Fibrillary Glomerulopathy
Anthony Chang, MD
Key Facts
Clinical Issues
Rare: < 1% of native kidney biopsies
Associated with malignancy, dysproteinemia, and autoimmune disease
Proteinuria (100%)
Hematuria (˜ 50%)
40-50% progress to ESRD within 2-4 years
35-50% recur in kidney allografts
Microscopic Pathology
Diffuse mesangial expansion by eosinophilic material
Congo red negative
Several histologic patterns
Mesangial proliferation
Membranoproliferative GN
Crescents ˜ 25%
Segmental &/or global glomerular scarring
IF: IgG and C3 in mesangium and along GBM
Usually IgG4, rarely IgM and IgA
Usually kappa = lambda
EM: Nonbranching, randomly arranged fibrils
Thicker than amyloid
Average: 20 nm; range: 10-30 nm
Top Differential Diagnoses
Amyloidosis
Immunotactoid glomerulopathy
Cryoglobulinemic glomerulonephritis
Fibronectin glomerulopathy
Diagnostic Checklist
IgG, kappa and lambda light chains strongly positive
TERMINOLOGY
Synonyms
Fibrillary glomerulonephritis (FGN)
Nonamyloidotic fibrillary glomerulopathy
Congo red negative amyloidosis-like glomerulopathy
Definitions
Glomerular disease characterized by nonamyloid, nonperiodic fibrillar deposits of immunoglobulin, 10-30 nm in diameter
ETIOLOGY/PATHOGENESIS
Unknown
Fibrils contain IgG, usually IgG4 ± IgG1, with both light chains (polyclonal)
Occasional cases monotypic light chains (10-20%)
Most cases idiopathic
Associations
Malignancy (23%)
Dysproteinemia (17%)
Autoimmune disease (15%), including systemic lupus erythematosus
Infection, including hepatitis C virus (3%)
CLINICAL ISSUES
Epidemiology
Incidence
< 1% of native kidney biopsies
Age
Average: ˜ 50 years; range: 19-81 years
Gender
Slight female predilection
Ethnicity
Caucasian predilection (> 90%)
Presentation
Proteinuria (100%)
Nephrotic (38%)
Hematuria (52%)
Hypertension (70%)
Renal insufficiency
Laboratory Tests
Normocomplementemic (97%)
Treatment
Drugs
None effective, corticosteroids if acute inflammation
Prognosis
40-50% progress to ESRD in 2-4 years
Occasional complete (5%) or partial (8%) remission
Recurrence rate of 35-50% in kidney allografts
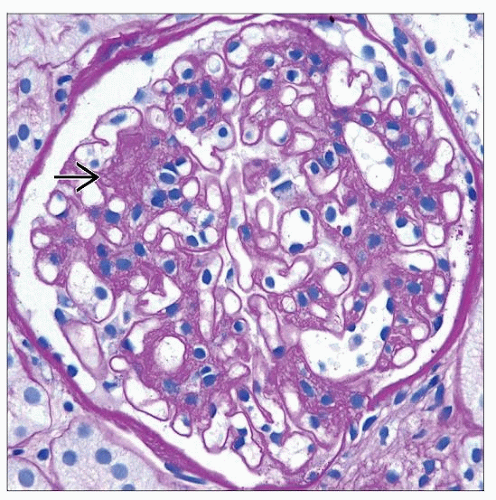
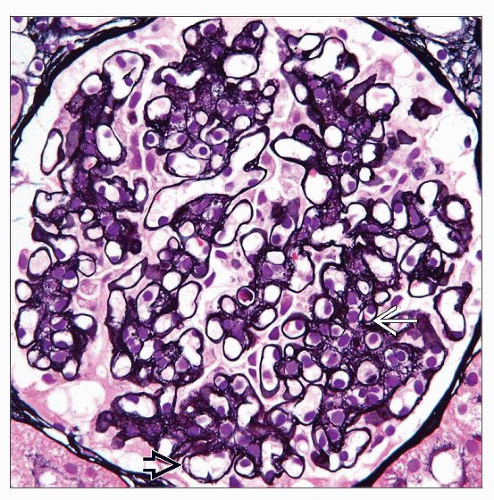
MICROSCOPIC PATHOLOGY
Histologic Features
Glomeruli
Diffuse mesangial expansion by eosinophilic material
Mesangial sclerosis &/or hypercellularity pattern
Can manifest as nodular glomerulosclerosis
Segmental &/or global glomerular scarring
Membranoproliferative pattern
Focal GBM duplication
Marked subepithelial deposits may mimic membranous GN
Cellular crescents in ˜ 25% of cases
Usually < 20% of glomeruli
Congo red stain negative
PAS and Jones silver stain negative (or weak)
Tubules and interstitium
Interstitial fibrosis and tubular atrophy common
Interstitial inflammation may be prominent when tubular basement membrane deposits present
ANCILLARY TESTS
Immunofluorescence
Prominent IgG deposits in mesangium and along GBM
Often IgG4 (90%) with (80%) or without (10%) IgG1; rarely IgG1 alone (10%)
IgG4 heavy chains spontaneously reassociate, impairing detection of monotypic light chains
Kappa = lambda in most cases
10-20% monotypic light chains (70% lambda)
May mimic anti-GBM disease or MGN
C3 almost always strongly positive (92%), often lesser C1q (60%)
May have IgM (47%) or IgA (28%) but at a lesser intensity than IgG
TBM deposits of IgG in a subset
Electron Microscopy
Randomly arranged fibrils deposited in mesangial areas and along GBM
Fibrils without hollow core or organized substructure
Average diameter: 18-20 nm; range: 10-30 nm
Resemble amyloid fibrils but usually larger diameter
Fibrils composed of immunoglobulins by immunogold labeling
TBM has fibrillar deposits in subset of cases
DIFFERENTIAL DIAGNOSIS
Amyloidosis
Congo red positive with apple-green birefringence under polarized light; 8-12 nm thick fibrils
Immunotactoid Glomerulopathy
Microtubular substructure of deposits larger (30-50 nm thick fibrils)
Often associated with underlying plasma cell dyscrasia
Usually (˜ 80%) monotypic
Cryoglobulinemic Glomerulonephritis
Serum cryoglobulins present
Membranoproliferative pattern of injury with “pseudothrombi” on light microscopy
Strong IgM, not IgG4 dominant
Fibronectin Glomerulopathy
Mesangial and subendothelial deposition of PAS(+) material
Negative immunofluorescence staining
DIAGNOSTIC CHECKLIST
Pathologic Interpretation Pearls
Pathologic predictor of poor outcome
Global glomerulosclerosis
SELECTED REFERENCES
1. Nasr SH et al: Fibrillary glomerulonephritis: a report of 66 cases from a single institution. Clin J Am Soc Nephrol. Epub ahead of print, 2011
2. Alpers CE et al: Fibrillary glomerulonephritis and immunotactoid glomerulopathy. J Am Soc Nephrol. 19(1):34-7, 2008
3. Rosenstock JL et al: Fibrillary and immunotactoid glomerulonephritis: Distinct entities with different clinical and pathologic features. Kidney Int. 63(4):1450-61, 2003
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree