(1)
Department of Pathology, Radboud University Nijmegen Medical Center, Nijmegen, The Netherlands
Keywords
JawNeoplasmsOdontogenic tumors3.1 Introduction
Odontogenic tumors encompass a group of lesions that share a common origin from odontogenic tissues. They may arise from the epithelial part of the tooth germ, the mesenchymal part or from both. In this Chapter, those exclusively composed of odontogenic epithelium will be dealt with. They supposedly are derived from the epithelium that plays a role in tooth development by differentiating into ameloblasts that form the tooth enamel and by inducing mesenchymal cells to differentiate into dentin forming odontoblasts. As this epithelium does not disappear after tooth formation, it may serve as a source of tumor cells even at old age.
3.2 Ameloblastoma
Ameloblastoma, the most common odontogenic tumor [1], closely resembles the epithelial part of the tooth germ: ameloblastomas may be locally aggressive, but do not metastasise. They may occur at any age, but cases in the first decade are rare and most of them are diagnosed between the ages of 30–60 years. Mostly, the mandible is involved. In the less often seen maxillary cases, the tumor may grow into the paranasal sinuses to attain a considerable size without causing any external deformity. Radiographically, ameloblastoma is a radiolucent lesion that usually is multilocular, the so-called soap bubble appearance, or unilocular with scalloped outlines (Fig. 3.1) [2]. Macroscopically, the tumors may be solid as well as cystic but mostly, both appearances occur together in a single lesion (Fig. 3.2). By microscopy, ameloblastomas basically consist of either anastomosing epithelial strands and fields or discrete epithelial islands. The former pattern is referred to as plexiform type, the latter as follicular type (Figs. 3.3 and 3.4); both morphologies may occur within one and the same lesion [1]. The peripheral cells at the border with the adjacent fibrous stroma are columnar with nuclei usually in the apical halve of the cell body away from the basement membrane; they resemble the epithelial cells in the tooth germ that lie at the border with the dental mesenchyme (Fig. 3.5). The cells lying more centrally are fusiform to polyhedral and loosely connected to each other through cytoplasmic extensions (Fig. 3.6); they resemble the cells of the so-called stellate reticulum, another part of the tooth germ (Fig. 3.5). In the follicular type, an increase in intercellular edema may lead to cyst formation and these cysts may coalesce to form the large cavities that are responsible for the multicystic gross appearance that ameloblastomas may show (Fig. 3.7). Cyst formation may also occur in the plexiform type ameloblastoma but there, it usually is the result of stromal degeneration which means that strictly spoken, they are not cysts as they lack an epithelial lining (Fig. 3.8). At the interface between epithelium and stroma, condensation of stromal collagen may cause juxtaepithelial eosinophilic hyaline bands (Fig. 3.9). This should not be misinterpreted as dysplastic dentin as present in mixed odontogenic tumors (discussed in Chap. 5) although it seems that the possibility that ameloblastomas occasionally may show deposition of genuine dentin cannot be ruled out completely in view of some recent reports on tumors provisionally labelled as adenoid ameloblastoma with dentinoid (Fig. 3.10) [3–5]. Furthermore, there may be juxtaepithelial areas of focal myxomatous stromal degeneration that should not be confused with the myxocellular tissue that is found in mixed odontogenic tumors and forms a neoplastic tissue component of those lesions (Fig. 3.11). Mitotic figures may occur within the peripheral columnar as well as in the stellate reticulum like cells (Fig. 3.12). In the absence of concomitant cytonuclear atypia and with a normal configuration, they lack prognostic significance.


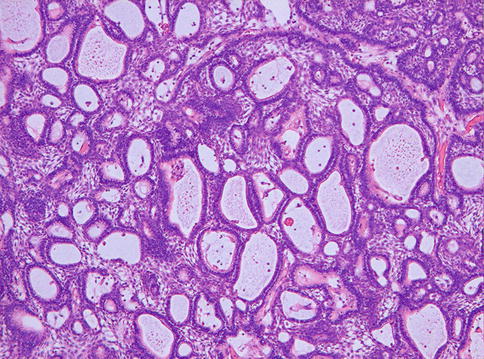
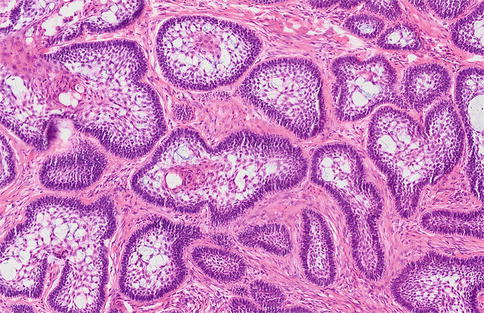
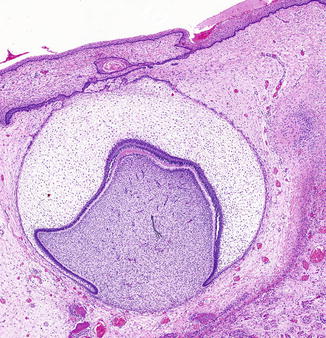
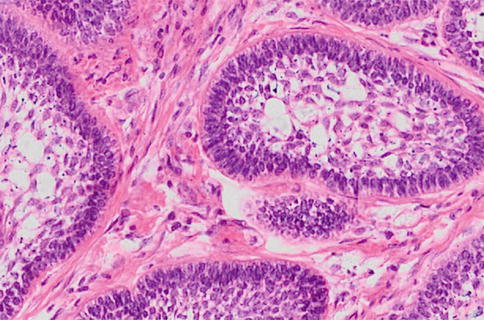
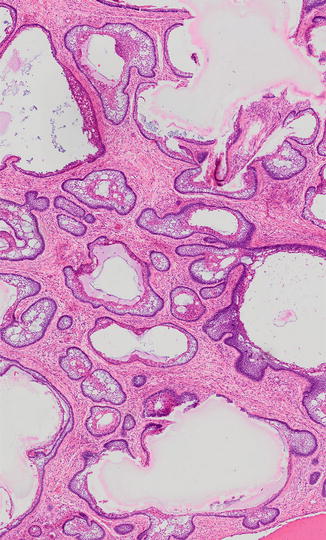
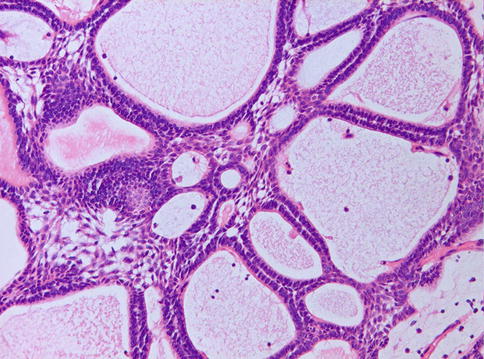
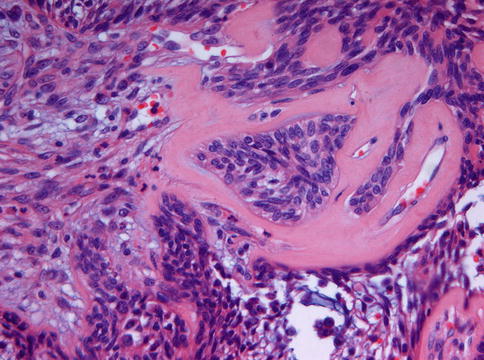
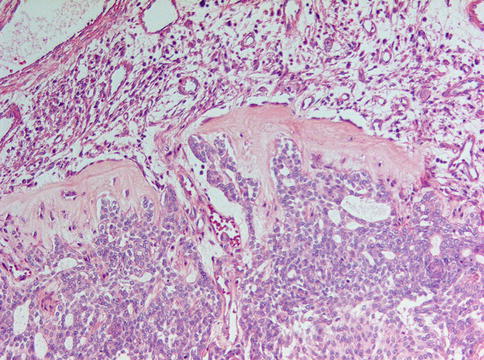
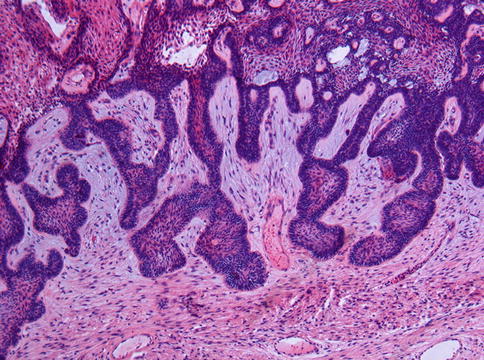
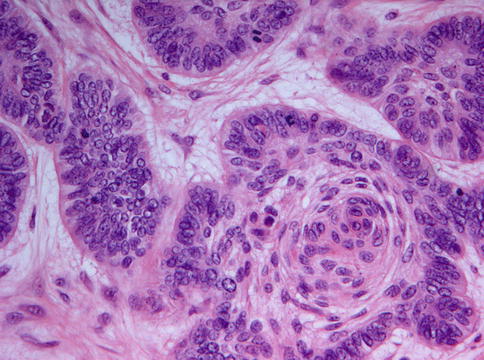

Fig. 3.1
Radiograph of ameloblastoma showing swelling and bone loss in the left mandibular ramus. The soap bubble appearance is typical for this tumor

Fig. 3.2
Gross appearance of mandibular ameloblastoma showing both cystic and solid areas
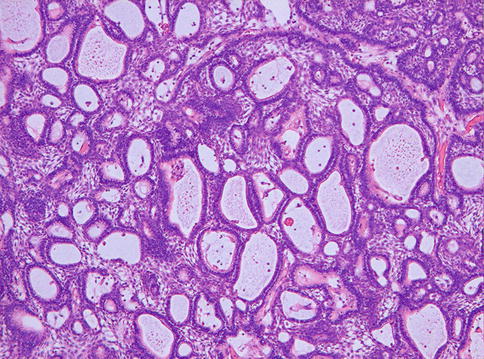
Fig. 3.3
Ameloblastoma with plexiform growth pattern as shown by anastomosing epithelial strands enlarging to more extended epithelial areas. Stroma is a minor component
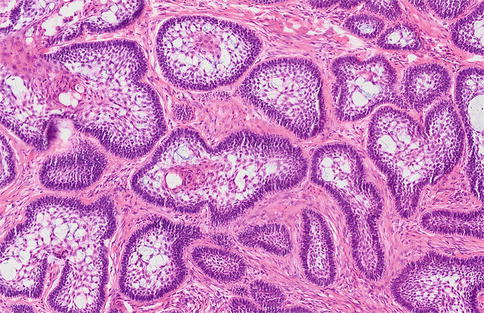
Fig. 3.4
Ameloblastoma with follicular growth. Epithelial islands lying in a fibrous stroma
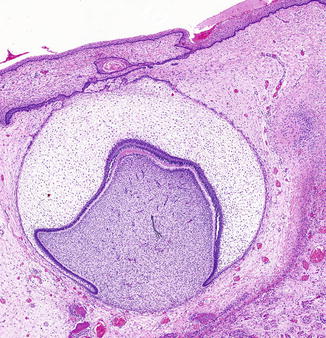
Fig. 3.5
Immature tooth germ. The resemblance of the enamel organ to the epithelial islands in follicular ameloblastoma is obvious
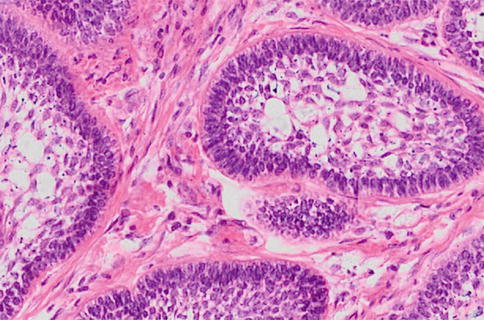
Fig. 3.6
In ameloblastoma, the cells adjacent to the stroma are columnar; those more centrally placed are spindle-shaped and loosely connected to each other, thus creating a resemblance to the enamel organ involved in odontogenesis
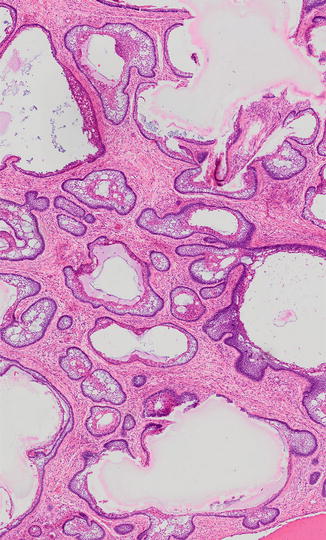
Fig. 3.7
In follicular ameloblastoma, cysts arise through liquefaction in the epithelial islands
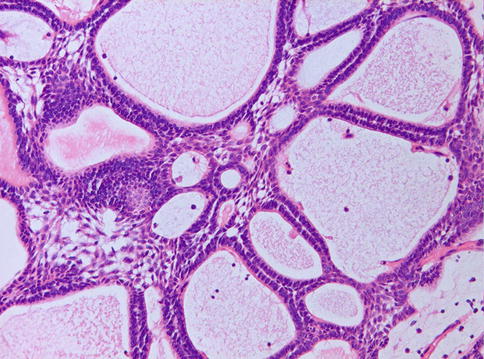
Fig. 3.8
In plexiform ameloblastoma, fluid-filled cavities are not genuine cysts but due to pseudocystic stromal liquefaction
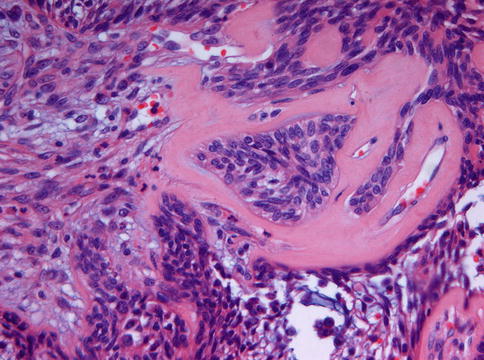
Fig. 3.9
In the juxta-epithelial stroma, a dense hyaline band can be seen. This should not be mistaken for dysplastic dentin as occurs in mixed odontogenic tumors
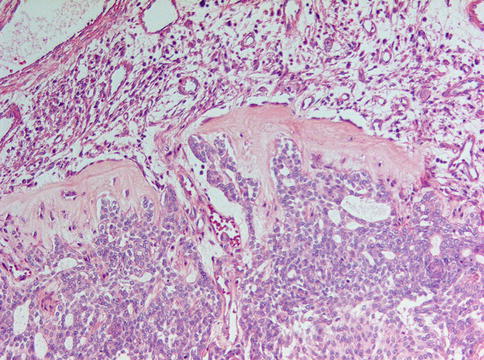
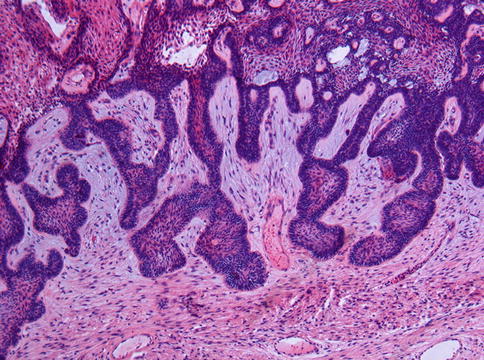
Fig. 3.11
Occasionally, the stromal component in ameloblastoma may show myxomatous changes not to be confused with the primitive odontogenic mesenchyme typically for mixed odontogenic tumors
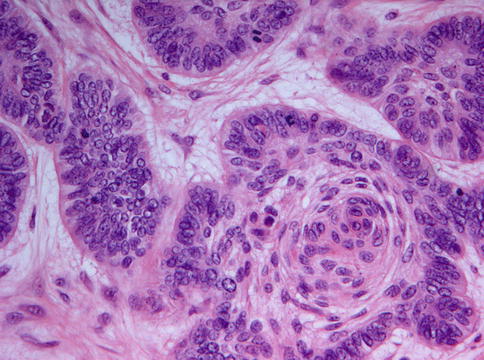
Fig. 3.12
Mitotic activity may occur in ameloblastoma but in the absence of cytonuclear atypia, it does not bear any ominous significance
The involvement of adjacent tissues by ameloblastoma is site-dependent. In the bone marrow, the tumor infiltrates the adjacent cancellous bone (Fig. 3.13). In contrast, the cortical bone of the mandible expands through remodeling and perforation of the cortical plate is exceptional; when occurring, the periosteum still forms a barrier (Fig. 3.14) [6]. Consequently, spread into the adjacent soft tissues is highly unusual and, when observed, one should consider the possibility of an intraosseous malignant tumor, probably an ameloblastic carcinoma. In the maxilla, the tumor may grow through the covering mucosa, thus showing an ulcerating oral muosal surface (Fig. 3.15); in the mandible, the tumor will remain entirely intraosseous and submucosal (Fig. 3.16).
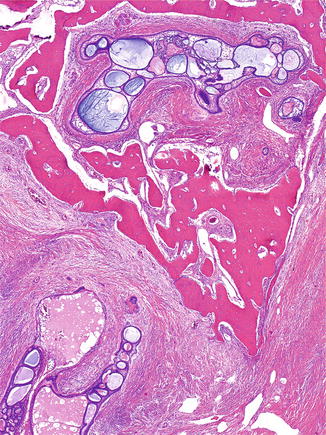
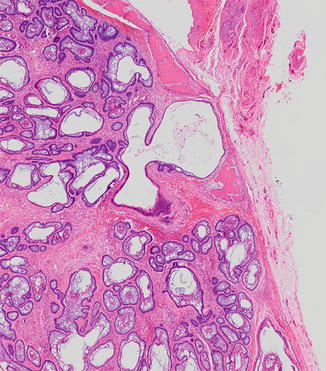
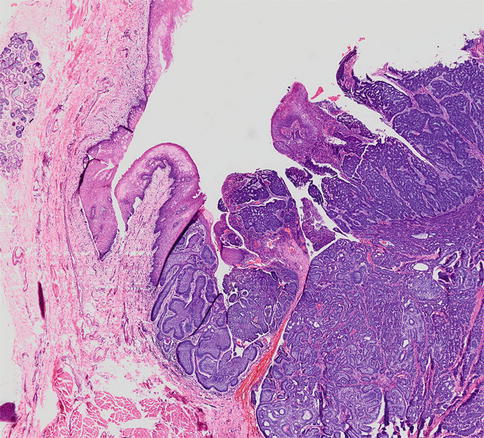
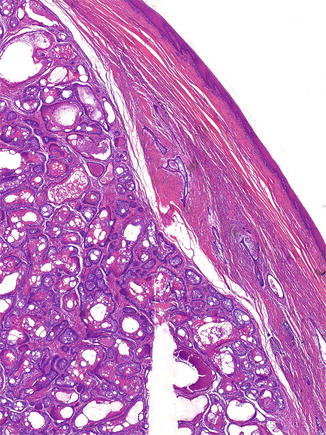
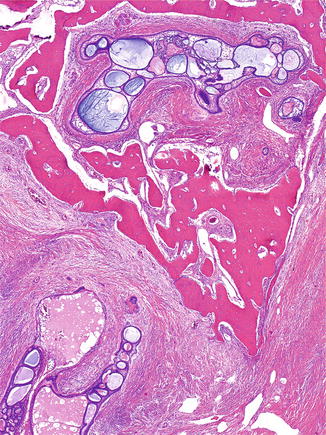
Fig. 3.13
Low power view of ameloblastoma showing invasion of the cancellous bone
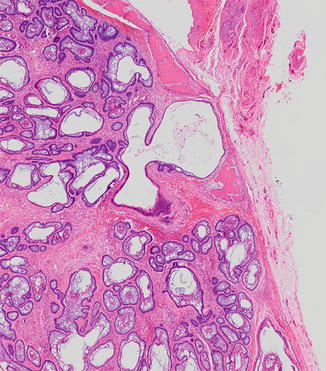
Fig. 3.14
In cases with erosion of the cortical bone, the periosteum still walls of the tumor from the perimandibular soft tissues
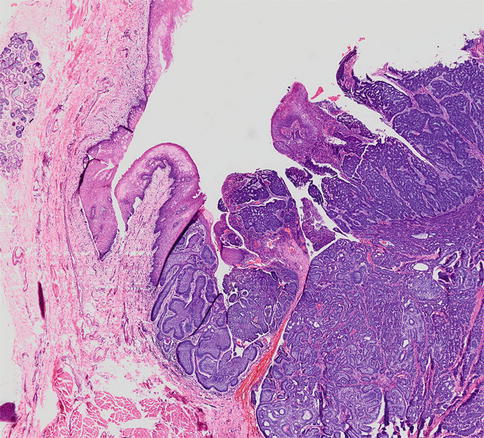
Fig. 3.15
Maxillary ameloblastoma showing mucosal perforation
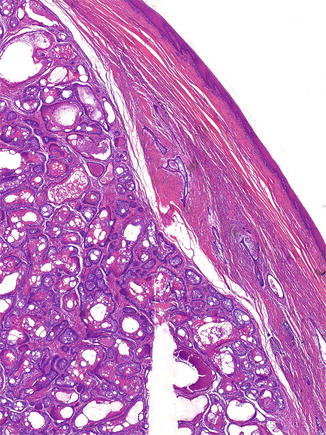
Fig. 3.16
Mandibular cases of ameloblastoma usually remain intraosseous and submucosal
In addition to the two basic subtypes of ameloblastoma, follicular and plexiform, some other histologic variants can be discerned. Acanthomatous and granular cell type ameloblastoma are variants of ameloblastoma with squamous metaplasia (Fig. 3.17) and granular cells respectively (Fig. 3.18). If keratinization is abundant, leading to large cavities filled with keratin, lesions are called keratoameloblastoma (Fig. 3.19) [7]. In these tumors acantholysis may lead to a pseudopapillary lining that characterizes the variant called papilliferous keratoameloblastoma. In the basal cell (basaloid) ameloblastoma the epithelial nests lack an edematous center with cells loosely connected to each other but instead show closely packed basaloid cells, with a peripheral rim of cuboidal cells (Fig. 3.20).
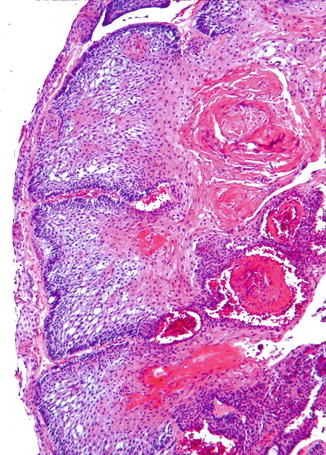
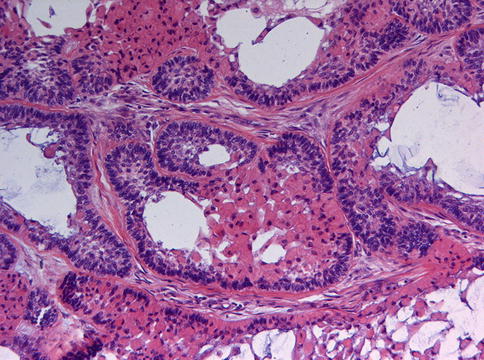
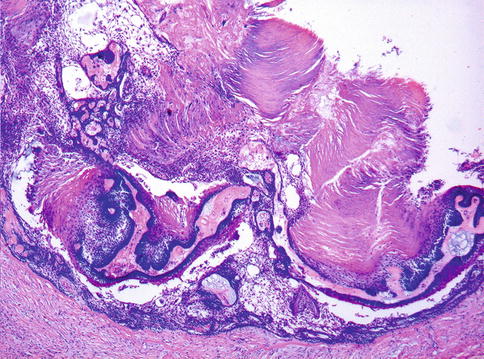
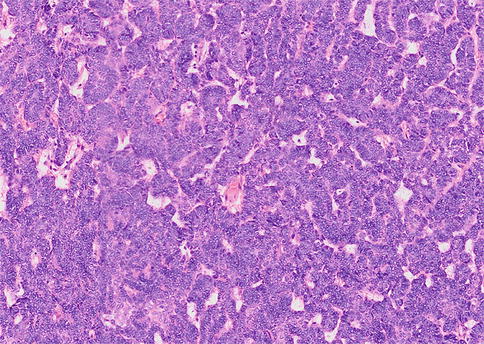
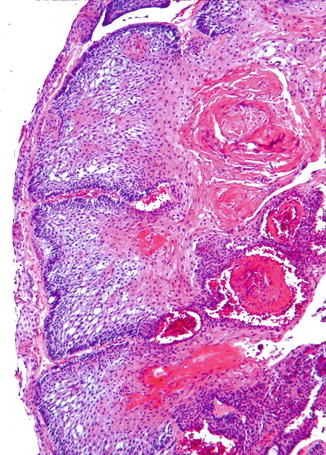
Fig. 3.17
Acanthomatous ameloblastoma showing squamous differentiation
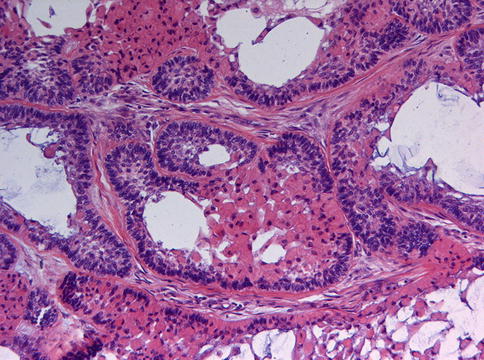
Fig. 3.18
In granular ameloblastoma, the loose central areas are replaced by aggregates of cells with eosinophilic granular cytoplasm
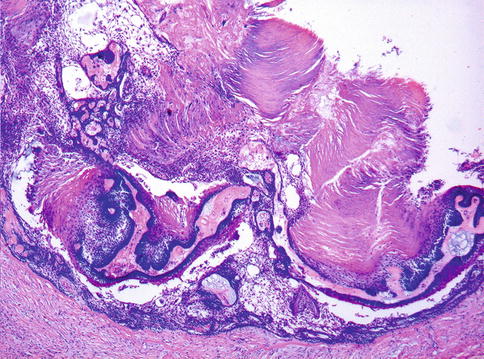
Fig. 3.19
Occasionally, ameloblastomas may show heavy keratinization in their center, a morphological pattern for which the term kerato-ameloblastoma is employed
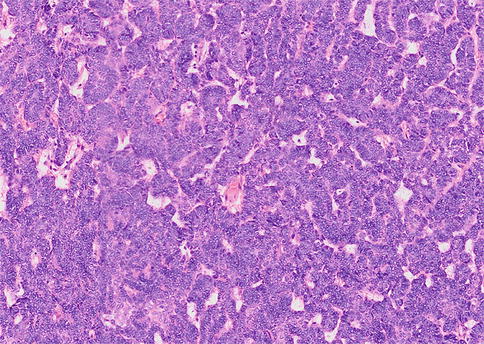
Fig. 3.20
Basaloid ameloblastomas do not show loose edematous areas but instead cell nests composed of closely packed basaloid cells
Tumors with a preponderance of stroma and limited epithelium are called desmoplastic ameloblastoma. Radiologically, they may mimic fibro-osseous lesions as they have a mixed radiodense and radiolucent appearance (Fig. 3.21). They are also clinically and histologically different from the more conventional types both as this type occurs more often in the anterior parts of both maxilla and mandible and shows a dense collagenous stroma, the epithelial component being reduced to narrow, compressed strands of epithelium (Figs. 3.22 and 3.23). When these strands broaden to form larger islands, a peripheral rim of dark staining cuboidal cells and a compact center in which spindle-shaped epithelial cells assume a whorling pattern may be discerned (Fig. 3.24). Within the stromal component, active bone formation can be observed which explains the mixed radiodense radiolucent appearance at the radiographs [8].
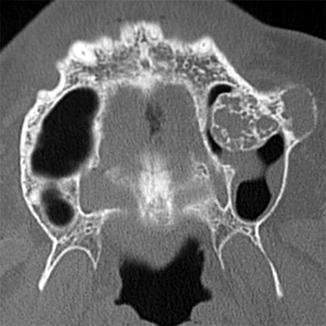

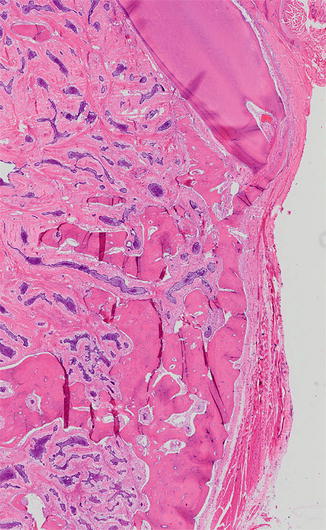
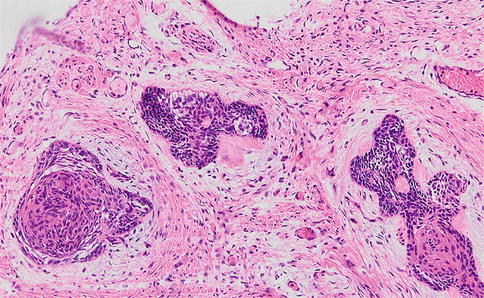
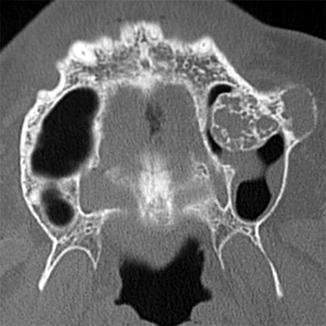
Fig. 3.21
Radiograph of maxillary desmoplastic ameloblastoma. There is expansion of the maxilla both at the buccal side and in the maxillary sinus and the mixed radiodense and radiolucent appearance is clearly seen. This pattern explains why this type of ameloblastoma is often mistaken for a fibro-osseous lesion

Fig. 3.22
Gross appearance of desmoplastic ameloblastoma showing a white-glistening fibrous cut surface. The invasive nature is apparent by the engulfment of the roots of the teeth
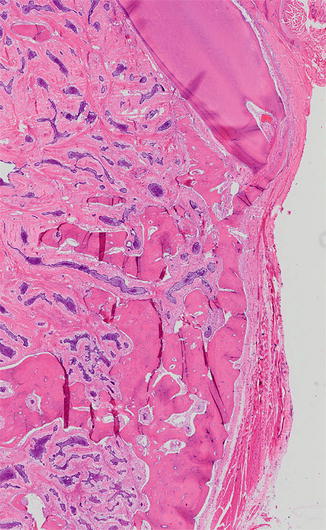
Fig. 3.23
In desmoplastic ameloblastoma, the epithelial component is less predominant than in the other ameloblastoma types. Tiny islands and compressed strands lie dispersed in a dense collagenous stroma
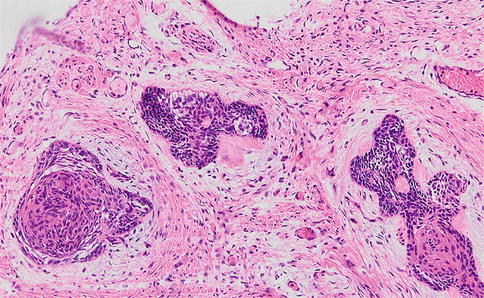
Fig. 3.24
The epithelial islands in desmoplastic ameloblastoma may show a whirling center composed of spindle-shaped cells and peripheral columnar cells may be less conspicuous
Sometimes, ameloblastomas present themselves as a large cyst. This so-called unicystic ameloblastoma occurs at a lower mean age than the other types and may mimic a dentigerous cyst both clinically as well as radiologically because of its occasional association with an impacted tooth (Figs. 3.25 and 3.26) [9]. The lesion consists of a single cystic cavity lined by ameloblastomatous epithelium (Fig. 3.27). This epithelium may proliferate to form intraluminal nodules with an architecture similar to a plexiform ameloblastoma (Fig. 3.28) whereas downward proliferation of this epithelium may lead to infiltration of the fibrous cyst wall by ameloblastoma nests (Fig. 3.29). Sometimes, the cyst lining itself lacks any features indicative of ameloblastoma, these being confined to intramural epithelial nests [10]. Inflammatory alterations may obscure the specific histologic details to such an extent that none are left in which case the lesion may be mistaken for a radicular cyst (Figs. 3.30 and 3.31). However, as already mentioned before when discussing the differential diagnostic issues of the keratocystic odontogenic tumor, radicular cysts are usually small and confined to the periapical area of a decayed tooth whereas both keratocystic odontogenic tumor and unicystic ameloblastoma may occupy large areas of the mandibular body and are not associated with any tooth pathology. In dubious cases, immunohistochemistry may be helpful as ameloblastomas show distinct nucleo-cytoplasmic calretinin immunoreactivity that is particulary intense in the stellate reticulum-like epithelial cells and in areas of squamous metaplasia [11].



Fig. 3.25
Radiograph of a unicystic ameloblastoma involving the right mandibular ramus

Fig. 3.26




Gross specimen of mandibular ameloblastoma presenting itself as a large cyst
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


