OVERVIEW
- Medically unexplained symptoms (MUS) are common in all fields of medicine
- Many patients have only occasional or mild MUS, but some have either persistent, recurring or changing symptoms
- In addition to the distress they cause to patients, MUS are a public health issue due to their prevalence and associated resource cost
Epidemiology
Symptoms that cannot be adequately explained by disease are common in almost all fields of medicine. The term MUS includes symptoms that are part of a recognised syndrome (such as IBS or fibromyalgia) as well as those symptoms that are not, for instance intermittent palpitations or fatigue of less than 6 months duration.
The prevalence of MUS can be considered at three levels: the general population, GP consulters and patients referred from primary to secondary care.
Population prevalence
Most people will have at least one MUS that is sufficiently severe for them to seek medical advice at some point in their life. In that respect, an occasional symptom not due to disease can be regarded as normal. Between 10 and 20% of adults will have experienced several MUS (more than 4 for men or 6 for women, from a list of 30) over their life course. These epidemiological criteria are sometimes referred to as somatoform disorder or abridged somatisation.
Only around 0.2% of adults have the most severe form of MUS known as somatisation disorder, which is characterised by experiencing, and seeking treatment for, many MUS and starting before the age of 30.
GP consultation prevalence
Estimates of the proportion of patients consulting a GP with MUS vary. A commonly quoted figure is 15%, which is roughly equivalent to one patient per hour of clinic time based on 10 min appointments. Of course, some days it will be less, some days it will feel like much more!
More important than the prevalence of a single MUS in GP clinics is the proportion of patients who repeatedly attend with MUS. This seems to be about 2% of the practice population—and is similar whether one looks at patients who attend repeatedly with MUS over a year or those who are referred to specialists with MUS at least twice over a period of 5 years. Given that these people are relatively frequent consulters, they are likely to account for 4–6% of consultations or one to two patients per day.
Referral prevalence
MUS are common among patients referred to specialists. Table 2.1 shows the proportion of patients referred to six specialties who were deemed by the specialist to have no organic disease. Sometimes referral for MUS is necessary in order to make a diagnosis (for instance see Chapter 13) but in other cases there may be a very low probability of disease and it seems likely that GPs refer some patients for reassurance, either of the patient or themselves.
Table 2.1 Prevalence of medically unexplained symptoms in new referrals to different specialities.
| Speciality | Prevalence (%) |
| Cardiology | 53 |
| Gastroenterology | 58 |
| Gynaecology | 66 |
| Neurology | 62 |
| Respiratory | 41 |
| Rheumatology | 45 |
Prevalence and overlap of syndromes
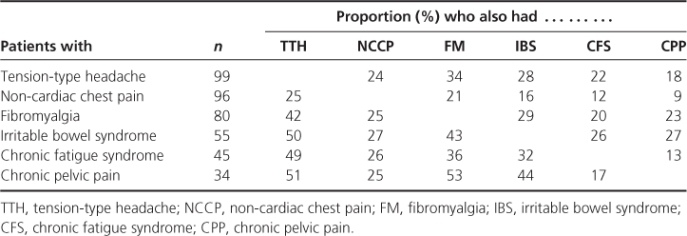
Many patients with MUS meet criteria for a syndrome such as IBS or fibromyalgia. Population surveys demonstrate that these are all fairly common, although most patients with them do not consult their GP. Although the use of syndrome labels encourages us to think about them as discrete entities, it is clear that there is substantial overlap—and that patients with symptoms of one syndrome commonly have additional symptoms of another. This was mentioned in Chapter 1 and is elaborated in Table 2.2, which shows the overlap of a range of functional syndromes among patients referred to one of six specialist clinics.
Table 2.2 Proportion of patients with one functional syndrome who also had another, among hospital outpatient attenders.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


