Objectives
- Describe the functional anatomy of the esophagus and related structures, and their innervation
- Understand the roles played by the oral cavity, pharyngeal structures, and esophagus in transferring food from the mouth to the stomach during swallowing
- Discuss how the contents of the respiratory and digestive systems are kept separate
- Define the mechanisms and functions of primary and secondary esophageal peristalsis
- Discuss how the contents of the respiratory and digestive systems are kept separate
- Describe the roles played by the upper and lower esophageal sphincters in esophageal motility
- Understand how the relaxation of these structures is coordinated with the swallow
- Describe how the lower esophageal sphincter protects against reflux of gastric contents
- Understand how belching occurs
- Understand how the relaxation of these structures is coordinated with the swallow
- Discuss disease states in which esophageal motility and/or swallowing are abnormal
Basic Principles of Esophageal Motility
 The esophagus is a muscular tube that serves to transfer food from the mouth to the stomach. Under normal circumstances, food resides in the esophagus for only a few seconds and thus there is no time for it to be acted upon by any esophageal secretions. Thus, an understanding of the physiology of the esophagus relates primarily to its motility functions. In addition to moving the food along its length in the process of swallowing, the movements of the esophagus and related oral and pharyngeal structures must be carefully regulated to avoid misdirection of the food into the respiratory tract, or respired air into the digestive system. At rest, the esophagus is a relaxed structure that is closed off at both ends by sphincters—the upper and lower esophageal sphincters, respectively. These sphincters not only cooperate in the act of swallowing, or deglutition, but also prevent backflow of gastric contents into the esophageal lumen or oral cavity. However, under specific circumstances, the esophagus does allow for retrograde movement. This occurs normally for air swallowed with the meal, in the process of belching, or abnormally during vomiting. During retrograde movement in humans and most mammals, the esophagus itself is a passive conduit; that is, there are no specific motility functions that propel vomitus or air along the length of the tube. Note that the process of vomiting will be discussed in detail in Chapter 8.
The esophagus is a muscular tube that serves to transfer food from the mouth to the stomach. Under normal circumstances, food resides in the esophagus for only a few seconds and thus there is no time for it to be acted upon by any esophageal secretions. Thus, an understanding of the physiology of the esophagus relates primarily to its motility functions. In addition to moving the food along its length in the process of swallowing, the movements of the esophagus and related oral and pharyngeal structures must be carefully regulated to avoid misdirection of the food into the respiratory tract, or respired air into the digestive system. At rest, the esophagus is a relaxed structure that is closed off at both ends by sphincters—the upper and lower esophageal sphincters, respectively. These sphincters not only cooperate in the act of swallowing, or deglutition, but also prevent backflow of gastric contents into the esophageal lumen or oral cavity. However, under specific circumstances, the esophagus does allow for retrograde movement. This occurs normally for air swallowed with the meal, in the process of belching, or abnormally during vomiting. During retrograde movement in humans and most mammals, the esophagus itself is a passive conduit; that is, there are no specific motility functions that propel vomitus or air along the length of the tube. Note that the process of vomiting will be discussed in detail in Chapter 8.
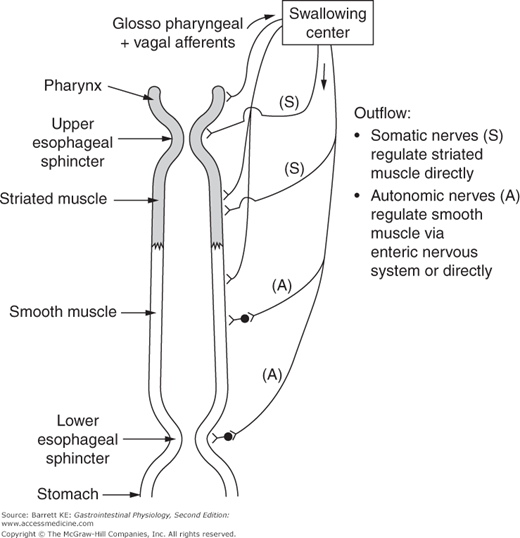
 The process of swallowing, as well as other esophageal motility functions, is under close regulatory control. Swallowing can be initiated voluntarily, but thereafter reflects an automatic reflex that involves, sequentially, impulses from the brainstem, processing of this information through vagal centers in the central nervous system, direct effects of parasympathetic vagal efferents on esophageal muscle layers, and relay of information via the enteric nervous system (Figure 7–1). Movement of materials along the length of the esophagus is aided by gravity, but predominantly depends on a coordinated series of muscle contractions and relaxations that make up the propulsive motility pattern known as peristalsis.
The process of swallowing, as well as other esophageal motility functions, is under close regulatory control. Swallowing can be initiated voluntarily, but thereafter reflects an automatic reflex that involves, sequentially, impulses from the brainstem, processing of this information through vagal centers in the central nervous system, direct effects of parasympathetic vagal efferents on esophageal muscle layers, and relay of information via the enteric nervous system (Figure 7–1). Movement of materials along the length of the esophagus is aided by gravity, but predominantly depends on a coordinated series of muscle contractions and relaxations that make up the propulsive motility pattern known as peristalsis.
Functional Anatomy of the Esophageal Musculature
The esophagus is a muscular tube, 18–25 cm long in adult humans, with its length varying with the total body height. Like the remainder of the gastrointestinal tract, it is surrounded by two muscle layers; the innermost (i.e., closest to the lumen) oriented in a circular fashion and the outer oriented longitudinally. However, unlike the exclusive occurrence of smooth muscle in all more distal segments of the gastrointestinal tract, the esophagus contains striated (or skeletal) muscle in its upper third, both striated and smooth muscle in its middle third, and exclusively smooth muscle in its most distal third. The distinction between muscle types also corresponds approximately to different types of neural control, as discussed later.
 Other structures associated with the esophagus are important in swallowing and normal esophageal function. We have already mentioned the upper and lower esophageal sphincters, which are areas of specialized muscle that occlude both ends of the esophagus at rest. The esophagus is situated within the low-pressure thorax, and thus the presence of these sphincters is important to prevent the entry of air and gastric contents. The pharynx, which connects the nose and mouth to both the esophagus and trachea, is also critically involved in swallowing. The pharynx is traditionally divided into three regions—nasopharynx, oropharynx, and hypopharynx. The nasopharynx is not a part of the alimentary tract, but muscles in this structure contribute to swallowing by preventing the movement of the food bolus into the nasal passages. The oropharynx is responsible for propulsion of the food bolus backward into the esophagus. The hypopharynx, extending from the base of the tongue to the cricoid cartilage, contains the upper esophageal sphincter. In total, the pharynx is critically involved in segregating food and air as they pass through this region.
Other structures associated with the esophagus are important in swallowing and normal esophageal function. We have already mentioned the upper and lower esophageal sphincters, which are areas of specialized muscle that occlude both ends of the esophagus at rest. The esophagus is situated within the low-pressure thorax, and thus the presence of these sphincters is important to prevent the entry of air and gastric contents. The pharynx, which connects the nose and mouth to both the esophagus and trachea, is also critically involved in swallowing. The pharynx is traditionally divided into three regions—nasopharynx, oropharynx, and hypopharynx. The nasopharynx is not a part of the alimentary tract, but muscles in this structure contribute to swallowing by preventing the movement of the food bolus into the nasal passages. The oropharynx is responsible for propulsion of the food bolus backward into the esophagus. The hypopharynx, extending from the base of the tongue to the cricoid cartilage, contains the upper esophageal sphincter. In total, the pharynx is critically involved in segregating food and air as they pass through this region.
The function of the pharynx is controlled by the central nervous system, via outflow from a region known as the central swallowing center (Figure 7–1). The pharynx thereby permits complex coordination of voluntary swallowing with other higher functions, such as respiration and speech. Central input also controls the contractile function of the upper one third of the esophagus, corresponding to the segment of the esophagus that consists of striated muscle. The somatic nerves that innervate these structures have motor end plates that terminate directly on the striated muscle fibers. They originate in brain regions known as the nucleus retrofacialis and the nucleus ambiguus. They release acetylcholine (ACh), which acts on the striated muscle cells via nicotinic receptors.
The smooth muscle of the esophagus is innervated predominantly by the vagus nerve. The vagal efferents synapse with myenteric neurons via ACh and with the smooth muscle directly via ACh and substance P (the former acting via muscarinic receptors). Sensory afferents located in the esophagus likewise project via the vagus to a brain region known as the nucleus tractus solitarius in the dorsal vagal complex. Cell bodies in this region also project to the motor neurons in the nucleus ambiguus, which control a pattern generator for the oral and pharyngeal components of swallowing. This neural circuitry ensures that control of the muscle groups involved in deglutition is linked to the function of more distal regions of the esophagus, as well as to the regulation of opening of the lower esophageal sphincter.
The esophagus is also richly supplied with enteric neurons. These clearly contribute to both sensing the presence and nature of esophageal contents, and coordinating local reflexes that supplement central control of swallowing and esophageal peristalsis. This network of enteric neurons can produce secondary peristalsis of the smooth muscle portion of the esophagus even in the absence of vagal input.
Features of Esophageal Motility
The motility functions consist sequentially of the movement of food from the mouth into the esophagus itself, propulsion along the length of the esophagus via the process of peristalsis, and relaxation of the lower esophageal sphincter to permit entry of the food bolus into the stomach. In health, these components of deglutition are tightly integrated, but for simplicity we will consider each in turn here.
Although the term swallowing can refer to the entire process required to move food from the mouth to stomach, here we will consider it to include only those motility events that move the bolus beyond the upper esophageal sphincter, as well as their regulatory controls. As noted earlier, swallowing is initiated when we sense that food particles in the mouth have been reduced in size sufficiently to permit their passage into the esophagus. While we consider this to be a voluntary response, during its course it in fact becomes an involuntary reflex involving significant input from a pattern-recognition center in the brainstem. This recognizes a food bolus as suitable for swallowing and generates the required neuromuscular response. However, it is possible to override this recognition system voluntarily, such as in the case of swallowing a pill or capsule. But in either case, the subsequent events that contribute to swallowing are entirely involuntary.
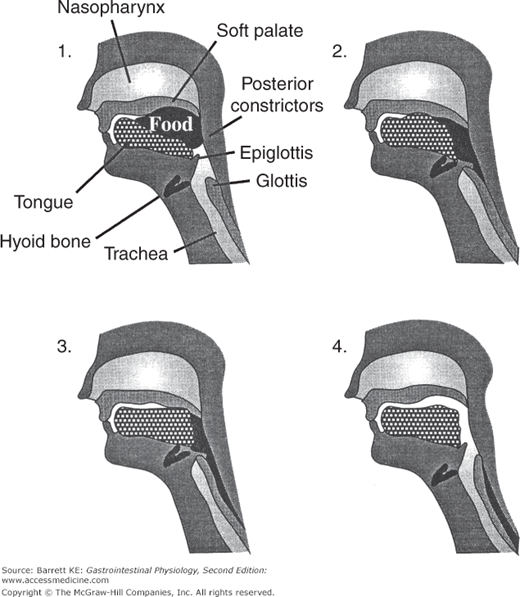
 First, the tongue shapes and lubricates the bolus and moves it backward in the mouth. Subsequently, a rapid series of pharyngeal effects occur, initiated by mucosal mechanoreceptors in the pharynx that activate afferent nerves traveling through the glossopharyngeal nerve to the swallowing center. In turn, efferent motor nerves run through the vagi to control the contractile state of the pharyngeal muscles. The sequence of contractions that ensues has been observed in experimental subjects by fluoroscopic (X-ray image) analysis. Such studies have shown the events to occur almost simultaneously, which contrasts to the slower motility changes that occur more distally in the esophagus, as will be discussed later. First, the larynx and soft palate move upwards, closing off the airway and nasopharynx, respectively. Next, contraction of several muscles in the anterior portion of the pharynx causes forward displacement of the larynx and pharynx as well as helping to open the upper esophageal sphincter. Sphincter opening also depends on relaxation of the encircling cricopharyngeal muscle. This is accomplished by a suppression of impulses normally occurring to this region, coordinated by the swallowing center via the nucleus ambiguus. Longitudinal contractions of the pharynx also bring the upper esophageal sphincter close to the base of the tongue, whereupon a pressure gradient developed by the tongue and pharyngeal muscles serve to force the bolus through the sphincter. Finally, the posterior wall of the pharynx contracts in a transverse fashion to clear the area of any remaining food residues. These transverse contractions are propagated aborally (i.e., in the direction away from the mouth) and can be considered the harbinger of the peristaltic wave that later will carry the bolus through the esophagus and down into the stomach. The sequence of events involved in normal swallowing is shown diagrammatically in Figure 7–2.
First, the tongue shapes and lubricates the bolus and moves it backward in the mouth. Subsequently, a rapid series of pharyngeal effects occur, initiated by mucosal mechanoreceptors in the pharynx that activate afferent nerves traveling through the glossopharyngeal nerve to the swallowing center. In turn, efferent motor nerves run through the vagi to control the contractile state of the pharyngeal muscles. The sequence of contractions that ensues has been observed in experimental subjects by fluoroscopic (X-ray image) analysis. Such studies have shown the events to occur almost simultaneously, which contrasts to the slower motility changes that occur more distally in the esophagus, as will be discussed later. First, the larynx and soft palate move upwards, closing off the airway and nasopharynx, respectively. Next, contraction of several muscles in the anterior portion of the pharynx causes forward displacement of the larynx and pharynx as well as helping to open the upper esophageal sphincter. Sphincter opening also depends on relaxation of the encircling cricopharyngeal muscle. This is accomplished by a suppression of impulses normally occurring to this region, coordinated by the swallowing center via the nucleus ambiguus. Longitudinal contractions of the pharynx also bring the upper esophageal sphincter close to the base of the tongue, whereupon a pressure gradient developed by the tongue and pharyngeal muscles serve to force the bolus through the sphincter. Finally, the posterior wall of the pharynx contracts in a transverse fashion to clear the area of any remaining food residues. These transverse contractions are propagated aborally (i.e., in the direction away from the mouth) and can be considered the harbinger of the peristaltic wave that later will carry the bolus through the esophagus and down into the stomach. The sequence of events involved in normal swallowing is shown diagrammatically in Figure 7–2.
Figure 7–2.
Stages involved in swallowing. 1. The tongue moves the bolus backward and the soft palate moves upwards to close off the nasopharynx. 2. The posterior tongue continues to move the bolus backward. 3. The upper pharyngeal muscle contracts at the posterior wall of the pharynx, forcing the bolus down into the pharyngeal channel away from the nasopharynx. The distal pharynx relaxes to receive the bolus, the upper esophageal sphincter relaxes, and the trachea is closed off by movement of the glottis. 4. As the bolus moves into the esophagus, the various structures return to their resting positions. (From Chang EB, Sitrin MD, Black DD. Gastrointestinal, Hepatobiliary and Nutritional Physiology. Philadelphia: Lippincott-Raven; 1996:37.)
The nerves that innervate the muscular structures of the pharynx and upper esophageal sphincter release ACh, which causes muscle contraction via binding to nicotinic receptors. Although these nerves accompany the vagus anatomically, functionally they are somatic motor nerves that terminate directly at motor end plates on the striated muscle of this region. This should be contrasted with the autonomic nerves that control the function of the smooth muscle in the more distal segment of the esophagus.