Essential Thrombocythemia
Kaaren K. Reichard, MD
Key Facts
Terminology
Clonal hematopoietic myeloproliferative neoplasm
Proliferation largely restricted to megakaryocytic lineage
Clinical Issues
Vascular disturbances in 50% of individuals
Microscopic Pathology
Peripheral blood
Variable thrombocytosis but ≥ 450 × 109/L
No leukoerythroblastosis
No significant left shift in the granulocytic series
Circulating blasts unusual
Red and white blood cell morphology unremarkable
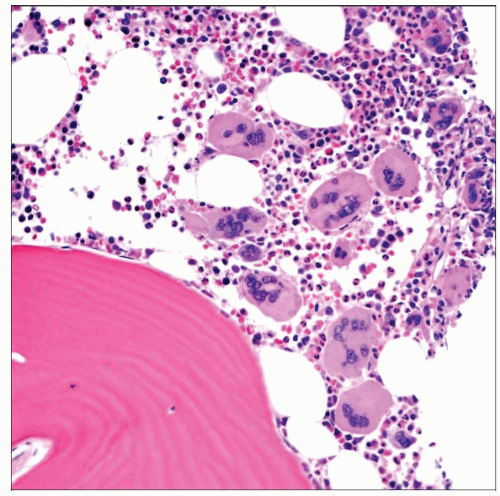
Bone marrow
Normal cellularity to mildly hypercellular
Blasts < 5%
Striking megakaryocytic proliferation
Absent/minimal reticulin fibrosis
Ancillary Tests
Cytogenetics typically normal
∽ 50% of cases with JAK2 V617F mutation
Top Differential Diagnoses
Reactive thrombocytosis
Numerous causes
Cause is usually clinically apparent
BM examination not required
BCR-ABL1-negative MPNs
CML with thrombocytosis
BCR-ABL1 fusion present
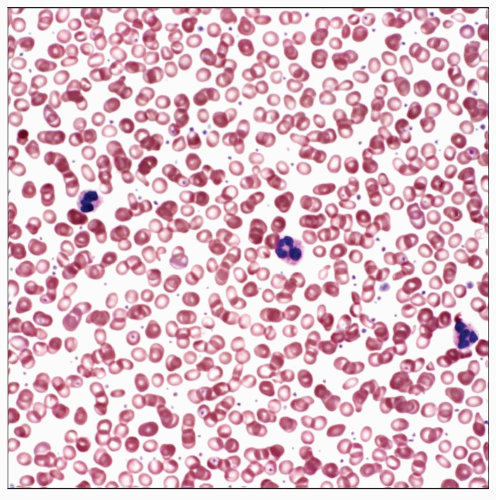 This PB smear shows the typical appearance of ET: Thrombocytosis with unremarkable neutrophil and red blood cell morphology. Reactive thrombocytoses often exhibit a similar appearance. |
TERMINOLOGY
Abbreviations
Essential thrombocythemia (ET)
Synonyms
Essential thrombocytosis
Primary thrombocytosis
Primary thrombocythemia
Definitions
Clonal hematopoietic myeloproliferative neoplasm (MPN)
Proliferation largely restricted to megakaryocytic lineage
Sustained thrombocytosis ≥ 450 × 109/L
ETIOLOGY/PATHOGENESIS
Molecular Pathogenesis
Approximately 50% of cases harbor the JAK2 V617F activating mutation
Approximately 4% of cases harbor an MPL mutation
Exclusion of BCR-ABL1(+) disease
Familial ET
Rare
Incidence of JAK2 mutation lower than in sporadic ET
Incidence of thrombosis lower than in sporadic ET
Activating MPL mutation thought to be main cause
Spontaneous megakaryocyte formation
Reported 100% 10-year survival
CLINICAL ISSUES
Epidemiology
Incidence
0.6-2.5/100,000 people per year
Age
Typically adults
6th and 7th decades of life
May present in children; exclude familial
Gender
No gender predilection
Site
Peripheral blood (PB), bone marrow (BM)
Presentation
Abnormal complete blood cell count (CBC)
Thrombocytosis
Vascular disturbances in 50% of individuals
Thrombosis
Hemorrhage
Increased risk of miscarriage
Laboratory Tests
CBC with differential
PB and BM examination
Conventional cytogenetics
Molecular studies as needed
JAK2 V617F seen in ˜ 50% of cases
MPL mutations in < 5%
Treatment
Low-dose aspirin, unless contraindicated
Cytoreductive therapy
Aim is to reduce thrombotic complications
Hydroxyurea
Anagrelide
Prognosis
Generally indolent
Predictors of thrombosis
Age > 60 years
Prior history of thrombosis
Acute leukemia transformation
Poor prognosis
Rare event
MICROSCOPIC PATHOLOGY
Peripheral Blood
Variable thrombocytosis but ≥ 450 × 109/L
Striking platelet anisocytosis
Small and large platelets
Hypogranular forms may be seen
Circulating megakaryocytic nuclei
No leukoerythroblastosis
Neutrophilia may occasionally be observed
No significant left shift in the granulocytic series
No significant basophilia
Circulating blasts unusual
Red blood cell morphology unremarkable
White blood cell morphology unremarkable
Bone Marrow
Normal cellularity to mildly hypercellular
Generally no significant granulocytic or erythroid proliferation
Occasionally may encounter mild granulocytic hyperplasia
Consider early phase of primary myelofibrosis in such cases
Blasts < 5%
Striking megakaryocytic proliferation
Increased numbers
Loosely clustered
Markedly enlarged
ET megakaryocytes are largest of all BM disorders
Hyperlobulated
Mature
May see intrasinusoidal/perisinusoidal distribution
Absent/minimal reticulin fibrosis
Rare lymphoid nodules
Normal iron stores
Unless concurrent iron deficiency
Exclude iron-deficient polycythemia vera
Normal bone
ANCILLARY TESTS
Histochemistry
Reticulin
Absent to minimal fibrosis
Progressive fibrosis in rare cases
Immunohistochemistry
Highlight abnormal megakaryocytic proliferation
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree