Extraanatomic Bypass
Gregory J. Landry
Gregory L. Moneta
Introduction
Extraanatomic bypasses include femorofemoral, axillofemoral, and axillobifemoral bypasses. Freeman and Leeds performed the first extraanatomic bypass in 1952 using an endarterectomized superficial femoral artery tunneled subcutaneously to the contralateral femoral artery. Vetto reported the first femorofemoral bypass in 1962. The first axillofemoral bypasses for lower extremity ischemia were independently reported by Blaisdell and Louw in 1963. Sauvage and Wood reported the first axillobifemoral bypass for bilateral lower extremity ischemia in 1966. Although extraanatomic bypass has largely been regarded as a second-choice alternative to standard aortoiliac and aortofemoral reconstruction and has been replaced to a large degree by percutaneous endoluminal interventions in appropriate patients, it remains a reliable and durable option for lower extremity revascularization that should remain in the armamentarium of physicians performing vascular surgery.
Extraanatomic bypass has traditionally been reserved for the treatment of symptomatic aortoiliac occlusive disease in patients with severe systemic illness increasing operative risk and in patients with local factors increasing the risk or difficulty of standard aortofemoral reconstruction. Examples of such local factors include prior aortoiliac procedures, prior radiation, extensive intra-abdominal adhesions, severe aortic calcification, abdominal malignancy, intra-abdominal infection, aortic or aortic graft infection, colostomy or ileostomy, and enterocutaneous fistula. While infrequently used, endovascular aortouniiliac repair of abdominal aortic aneurysms has resulted in an additional indication for femorofemoral bypasses. While many, if not most, aortoiliac revascularizations are now performed with percutaneous endoluminal therapy, extraanatomic bypass remains a viable alternative in patients whose extent of disease is too great for percutaneous treatment. Femorofemoral or unilateral axillofemoral bypass is indicated for unilateral aortoiliac occlusive disease, with axillobifemoral bypass indicated for bilateral disease.
Patients with aortoiliac occlusive disease of sufficient severity to warrant extraanatomic bypass grafting typically have absent or weak femoral pulses. Noninvasive vascular examination of the lower extremities is helpful in documenting the severity of ischemia and level of distal disease. Computed tomography (CT), magnetic resonance (MR), or digital subtraction arteriography is routinely performed for elective cases but often is not essential in urgent or emergent cases. Unilateral iliac artery angioplasty and stenting can occasionally be performed to facilitate femorofemoral bypass.
The adequacy of axillary inflow can be determined noninvasively in most cases. Segmental pressure measurements and Doppler analog waveforms are obtained at the level of the radial, ulnar, and brachial arteries in both arms. A pressure difference greater than 15 mm Hg between arms indicates significant occlusive disease. Upper extremity arteriography is performed when abnormalities are detected by noninvasive testing. Subclavian artery angioplasty with or without stenting is performed when indicated to improve axillary artery inflow. The right axillary artery is preferred for the axillary anastomosis, since the left subclavian artery has a higher reported incidence of developing atherosclerotic occlusive disease.
Prophylactic antibiotics, usually a first-generation cephalosporin, are administered immediately prior to surgery and continued for 24 hours. Aspirin therapy (325 mg/d) is started preoperatively and continued indefinitely postoperatively. Patients with an identified hypercoagulable state or a history of multiple graft failures are treated with long-term warfarin anticoagulation.
Technical Considerations
Anesthesia
General anesthesia with endotracheal intubation is preferred. Femorofemoral bypasses can be performed with spinal or epidural anesthesia in high-risk cases. Monitored local anesthesia can be used for axillofemoral bypasses, although tunneling of the grafts requires supplemental sedation.
Patient Positioning
Patients are placed in the supine position. For axillofemoral bypasses the donor arm is abducted 90 degrees. This position maximizes the distance between the axillary and femoral arteries, thereby minimizing tension on the axillary anastomosis postoperatively. The femoral regions are widely prepped and draped for femorofemoral bypasses, and the supra- and infraclavicular regions, axilla, chest, abdomen, for axillofemoral bypasses. To minimize operative time, a multiple team approach is preferred if possible, with separate surgical teams operating simultaneously at each of the operative sites.
Femoral Artery Dissection
The femoral arteries are exposed through bilateral vertical groin incisions. The common femoral artery just prior to the common femoral bifurcation is the preferred site for the distal anastomosis; however, the choice of site for the distal anastomosis is based upon angiographic findings and patient circumstances. Accordingly, the distal graft anastomoses may be to the common, deep, or superficial femoral arteries. Occasionally, endarterectomy of the outflow vessels may be required. In special circumstances, distal anastomoses may be to more distal portions of the deep or superficial femoral arteries, and lateral approaches to these vessels may be used, especially in the presence of infection of previously placed femoral grafts.
Axillary Artery Dissection
The axillary artery is defined anatomically by the first rib proximally and the teres major muscle distally. It is convenient to define the parts of the artery by their relationship to the pectoralis minor muscle. The first, second, and third parts of the artery are medial to, posterior to, and lateral to the pectoralis minor muscle, respectively. There is one named branch, the supreme thoracic artery, arising from the first part of the axillary artery. Two branches (thoracoacromial and lateral thoracic arteries) emanate from the second part, and three (subscapular and medial and lateral humeral circumflex arteries) from the third part of the axillary artery. The axillary vein runs parallel to the course of the axillary artery and lies anterior and inferior to it. The brachial plexus nerves interdigitate with the axillary artery and its branches. The first part of the artery lies anterior to the brachial plexus. The divisions and cords of the brachial plexus lie anterior to the third part of the artery. The second part of the axillary artery is enveloped by the brachial plexus cords passing from posterior to anterior.
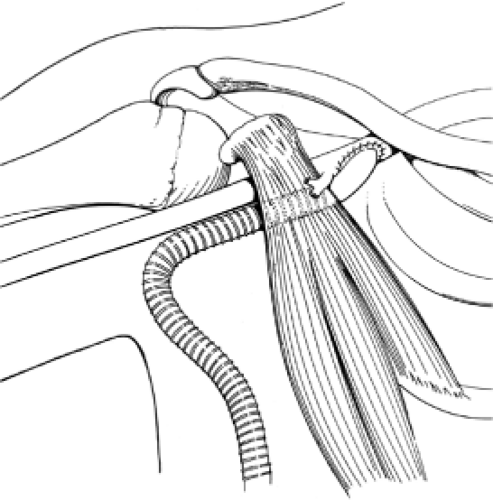
These anatomic relationships point out the advantages of using the first part of the axillary artery for the proximal anastomosis. It is relatively fixed in position, is anterior to the brachial plexus, and has only a single collateral branch. An incision paralleling the course of the axillary artery is made approximately two fingerbreadths below the middle third of the clavicle. The fibers of the pectoralis major muscle are then bluntly separated, revealing the clavipectoral fascia, which is incised.
The pectoralis minor muscle is mobilized but not divided and serves as the lateral border of the dissection. The axillary vein is mobilized and retracted caudally to reveal the axillary artery, a step that requires ligation and division of the cephalic vein and other small venous branches along the cephalad portion of the vein. The thoracoacromial artery is left intact and used as the marker for the lateral corner of the anastomosis. Sufficient length of artery is dissected and mobilized medial to the thoracoacromial artery for the proximal anastomosis.
Femorofemoral Tunnel
A subcutaneous, suprapubic, inverted U tunnel is created between the two femoral incisions using a long, curved aortic clamp. The tunnel lies directly anterior to the external oblique and anterior rectus fascia. By placing the tunnel directly on top of the fascia and avoiding placement of the tunnel in the suprapubic fat, motion of the graft with positional changes and kinking in the groin area is minimized, which is particularly important in obese patients with a large suprapubic pannus. An externally supported PTFE graft (8 mm × 40 cm) is used. An externally supported PTFE graft (8 mm × 40 cm) is used.
Axillofemoral Tunnel
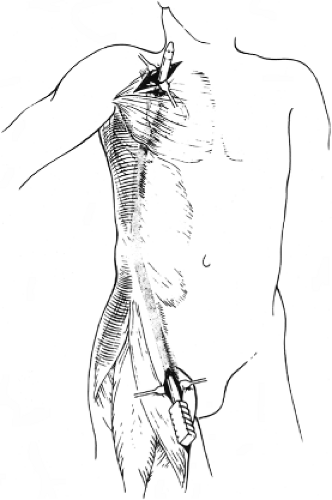
A subcutaneous tunnel is begun at the ipsilateral femoral incision. The standard tunnel passes medial to the anterior superior iliac spine and then along the lateral aspect of the abdomen in the midaxillary line. The tunnel continues posterior to the pectoralis major and minor muscles into the axilla (Fig. 1). The use of the Oregon tunneler or a similar tunneling device allows the tunnel to be made without the need for counterincisions in all but unusually tall patients. An externally supported polytetrafluoroethylene PTFE graft (8 mm × 70 to 90 cm) is passed through the subcutaneous tunnel.
Graft Anastomoses
Femorofemoral Bypass
After completion of the tunnels, intravenous heparin is administered at a dose of 100 U/kg. The arteries are controlled proximally and distally with atraumatic vascular clamps or Silastic vessel loops. Bilateral end-to-side anastomoses are created to femoral arteriotomies with CV-5 or CV-6 PTFE suture. The arteriotomies are 2.5 times the diameter of the graft in length. The anastomosis to the inflow artery is preferentially to the common femoral artery. The anastomosis to the outflow artery depends on the patency of the outflow vessels. If the superficial and profunda femoral arteries are patent, the anastomosis can be placed on the common femoral artery. If the superficial femoral artery is occluded, as is often the case in patients with advanced atherosclerosis, the distal anastomosis can still be placed on the common femoral artery if the
origin to the profunda femoral artery is widely patent, or the anastomosis can be extended across the profunda origin or placed on the profunda itself.
origin to the profunda femoral artery is widely patent, or the anastomosis can be extended across the profunda origin or placed on the profunda itself.
The graft is spatulated to create a “cobra-head” anastomosis. Sutures are placed in the heal and toe of the anastomosis and are run continuously out of each corner. Alternatively, a single suture can be placed in the heal and sewn circumferentially. The graft and vessel edges are everted, with suture bites approximately 1mm in depth and travel between bites. The arteries are flushed and backbled prior to completion of the anastomosis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree