Femoral to Popliteal Bypass
Parth B. Amin
Melhem J. Sharafuddin
A number of conduits have been used to bypass obstructed segments of the femoropopliteal system. Autogenous saphenous vein has the best patency and avoids the potential for prosthetic graft infection. Furthermore, primary assisted patency can be improved substantially with surveillance duplex examination. This chapter will focus on femoropopliteal bypass using saphenous vein as a conduit.
SCORE™, the Surgical Council on Resident Education, classified femoral–popliteal bypass as an “ESSENTIAL UNCOMMON” procedure.
STEPS IN PROCEDURE
Expose greater saphenous vein
Expose common femoral artery from vein harvest incision
Dissect common femoral artery, profunda femoris, and superficial femoral artery
Exposure of suprageniculate popliteal artery
From vein harvest incision, enter popliteal fossa anterior to sartorius
Continue dissection posterior to the femur
Identify the popliteal artery and vein
Divide venous tributaries crossing over the popliteal artery
Exposure of infrageniculate popliteal artery
Approach incision 1 cm posterior to tibia and 2 cm distal to medial femoral condyle
Incise fascia and retract soleus and gastrocnemius to get into popliteal space
Divide crossing veins on top of popliteal artery
Measure length of vein needed for bypass
Divide vein at saphenofemoral junction
Mobilize saphenous vein by dividing branches
Prepare vein using retrograde valvulotome or used reversed vein
Create proximal anastomosis
Tunnel vein subsartorially into popliteal fossa
For infrageniculate bypass, tunnel from suprageniculate to infrageniculate popliteal compartment
Perform distal anastomosis
Doppler evaluation and completion angiogram
HALLMARK ANATOMIC COMPLICATIONS
Bypass graft thrombosis
Lymphocele
Wound breakdown
Saphenous nerve injury
LIST OF STRUCTURES
Inguinal ligament
Pubic tubercle
Anterior superior iliac spine
Femur
Medial femoral condyle
Superficial circumflex iliac artery and vein
Inferior epigastric artery
Superficial external pudendal artery and vein
Inguinal lymph nodes
Femoral sheath
Fascia lata
Common femoral artery
Superficial femoral artery
Profunda femoris artery
Femoral vein
Greater saphenous vein
Femoral nerve
Saphenous nerve
Fossa ovalis
Inguinal lymph nodes
Iliopsoas muscle
Pectineus muscle
Adductor brevis muscle
Adductor longus muscle
Adductor magnus muscle
Adductor tubercle
Adductor canal
Sartorius muscle
Semimembranosus
Semitendinosus muscle
Vastus medialis muscle
Popliteal fossa
Soleus muscle
Gastrocnemius muscle
Exposure of Saphenous Vein
The greater saphenous vein is superficial and medial to the common femoral artery (see Chapters 130 and 131 for discussion of the anatomy of this vein). A preoperative saphenous vein marking using ultrasound may help reduce complications from skin flaps and also diagram larger tributaries. The greater saphenous vein is the largest vascular structure in the superficial fascia and essentially overlies the proximal femoral vein. In its course in the upper thigh, it lies between two layers of superficial fascia and is, therefore, not as obvious as it is in the lower leg. In addition to receiving the small tributaries mentioned earlier, typically, one or more larger tributaries draining the thigh or communicating with the lesser saphenous vein also drain into the greater saphenous vein.
Place the patient supine on the operating table with the thigh mildly externally rotated, flexed, and elevated at the level of the knee joint. Expose the vein first to assure adequate conduit for bypass. Use either a long continuous incision or several interrupted incisions along the course of the greater saphenous vein to perform an in situ bypass. Minimize handling of the edges of the skin incision and avoid making the skin flaps too thin. Skin flaps that are thin or traumatized with forceps, especially in patients with ischemia or occlusive vascular disease, usually result in wound problems. Complications such as wound infections, sloughing of skin flap edges, or sloughing of the skin flap (particularly the posterior flap) often arise in such cases. A gentle, meticulous technique is therefore critical when creating the skin flaps.
Once adequate length has been exposed, attention is then turned to arterial exposure. The proximal and distal arterial vessels are exposed and sites of anastomoses decided upon. After measuring this distance, a slightly longer segment of saphenous vein is harvested. The saphenous vein can be used in a reversed fashion particularly if there is no substantial size mismatch between the ends of the vein, and the respective arterial segment to which anastomosis will be performed. A nonreversed vein can be used as well for concerns regarding size mismatch. Valvulotome usage is described after proximal and distal arterial exposure.
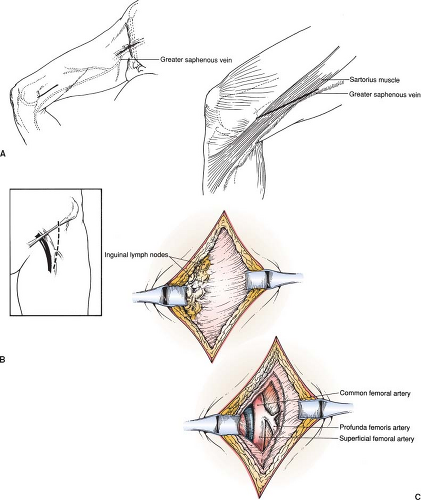
Sites of Groin Incision (Fig. 133.1)
Technical Points
Palpate the inguinal ligament and identify the pubic tubercle and anterosuperior iliac spine. Often, a short flap can be created, such that exposure of the common femoral artery can be obtained using the saphenous vein harvest site. If this is not feasible, place a longitudinal skin incision centered over the femoral artery. This skin incision should extend from 1 to 2 cm above the inguinal ligament to about 10 cm below the inguinal ligament. If separate incisions are used, the saphenous vein harvest incision should be started distally to the inferior most aspect of the femoral artery exposure. Often, there is substantial disease in the mid-to-distal common femoral artery. More proximal exposure can be obtained by retraction of the inguinal ligament cephalad, or by simply dividing a portion of the inguinal ligament. Care must be taken when dissecting at the junction of the external iliac and common femoral arteries as two major collateral branches, the superficial circumflex iliac artery and the inferior epigastric artery. Furthermore, the circumflex iliac veins are often seen crossing transversely under the inguinal ligament. Dissection here must be taken with great care as exposure can be limited.
The profunda femoris artery usually takes off from the common femoral artery about 1 to 3 cm distal to the inguinal ligament. The skin incision must, therefore, extend above the inguinal ligament to expose the common femoral artery adequately. If the incision or dissection is below the usual anatomic bifurcation of the common femoral artery, only the superficial femoral artery will be seen. The profunda femoris artery can also be used as a source of inflow, and so exposure of this vessel can be paramount. Suitable exposure of the profunda femoris as an inflow vessel most often requires division of the later circumflex femoral vein, which crosses the artery in a transverse manner. Once divided, care must be taken to avoid injuring smaller branches. Two larger branches off the profunda femoris, the medial and lateral circumflex femoral arteries, serve as important collaterals for patients with severe ischemia. These two collaterals can often arise directly off the common femoral artery and care should be taken to look for this variation.
Several lymph nodes will be found anterior to the femoral artery in the femoral canal. Be careful to avoid injury to the lymphatic channels and lymph nodes in this area. Disruption of the lymphatic system can result in lymphocele formation and wound problems. Dissect the common femoral, profunda femoris, and superficial femoral arteries gently. A small venous branch courses over the profunda femoris artery. If necessary, ligate and divide this vein to allow access to the profunda femoris distal to its first perforating branch. Obtain proximal control of the common femoral artery and distal control of both the superficial femoral and profunda femoris arteries using Silastic loops.
Anatomic Points
The common femoral artery is the most lateral structure in the femoral sheath. It reliably bisects the inguinal ligament. This relationship can be used to locate the femoral artery, even when occlusive disease prevents location of a palpable pulse. The femoral nerve lies immediately lateral to the femoral artery, whereas the femoral vein is immediately medial to the artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree