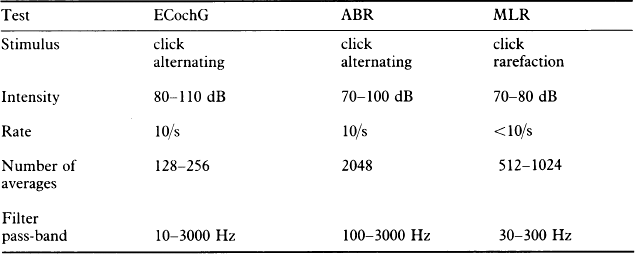
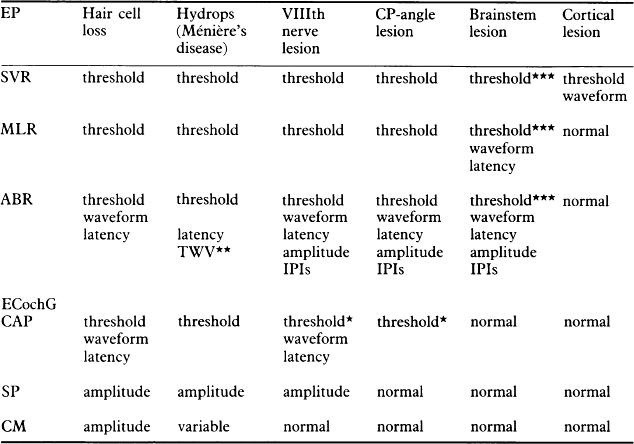
15 The ERA tests are valuable in differentiating cochlear from retrocochlear hearing loss, confirming lesions, and detecting unsuspected retrocochlear pathology (Robinson & Rudge 1983). The more common problems referred to neuro-otologists which may require ERA testing are listed below: The testing strategies depend on the clinical symptomatology and suspected site of lesion. Of all ERA tests, ABR is the most suitable test for this purpose. MLR and ECochG may contribute to establishing the site of the lesion in a specific situation; however, each test on its own is less valuable than in combination. Table 15.1 shows the effect of various pathologies on the EPs. Table 15.1 EP parameters alterable by various pathologies *with involvement of the end-organ and/or intracapalicular tumours **TWV = Travelling wave velocity ABR measures (see p. 110) ***Unilateral lesions do not cause threshold changes unless the generator of the response, used to estimate threshold is affected by the lesion. Bilateral or large-midline lesions can cause threshold changes in all responses rostral to the lesion. Standardization of ERA test procedures for neuro-otological strategies is desirable. This is especially relevant for ABR, which is the most important diagnostic tool, and the clinician has to rely on specific diagnostic parameters. ERA tests and recommended parameters for neuro-otological testing are shown in Table 15.2. ECochG is used in neuro-otological testing in order to establish the latency of the potential generated at the cochlear nerve site. It becomes especially helpful when wave I of ABR cannot be recorded in cases of moderate and severe hearing losses. The waveform of the compound action potential and SP reflect the pathophysiologic status in the cochlear, and clearest responses are obtained at high intensity click stimuli. However, some investigators found this test on its own of little use in acoustic tumour detection, or in differentiating between cochlear and retrocochlear pathologies. Testing conditions, stimulus intensities, repetition rate, and polarity are the same as for ABR, but the recording band-pass filters are not the same. For ECochG, a broader band-pass filter of 10–3000 Hz is used. When ABR is used for neuro-otological testing, the aim is to obtain clearly defined peaks of the waves, so that the latencies can be measured accurately. For CNS lesions, useful diagnostic information may be obtained from a comparison of both ipsilateral and contralateral (to the side of stimulation) ABRs. Hence, bilateral recordings should be used routinely. Monaural stimulation is used and the results compared with the normative data. However, if the other ear is not affected, it may act as a partial control for age and sex. Stimuli at a rate of approximately 10/s do not affect the latencies and waveform of ABR; therefore, a rate of 10/s is used in a standard neuro-otological test procedure. At higher repetition rates, especially in the presence of high frequency hearing loss, the components of the ABR degrade, wave I in particular, and, hence, compromise the measurement of inter-peak intervals. The auditory system may be stressed by stimulating at higher rates of 50–70/s, and this may elicit more subtle abnormalities. Abnormal responses may suggest a retrocochlear disorder (Shanon et al 1981, Pratt et al 1981). Employing alternating polarity clicks seems to be a rational way of testing, because electrical polarity does not always correspond to acoustic polarity at the eardrum (Salt 1982). In the presence of steep high frequency hearing loss, the latency differences between stimulation with condensation and rarefaction clicks may be considerable (see p. 93). Differentiation of cochlear from retrocochlear lesions relies mainly on ABR. A large proportion of neuro-otologic patients have mild or normal hearing on the pure-tone audiogram. The useful diagnostic parameters for detecting and interpreting abnormal ABRs are listed in Table 15.3. Table 15.3 An interaural latency difference of greater than 0.3 ms is considered abnormal, providing there is no evidence of hearing loss due to middle ear pathology. The inter-peak intervals are independent of conductive hearing loss, and separation into I–III and III–V intervals can sometimes suggest a lesion in the lower or upper brainstem. The MLR can provide additional information, as it has been reported that there is abnormal wave morphology in some patients with multiple sclerosis (Robinson & Rudge 1980). A patient with unilateral or asymmetric sensorineural hearing loss should be suspected of acoustic tumour unless the history is clearly associated with trauma or acute infection. The suspect group includes patients with sudden onset of symptoms and those whose initial presentation is suggestive of Ménière’s disease. Shaia & Sheehy (1976) reported a 0.8% tumour occurrence in 1220 cases of sudden unilateral hearing loss, but only 15–17% of tumours present with this symptom (Meyerhoff 1981, Morrison 1975). This situation requires screening tests by which patients can be selected for elaborate or invasive procedures. In acoustic tumour, auditory symptoms are the first to develop in most cases, and, therefore, hearing evaluation should initiate the screening programme.
ERA in neuro-otologic diagnosis
CLINICAL PROBLEM
CHOICE OF ERA TESTS
INTERPRETATION OF ERA TESTS
ABR
MLR
ECochG
Abnormal waveform
Abnormal waves
Abnormal AP
Latency of wave V (LV)
L–I function
Interaural latency difference (IT 5)
A–I function
Inter-peak interval (IPI I–V)
SP/AP ratio
Interaural difference of I–V intervals
Amplitude ratio V/I
INVESTIGATION OF UNILATERAL HEARING LOSS
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Basicmedical Key
Fastest Basicmedical Insight Engine