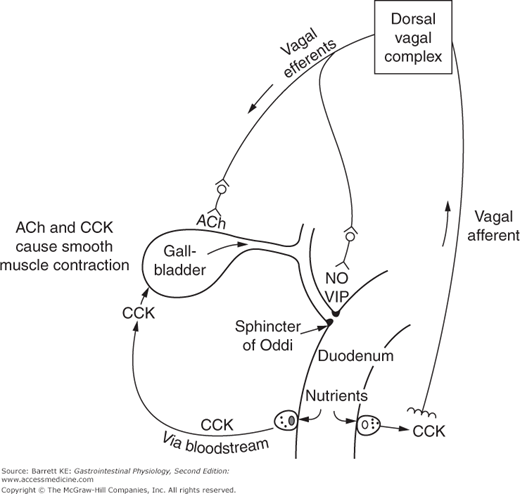
The epithelial layers are underlaid by smooth muscle that can alter the caliber of the gallbladder lumen according to the presence of neurohumoral stimuli. The muscle cells receive input from branches of the vagus nerve, and express cholinergic receptors to respond to released acetylcholine (ACh). They also express receptors for gastrointestinal hormones, and in particular for cholecystokinin (CCK1). As we learned earlier, this hormone is actually named for its ability to contract the gallbladder. However, the majority of the action of CCK on gallbladder motility is believed to be indirect, and mediated by the effects of this hormone on nerves that innervate the gallbladder, as well as on vagal afferents that travel from the duodenum and coordinate gallbladder emptying with the presence of nutrients in the gut lumen (Figure 12–1).
Figure 12–1.
Neurohumoral control of gallbladder contraction and biliary secretion. Nutrients in the duodenum lead to the release of cholecystokinin (CCK), which acts through both endocrine and neurocrine routes to activate gallbladder contraction and relax the sphincter of Oddi, resulting in the secretion of a bolus of concentrated bile into the duodenal lumen. Secondary neurotransmitters released by the enteric nervous system in response to a vago-vagal reflex include the excitatory neurotransmitter acetylcholine (ACh) and the inhibitory transmitters vasoactive intestinal polypeptide (VIP) and nitric oxide (NO).
Gallbladder Storage of Bile
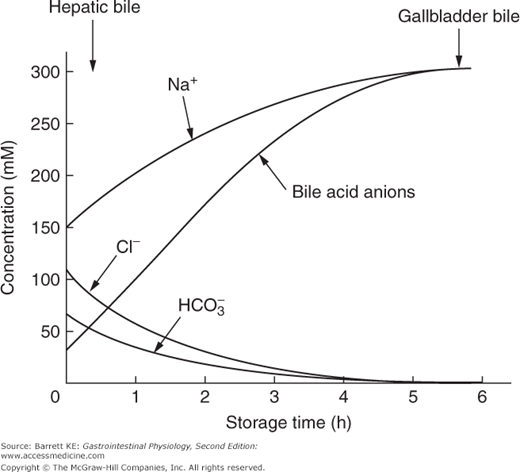
 Hepatic bile emerging from the biliary ducts is isotonic with plasma, with sodium as its major cation and chloride as its major anion. Bile acids are typically present at a concentration of approximately 30–50 mM; there are small amounts of potassium, calcium, and approximately 20–50 mM bicarbonate. After gallbladder storage, water is removed from the lumen and the concentration of bile acids is increased by approximately tenfold, whereas chloride and bicarbonate concentrations fall dramatically. On the other hand, the concentrations of all cations in the bile increase, although to a lesser degree than that of the bile acids indicating that cations are also subject to net absorption by the gallbladder epithelium. The concentration of calcium ions, which remains low, nevertheless increases disproportionately compared to that of sodium and potassium because of a phenomenon known as the Gibbs–Donnan equilibrium, where divalent cations are retained in a given compartment containing proteins more avidly than are monovalent anions. You may recall this concept from previous discussions of how plasma oncotic pressure is established, or the rules establishing the ionic composition of plasma versus the interstitial fluid. A figure comparing the composition of hepatic and gallbladder bile is shown as Figure 12–2.
Hepatic bile emerging from the biliary ducts is isotonic with plasma, with sodium as its major cation and chloride as its major anion. Bile acids are typically present at a concentration of approximately 30–50 mM; there are small amounts of potassium, calcium, and approximately 20–50 mM bicarbonate. After gallbladder storage, water is removed from the lumen and the concentration of bile acids is increased by approximately tenfold, whereas chloride and bicarbonate concentrations fall dramatically. On the other hand, the concentrations of all cations in the bile increase, although to a lesser degree than that of the bile acids indicating that cations are also subject to net absorption by the gallbladder epithelium. The concentration of calcium ions, which remains low, nevertheless increases disproportionately compared to that of sodium and potassium because of a phenomenon known as the Gibbs–Donnan equilibrium, where divalent cations are retained in a given compartment containing proteins more avidly than are monovalent anions. You may recall this concept from previous discussions of how plasma oncotic pressure is established, or the rules establishing the ionic composition of plasma versus the interstitial fluid. A figure comparing the composition of hepatic and gallbladder bile is shown as Figure 12–2.
 Despite the dramatic increase in the sum of anions and cations during gallbladder storage of bile, bile remains isotonic. How is this possible? The answer lies in the fact that the majority of the bile acid molecules are physically in the form of mixed micelles that also contain cholesterol and phosphatidylcholine. Once the critical micellar concentration is reached, the monomeric concentration of bile acids does not change. Any additional bile acid molecules are immediately incorporated into existing micelles. Osmolality is a colligative property, which means that each particle in a solution contributes the same amount of osmotic force, be it a molecule, ion, or micelle. This allows the osmolality of bile to remain constant despite its concentration. In addition, counterion binding to micelles may also further decrease the osmolality of the stored bile.
Despite the dramatic increase in the sum of anions and cations during gallbladder storage of bile, bile remains isotonic. How is this possible? The answer lies in the fact that the majority of the bile acid molecules are physically in the form of mixed micelles that also contain cholesterol and phosphatidylcholine. Once the critical micellar concentration is reached, the monomeric concentration of bile acids does not change. Any additional bile acid molecules are immediately incorporated into existing micelles. Osmolality is a colligative property, which means that each particle in a solution contributes the same amount of osmotic force, be it a molecule, ion, or micelle. This allows the osmolality of bile to remain constant despite its concentration. In addition, counterion binding to micelles may also further decrease the osmolality of the stored bile.
Bile also changes from being slightly alkaline (a result of bicarbonate secretion in the ductules) to slightly acidic. This may be important in reducing the risk of calcium precipitation, since calcium bicarbonate is more soluble than calcium carbonate. Bile acidification results from the activity of gallbladder epithelial cells, as will be discussed in more detail later.