Epithelial Cell Inclusions in Lymph Nodes
Definition
Clusters of benign, well-differentiated epithelial cells in lymph nodes.
Pathogenesis
The presence of epithelial cells in lymph nodes is usually the result of metastasis from a regional carcinoma. Their detection is of great clinical importance because it determines the staging, and consequently the treatment, of malignant tumors. Far less often, benign epithelial cells unrelated to the existence of a malignant tumor may also be present in various lymph nodes. Their origin is not well understood, although several theories have been proposed, including transportation of detached epithelial cells as a kind of benign metastasis (1,2,3,4,5), developmental heterotopia (6,7,8,9,10), and metaplasia of local multipotential cells (11,12,13). Because lymph node epithelial inclusions raise different problems of pathogenesis and differential diagnosis, depending on their location and histologic appearance, the various types are discussed separately.
Upper Cervical Lymph Nodes
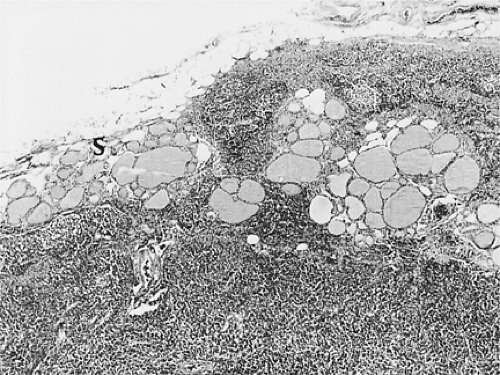
Salivary gland acini and ducts may be found randomly distributed within the upper cervical lymph nodes. They are considered to represent aberrant or heterotopic parotid gland tissue in lymph nodes (6). Ectopic parotid glands or portions thereof are often detected within parotid gland lymph nodes at biopsies performed in the course of inflammatory or neoplastic lymphadenopathies (14,15) (Fig. 54.1) (see Chapter 43).
Lower Cervical Lymph Nodes
Incidental findings of colloid-containing thyroid follicles at radical dissection of the neck for various squamous carcinomas or melanomas of the head and neck have been reported occasionally (16,17,18,19) (Figs. 54.2 and 54.3). None of these was detected grossly, and the incidence was only about 1 in 100 neck dissections (17). When the thyroid glands were later examined histologically, no primary carcinomas were found.
However, Butler and colleagues (18) showed the presence of an occult primary carcinoma of the thyroid in 16 of 22 patients who had thyroid follicles incidentally found in regional cervical lymph nodes. The authors believe that the benign histologic appearance and lack of a papillary component in the thyroid follicles present in cervical lymph nodes do not preclude their being metastatic. Although clinically occult, the primary thyroid carcinoma in the studied cases was found after careful sectioning of the gland, and it usually contained papillary in addition to follicular areas.
Whether thyroid follicles within cervical lymph nodes represent metastases of occult thyroid carcinomas or embryonic malformations has not been resolved, and definitive diagnosis may not be always possible.
Axillary Lymph Nodes
Nodules composed of mammary ducts, cysts, and myoepithelial cells have been observed in axillary lymph nodes (1,20,21). (In Figure 54.4, the breast was the site of fibrocystic disease but not of carcinoma.) More recently, with the introduction of sentinel node biopsy in the diagnosis of breast carcinoma, more cases of epithelial inclusions in axillary lymph nodes have been reported, some of these in the same lymph node with metastatic carcinoma (4,22,23,24). Evidently, this occurrence may be a source of false-positive misdiagnosis leading to inaccurate staging and improper treatment (24). The mechanical transport of breast epithelium to axillary lymph nodes through the intramammary lymphatics was reported in a series of 15 breast carcinoma patients (25). Various reports have been made of epithelial displacement in surgical specimens following needling procedures (26). In a recent
study of 676 patients with invasive breast carcinoma, the incidence of lymph node metastases was greater when the breast carcinoma was diagnosed by large-gauge needle core biopsy or even by fine-needle aspiration than by excisional biopsy (27). In a different study of 56 patients with invasive or in situ nonmetastatic breast carcinoma, benign epithelial inclusions in the axillary lymph nodes occurred more frequently in those patients who underwent breast massage intended to facilitate the localization of sentinel lymph nodes before their biopsy (5).
study of 676 patients with invasive breast carcinoma, the incidence of lymph node metastases was greater when the breast carcinoma was diagnosed by large-gauge needle core biopsy or even by fine-needle aspiration than by excisional biopsy (27). In a different study of 56 patients with invasive or in situ nonmetastatic breast carcinoma, benign epithelial inclusions in the axillary lymph nodes occurred more frequently in those patients who underwent breast massage intended to facilitate the localization of sentinel lymph nodes before their biopsy (5).
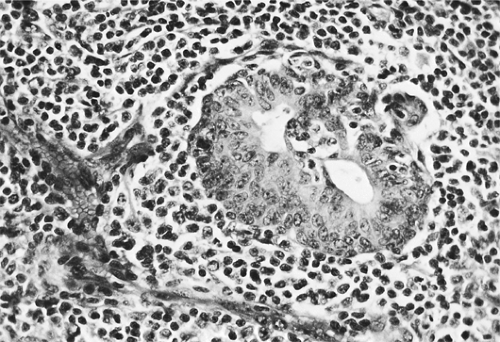 Figure 54.1. Salivary gland inclusion in parotid lymph node. Salivary gland duct with hyperplastic lining epithelium lies within the nodal lymphoid tissue. Hematoxylin, phloxine, and saffron stain. |
Mediastinal Lymph Nodes
Gland-like structures lined by columnar epithelial cells were seen in mediastinal lymph nodes (3,13,28) and were considered
to be of mesothelial origin. Some of these patients had pleuritis with pleural effusions, and the lymph node inclusions were interpreted as pleural cells that had entered lymphatic spaces and been transported to the mediastinal lymph nodes (3,29).
to be of mesothelial origin. Some of these patients had pleuritis with pleural effusions, and the lymph node inclusions were interpreted as pleural cells that had entered lymphatic spaces and been transported to the mediastinal lymph nodes (3,29).
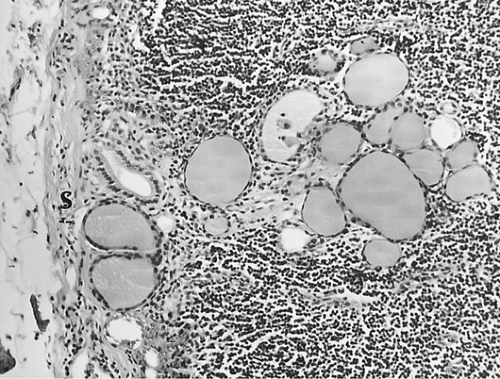 Figure 54.3. Same lymph node as in Fig. 54.2. Nonpapillary, colloid-containing follicles lined by flattened cuboidal epithelium in peripheral sinus (S). × 540. |
Mesenteric Lymph Nodes
Colonic glands of benign histologic appearance were observed in the mesenteric lymph nodes of patients undergoing colectomy for colonic carcinoma (29). The colonic carcinoma was only focal in a villous adenoma, and the glands in the mesenteric lymph nodes appeared benign and were thought to represent embolization caused by the surgical procedure (29).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree